Physical Therapy Modifiers. Small codes. Huge consequences. One letter off, and your claim dies. CMS flags it. The payer rejects it. You lose time, money, and patience. How did billing become such a fight? It’s supposed to be simple. Treat, code, submit, get paid.
But modifiers? They twist that flow. They decide if your care looks clean or confusing. They decide if your payment comes this week or next year. So let’s strip the mystery away. Let’s make modifiers easy and make your payments fast again.
Why Modifiers Matter in Physical Therapy Billing
Ever had two codes trigger a denial? That’s the story of modifiers. They explain what the codes alone can’t. The AMA says modifiers show how services differ even when performed on the same day. They prove your work was distinct, necessary, and part of the care plan. For CMS, modifiers are checkpoints. They confirm your services match policy and medical need.
Without them, your claim looks like a copy of itself. They’re not decoration. They’re the bridge between done and paid. Use them right, and claims glide through. Use them wrong, and you’ll meet the audit team.
The Most Common Physical Therapy Modifiers and What They Mean
You don’t need a dictionary. You just need these five. Five small codes that carry real weight. Five that decide if your claim moves forward or gets stuck. Learn them. Know them cold. Because in billing, mastery isn’t about knowing everything. It’s about knowing what matters most.
| Modifier | Purpose | Example Use |
|---|---|---|
| GP | Services under a PT plan of care | 97110 with GP |
| 59 | Distinct procedural service | 97140 and 97110 performed separately |
| KX | Medical necessity beyond therapy threshold | Used after therapy cap is reached |
| 76 | Repeat procedure by same provider | Repeat modality session |
| 91 | Repeat lab test | Rare in PT but recognized |
Each one tells a story. GP means you’re working inside a therapy plan. 59 means two services were separate, not duplicates. KX means the patient’s reached the cap, but you’ve got proof it’s still necessary. 76 repeats a procedure and tells the payer it’s intentional, not accidental. Get these five right, and you’ve solved most modifier headaches.
How to Decide Which Modifier to Use
So how do you know which one fits? You follow the trail. Always the same path. Start with what you see. Then look deeper. Every code tells part of the story, but the modifier completes it. Miss it, and the payer misunderstands your work. Follow the steps. Read the notes. Let the logic guide you until the pattern feels natural. That’s how accuracy becomes instinct.
1- Is the service part of a therapy plan? Use GP.
2- Are the procedures distinct? Add 59.
3- Has the therapy threshold been hit? Add KX if notes prove necessity.
4- Same procedure, same day, same provider? That’s 76.
5- Unsure? Check the payer’s policy before you send.
That’s it. Five questions. One clean claim. The AAPC calls it the modifier logic chain. Each question connects to compliance. Each answer protects your payment.
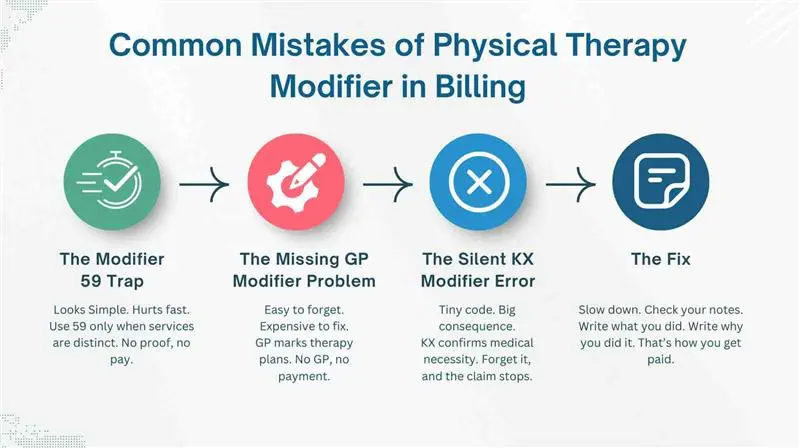
Common Mistakes of Physical Therapy Modifier in Billing
Let’s talk about the traps. Because everyone falls into them. Ever used 59 when 76 was right? Ever skipped GP on a therapy claim? Or hit the cap and forgot KX? The AMA warns that modifier 59 misuse tops the denial charts every year. CMS sees it too. Same mistakes. Same lost money. But it doesn’t have to stay that way.
