Medicare Updates For Physical Therapy Billing 2025 are finally here, and they are reshaping how physical therapists bill, document, and get reimbursed. Have you checked what has changed in your codes, your modifiers, or your documentation rules yet? Because this year, small mistakes could mean big denials.
Let’s unpack what matters most in these Medicare Updates For PT Billing 2025. This year, the changes run deeper than a few code tweaks. We are talking about new CPT codes that redefine how services are classified, updated supervision rules that change how PTAs and OTAs can work in outpatient settings, and modifier clarifications that now leave zero room for error. Add to that the latest MIPS 2025 performance measures, new quality reporting standards, and stricter documentation timelines, and you have a year where precision truly decides your bottom line.
These updates affect every part of your daily routine, from how you plan your sessions to how you record every minute on your claim. If you miss even a single compliance detail, CMS can flag your claim, delay payment, or deny it entirely. But if you understand these shifts early, you can stay ahead, stay compliant, and get paid faster without the constant back and forth of resubmissions.
This guide breaks down everything you need to know, step by step, so you can move through 2025 with clarity, confidence, and control.
Understanding the Basics of Physical Therapy Billing
What’s the foundation of Medicare PT billing? It still runs on the fee-for-service model, meaning you are paid per service, not per outcome. Each therapy visit is built around CPT and HCPCS codes, which describe exactly what you did.
But here’s the catch: accuracy is everything. CMS expects therapists to document every minute, every modifier, every signature. Timed codes must match the clock. Untimed codes must show clear medical necessity. Miss one detail and your claim hits a wall.
Billing isn’t just about entering numbers. It’s about proving skill, purpose, and compliance in every session.
Updated CPT and HCPCS Codes for Physical Therapy
So, what’s new in 2025? CMS finalized its annual updates, and physical therapy sits right in the middle of those changes.
The conversion factor dropped from $33.29 in 2024 to $32.35 in 2025, according to CMS’s final rule. That means slightly lower reimbursement per unit. The therapy threshold also increased to $2,410 for PT and SLP combined, as confirmed by APTA. Exceed that, and you will need the KX modifier to show medical necessity.
Another win is that general supervision is now allowed for PTAs and OTAs in private practice outpatient settings. That gives clinics more flexibility without breaking compliance, a major change acknowledged by APTA and the American Medical Association (AMA).
Let’s make it simple:
| Change | 2024 | 2025 |
|---|---|---|
| Conversion Factor | $33.29 | $32.35 |
| PT/SLP Threshold | $2,330 | $2,410 |
| PTA Supervision Rule | Direct supervision | General supervision |
Fewer limits, more responsibility. This year, Medicare trusts you but also watches more closely. Every decision you make in billing or documentation now carries more weight than ever before.
What Are the Most Common CPT Codes Used in Physical Therapy
Still using the same old codes? Sure, they look familiar, but their documentation standards matter more than ever in 2025. Each code now tells a story about patient progress, medical necessity, and the value of your care.
- 97110 – Therapeutic Exercise. Use it when improving strength, flexibility, or endurance. Note every movement and patient response.
- 97112 – Neuromuscular Re-education. Focuses on coordination, balance, and proprioception. Record the specific deficit addressed and improvement observed.
- 97530 – Therapeutic Activities. Hands-on functional movements such as lifting, reaching, and transfers. Show how each activity connects to daily life.
- 97161–97163 – Evaluations. Choose complexity carefully. CMS auditors check if your chosen level truly reflects time, decision making, and complexity.
Small code, big implications. Mislabel one, and you might lose more than a unit. You could face a red flag on an audit. One small oversight in coding can turn a routine claim into weeks of payment delays and compliance reviews.
What Is the Best Way To Master the 8-Minute Rule?
How often do you second-guess your unit count? The 8-minute rule is still the backbone of PT billing. CMS says you must provide at least 8 minutes of a timed service to bill one 15-minute unit.
Here’s your example rewritten as a clean, professional table:
| Total Timed Minutes | Billable Units |
|---|---|
| 8–22 minutes | 1 unit |
| 23–37 minutes | 2 units |
| 38–52 minutes | 3 units |
How do I Use Billing Modifiers Correctly?
Modifiers tell Medicare who did the work and why it mattered. Get them wrong, and even perfect documentation can’t save the claim.
