The 8-minute rule in therapy billing plays a major role. Many billing errors happen because people misunderstand how this rule works. Providers, coders, and billers must understand it to bill correctly and avoid denials.
This simple breakdown explains the rule clearly, so you can use it correctly every day. One unit of a time-based therapy service may be billed only when at least 8 minutes of direct care are provided.
The 8-minute rule is the standard Center for Medicare and Medicaid Services (CMS) method for counting billable units for timed outpatient therapy services.
What Is the 8-Minute Rule in Therapy Billing?
The 8-minute rule explains when therapy time becomes billable. The Centers for Medicare & Medicaid Services created this rule for outpatient therapy services.
The rule applies only to services billed by time, not by visit. A provider must spend at least eight full minutes giving direct care to bill one unit.
If care lasts seven minutes or less, billing is not allowed. This rule helps make sure payment matches the real time spent with the patient.
By setting a clear time limit, the rule prevents overbilling and supports fair claims.
Why Was the 8-Minute Rule Created?
The 8-minute rule was created to keep therapy billing fair and accurate. It stops providers from billing full units for only a few minutes of care.
Without this rule, short treatment times could still lead to full payment. That would cause overbilling and unfair use of healthcare funds.
The rule sets a clear time standard for all providers to follow. This helps claims reflect the real time spent treating each patient.
How Does the 8-Minute Rule Work?
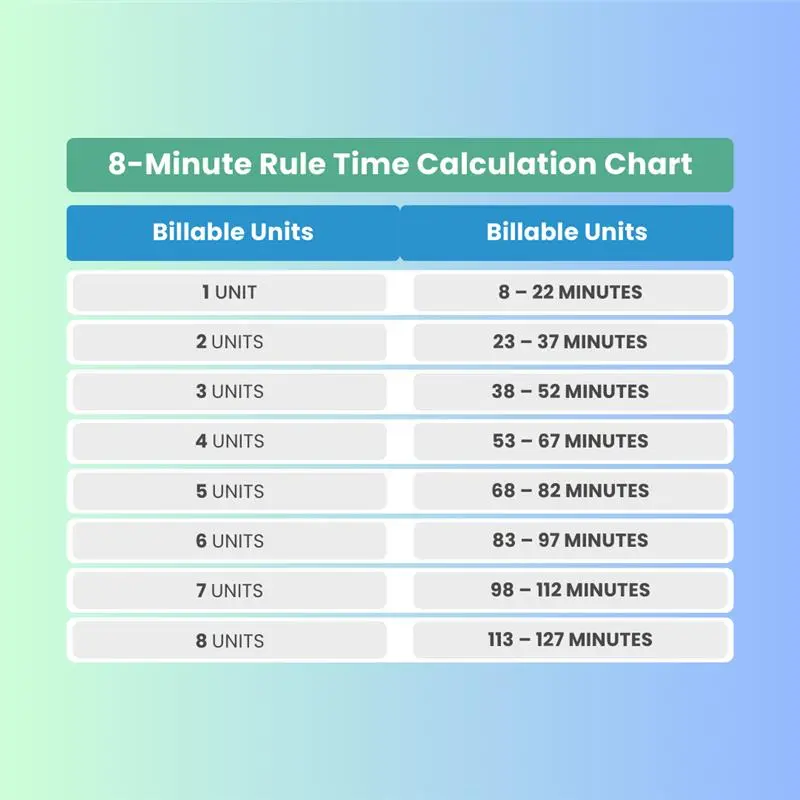
The 8-minute rule decides how many units you can bill for therapy time. You must arrive at least eight minutes before you can bill even one unit.
You do not round time up to fifteen minutes. Instead, you count the total minutes of direct, one-on-one care. As time increases, the number of billable units also increases.
Each unit requires you to cross a set time level before billing more. For example, twenty-two minutes of therapy allows only one unit. Once time reaches twenty-three minutes, you may bill two units.
This method stops billing for short visits. It also makes sure longer sessions receive fair payment.
Does the 8-minute rule apply to all therapy codes?
No. It applies only to time-based therapy codes, not service-based codes.
What Are Time-Based and Service-Based Codes?
Therapy billing uses two main types of codes. Knowing the difference helps you apply the 8-minute rule correctly. The rule applies only to time-based codes. It does not apply to service-based codes.
Time-Based Codes
Time-based codes depend on how many minutes of care you provide. You must count only direct, one-on-one treatment time with the patient. Each unit usually equals fifteen minutes of therapy. The 8-minute rule decides how many units you can bill.
Examples of time-based codes include:
- 97110 for therapeutic exercise
- 97140 for manual therapy
- 97112 for movement and balance training
- 97530 for functional activities
Each code must meet the time rules on its own.
Service-Based Codes
Service-based codes bill once per visit or session. Time does not affect how many units you bill. These services count as completed once performed. The 8-minute rule does not apply to them.
Examples of service-based codes include:
- 97161 to 97163 for therapy evaluations
- 97164 for therapy re-evaluations
- 97010 for hot or cold packs
- 97014 or G0283 for unattended electrical stimulation
Understanding this difference prevents billing errors and denied claims.
Remote Therapeutic Monitoring codes (98975–98981) are increasingly reviewed under time-based billing rules when performed by therapists.
How Is the 8-Minute Rule Different From Other Payer Rules?
Not all payers follow the same time rules for therapy billing. Some use the 8-minute rule, while others follow a different time standard. Knowing which rule applies helps prevent billing errors and claim denials.