The Modifier 59 Trap
This one fools everyone. You add 59 thinking it’ll fix the denial. It doesn’t. Why? Because 59 means “distinct service.” It tells payers two procedures were separate. If they weren’t, you’ve just told the wrong story. CMS flags this fast. When you use 59 without proof in your notes, you invite a denial or audit. Always double-check if 76 or another modifier fits better. Accuracy beats habit. Every time.
The Missing GP Modifier Problem
Simple. Common. Costly. Forget GP, and your claim loses its identity. Payers don’t know if the service was part of a therapy plan. Medicare rejects it immediately. The AAPC calls this the number-one “avoidable denial” in physical therapy billing. All you needed was two letters. So ask before sending any claim: Does this fall under a PT plan of care? If yes, it gets GP. Always.
The Silent KX Modifier Error
This one’s sneaky. You treat, you bill, you hit the therapy cap. But you forget KX. Now your claim sits unpaid. Because KX tells CMS your care is still medically necessary. Without it, they assume it’s not. It’s not about more paperwork. It’s about proof. Your documentation must show why therapy continues past the limit. When you manage Physical Therapy Modifiers right, this mistake disappears. One letter. One line in your note. That’s all it takes.
The Fix
The fix is simple. Slow down. Check your documentation. If your notes don’t prove it, the modifier doesn’t exist. Write what you did. Write why you did it. That’s how you survive an audit and keep your money. That’s how you turn billing chaos into clean claims and fast payments.
Payer-Specific Nuances You Should Know
Here’s where it gets messy. Every payer plays by its own rules. What works for one fails for another. There’s no single playbook. No universal logic. One payer demands proof before payment. Another rejects the same proof as too much. It’s a maze of conditions, edits, and thresholds. Miss one detail, and the claim stops cold. So let’s make it clear. Let’s lay it out where you can see it. Because when you understand what each payer wants, you stop guessing and start winning.
| Payer | What They Expect | What Happens If You Miss It |
|---|---|---|
| Medicare | Requires KX once therapy threshold is reached. Must prove medical necessity in notes. | CMS stops payment. Claim sits until corrected. |
| Blue Cross | Often demands prior authorization even when modifiers look perfect. | Denial hits. You appeal. You wait. |
| Commercial Payers | Some reject duplicate modifiers. Others need them in a specific order. | Claim rejected for “invalid modifier use.” |
| Medicaid Plans | Follow state-specific rules. Documentation must match policy exactly. | Delays and audits. No exceptions. |
Each payer speaks a different language. One letter can change the outcome. One rule can flip a claim from paid to denied. So what’s the lesson? Always check the payer policy. Every time. It takes a minute. It saves you hours of appeal work. Because when it comes to Physical Therapy Modifiers, guessing is expensive. Clarity is profit.
Best Practices to Simplify Modifier Use
You can make Physical Therapy Modifiers almost automatic. It’s not magic. It’s structure. You need systems that think before you do. Ones that catch mistakes, flag gaps. And Whisper reminders before claims go out. Because billing shouldn’t feel like guesswork. It should flow. Steady. Certain. Precise. When the right systems are in place, modifiers stop being chaos. They become rhythm. Clean. Predictable. Paid.
- Keep a modifier cheat sheet by every workstation.
- Add EHR alerts for missing or conflicting codes.
- Run monthly audits to catch trends early.
- Train your team every quarter on CPT and modifier pairing.
The AAPC says regular audits cut errors by up to 30%. That’s not theory. It’s proven through thousands of real claims. Audits reveal the cracks before they split wide. They show patterns, habits, and blind spots that cost money. So make it habit. Not a chore. Because consistency is quiet power. It’s what keeps your claims clean and your payments steady.
How Automation Can Simplify Modifier Application
Humans get tired. Software doesn’t. Automation scans every claim in seconds. It spots what you miss, the missing GP, the wrong 59, the absent KX after the cap. CMS encourages using tech that improves billing accuracy. It’s not just about speed. It’s about consistency.
Smart billing systems read your documentation and suggest modifiers before submission. They stop rejections before they happen. They learn your patterns, your habits, your mistakes. They notice what you miss when you’re tired. Every claim gets checked, line by line, code by code. It’s precision without pause. Protection without effort. Relentless and exact. Like a silent partner standing behind you, watching your every code, guarding your every dollar. Always alert. Always steady. Never distracted.
How Pro-MBS Helps Physical Therapy Practices Get It Right
Billing chaos hits hard. Claims bounce back. Denials pile up. You fix one error, and another appears. Time drains. Revenue slows. The cycle never ends. Every missed modifier, every skipped check, costs more than money. It costs trust. It costs time you can’t get back.
That’s where Pro-MBS steps in. We live inside the details. We know every CMS rule, every payer quirk, every modifier that matters. Our systems don’t guess. They verify. Automation flags what’s missing. Experts fix what’s wrong. Every claim leaves clean. Every payment comes faster. Every practice breathes easier. The result is simple. Fewer denials. Faster payments. Stronger cash flow. We don’t chase revenue. We build it right the first time.
Frequently Asked Questions
What Modifiers Are Used for Physical Therapy?
Physical Therapy Modifiers like GP, 59, and KX define purpose and precision. They prove each service was distinct, medically necessary, and compliant with CMS rules. Used right, they cut through denials and speed up payments. Pro-MBS helps your team master modifier logic so your claims move fast and clean.
What is the 76 and 77 Modifier Used For?
Modifier 76 means a repeat procedure by the same provider. Modifier 77 means it was repeated by another. Both tell payers the action was intentional, not a billing error. These Physical Therapy Modifiers protect against duplicate claim denials. At Pro-MBS, we ensure every modifier is chosen with precision so your work gets paid without delay.
Does Modifier 52 Reduce Payment?
Yes. Modifier 52 means the procedure was reduced or incomplete. Reimbursement drops because only part of the service was performed. In Physical Therapy Billing, use it carefully and document the reason. Pro-MBS trains your team to apply it only when it saves compliance, not when it costs revenue.
When to Add 59 Modifier in Physical Therapy?
Use Modifier 59 when two therapy procedures are separate and distinct. It tells payers both were valid, not duplicates. Without it, one code dies in denial. Pro-MBS keeps your Physical Therapy Modifiers accurate and airtight, protecting every clean claim before it leaves your system.
What is the 8-Minute Rule for Physical Therapy Billing?
The 8-Minute Rule, defined by CMS, governs how time-based therapy codes are billed. One unit equals at least eight minutes but under twenty-three. Miss the timing, and you lose revenue. Pro-MBS builds automation and audits to keep every treatment minute counted and every dollar earned.
How to Maximize Physical Therapy Billing?
Start with precision. Use correct Physical Therapy Modifiers, follow the 8-Minute Rule, and verify payer policies. Automation and monthly audits turn guesswork into accuracy. Pro-MBS brings that structure, transforming billing chaos into steady, predictable cash flow.
How Many Minutes is 3 Units in PT?
Under CMS rules, three therapy units mean thirty-eight to fifty-two minutes of direct care. Each added unit demands full documentation. Your timing must match your notes, or compliance falters. Pro-MBS ensures every unit is tracked, recorded, and justified so your claims never stumble under review.
What Are the Different Types of Modifiers?
There are informational, payment, and CPT Modifiers. In therapy, the ones that matter most are GP, 59, KX, and 76. Each defines intent, necessity, and compliance. Pro-MBS teaches your team to wield Physical Therapy Modifiers with clarity and confidence so payments come faster and denials fade.