The table below shows the key differences between these two rules.
| Rule | Definition | Billing Threshold | Commonly Used By |
|---|---|---|---|
| 8-Minute Rule | CMS guideline that requires at least 8 minutes of a 15-minute timed service to bill 1 unit. | 1 unit = 8–22 minutes (then follow incremental ranges). | Medicare and Medicare Advantage plans |
| AMA Midpoint Rule | Requires at least 50% of the defined time for a CPT code to be billed. Often used by some commercial payers. | 1 unit = ≥ 7.5 minutes of a 15-minute code. | Some commercial/private payers |
Many commercial payers follow the American Medical Association (AMA) Midpoint Rule. Under this rule, each service must reach the midpoint time on its own before billing.
These differences matter when you choose how to bill therapy time. Always follow the rule used by the patient’s insurance plan. Using the wrong rule can lead to denied claims or payment takebacks. Checking payer rules before billing helps keep claims accurate and compliant.
What Are Common 8-Minute Rule Billing Mistakes?
Many billing errors happen when the 8-minute rule gets applied the wrong way. These mistakes can lead to denied claims, lost payment, or audit risk. Below are the most common errors and why they cause problems.
1. Rounding Time the Wrong Way
Some providers round up short treatment times. This causes billing errors under Medicare rules. For example, six minutes of manual therapy is not billable. You must reach at least eight full minutes to bill one unit. Anything less than eight minutes does not count.
2. Misunderstanding Cumulative Time (Medicare Rule)
Under Medicare, timed therapy minutes are added together first. For example, five minutes of exercise and six minutes of manual therapy equal eleven total minutes. That allows billing for one unit. The unit must be billed under the service with the most time.
Example: A therapist provides 10 mins of Manual Therapy (97140) and 14 mins of Therapeutic Exercise (97110).
- Total Timed Minutes: 24 minutes.
- 8-Minute Rule Result: 2 units (23–37 min bracket).
- Billing Tip: You bill 1 unit of 97110 and 1 unit of 97140 because both exceeded 8 minutes and the total reached the 2-unit threshold.
This rule applies only to Medicare. Some commercial payers use different rules.
3. Poor or Vague Documentation
Weak notes create major problems during reviews. Statements like “thirty minutes of therapy” are not enough.
Providers must clearly document:
- Start and end times for each service
- Exact minutes for every billed code
- What treatment was done and how the patient responded
Clear documentation proves services were billed correctly. It also protects providers if claims get reviewed later.
What Documentation Is Required for the 8-Minute Rule?
Clear documentation is required when using the 8-minute rule. Medicare and other payers expect notes that clearly support every billed unit. If time or service details are unclear, payers may deny the claim. Poor notes also increase the risk of audits and payment takebacks.
What to Document
- Start and stop times for each service:
Record the exact time spent on each service. For example, note the start and end times that show total minutes clearly. This helps match the documented time with billed units. - Type of service provided:
Name the exact service performed during treatment. Avoid general terms like “therapy provided.” Clear service names show what care the patient received. - Patient response and progress:
Document how the patient reacted to treatment. Note changes like improved movement, less pain, or better tolerance. This shows that care was needed and effective.
Why Documentation Matters
Good documentation supports correct billing. Auditors compare your notes with the billed units. Clear records reduce claim denials. They also protect providers if payments are reviewed later.
⚡Pro Tip:
Document each service separately when more than one service occurs. Never combine different services under one total time entry.
Why Does the 8-Minute Rule Matter for Compliance?
The 8-minute rule in therapy billing is a required compliance rule. Centers for Medicare & Medicaid Services sets this rule for Medicare therapy services.
When providers apply the rule the wrong way, billing errors occur. These errors can lead to denied claims or payment takebacks.
Over time, repeated mistakes can raise audit risk. Correct use of the rule protects revenue and keeps billing compliant.
For 2026, therapy claims that exceed the $2,480 threshold require the KX modifier. Incorrect use can trigger audits or payment reviews.
How Does the 8-Minute Rule Cause Denials and Repayments?
Errors in the 8-minute rule in therapy billing often lead to denied claims. Payers deny payment when billed units do not match the recorded minutes.
Sometimes payers review claims after payment. If they find a pattern of errors, they may demand money back. These reviews can reach back several years.
Repayment requests can grow large and strain a practice’s finances. Accurate time tracking and clear notes help prevent these losses.
How Does the 8-Minute Rule Increase Audit Risk?
The 8-minute rule in therapy billing is closely monitored by payers. Payers use data tools to spot billing patterns that look unusual.
Billing the highest units often, without strong notes, raises concern. This can trigger focused audits on therapy claims. During audits, reviewers check every billed minute.
If they find mistakes, payers may take further action. These actions can include penalties or loss of payer contracts. Correct billing and clear notes help lower audit risk.
How Does Compliance Protect Therapy Providers?
Correct use of the 8-minute rule in therapy billing protects providers. It starts with tracking time the right way and writing clear notes.
When providers document start and end times, billing stays accurate. Clear service details show what care the patient received.
Strong notes also explain how the patient responded to treatment. This helps prove the care was needed and done correctly.
By following the rule, providers receive proper payment. They also lower audit risk and avoid legal or financial trouble.
Why Is the 8-Minute Rule in Therapy Billing So Important?
The 8-minute rule in therapy billing protects the accuracy of therapy claims. It ensures billing matches the real time spent treating patients.
Providers must know the difference between timed and untimed services. They must also follow the correct time limits for each billed unit.
Clear documentation supports correct billing and proves care was needed. This helps prevent denials and lowers the risk of audits.
In today’s strict billing environment, compliance protects financial health. Using the rule correctly is a daily responsibility for every therapy billing team.