- GP – Required on every PT service under a plan of care.
- CQ – For services partly or fully delivered by a PTA.
- CO – The OTA equivalent for occupational therapy.
- KX – When you pass the annual therapy threshold and justify medical necessity.
- 59 or X-modifiers – When you bill two procedures that are distinct from each other.
Here’s a real-world example: a clinic billed 97110-GP for a PTA session but forgot the CQ modifier. Result? Denied claim. Why? Because CMS automatically applies a 15% payment reduction when a PTA provides more than 10% of service minutes. Without CQ, that rule doesn’t trigger correctly, and Medicare flags it.
So always double-check your modifiers before submitting. It’s faster than filing an appeal.
MIPS 2025 and Quality Reporting for Physical Therapists
Think MIPS doesn’t apply to you? Think again. In 2025, MIPS (Merit-Based Incentive Payment System) continues to affect how much you earn or lose on every Medicare claim.
The penalty for poor performance stays at -9%, per CMS’s 2025 quality measure benchmarks. That means failing to report correctly could cost thousands. So, what changed? PTs can still report via claims, EHR, or registry, but quality measures are now narrower and more outcome-based. APTA notes new emphasis on documentation of medications, fall risk management, and patient-specific functional outcomes.
Want a bonus instead of a penalty? Keep these habits:
- Audit your data early in the reporting year.
- Align measures with your actual patient mix.
- Keep documentation crystal-clear and ready for submission.
The smarter your data, the stronger your reimbursement. Numbers tell a story, and Medicare listens closely. When your reports are clean, your outcomes clear, and your documentation solid, CMS sees more than data. It sees value. That is how strong reporting turns into stronger payments.
Documentation and Compliance Standards for 2025
This year, CMS tightened its stance on documentation integrity. Why? Because poor notes cost billions and weaken trust in Medicare. Auditors are watching closer than ever, searching for shortcuts and sloppy copy-paste templates.
Every line you write has to show skill, purpose, and intent. It’s not about writing more; it’s about writing what matters. In 2025, good documentation isn’t just paperwork. It’s proof that your care makes a difference.
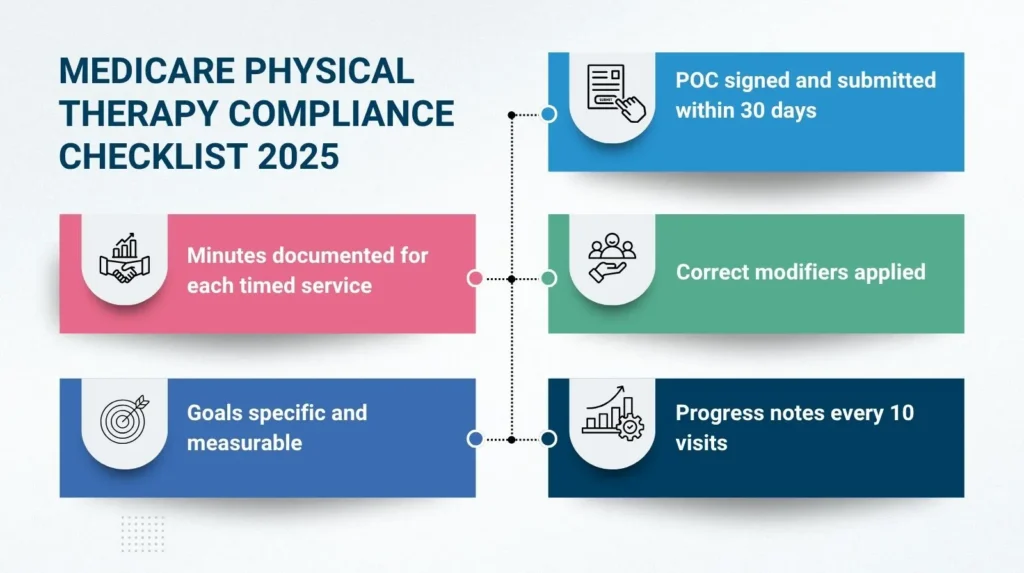
So, what must your notes include in 2025?
- A signed Plan of Care (POC) submitted within 30 days of evaluation.
- Measurable goals with clear time frames.
- Progress reports every 10 visits or 30 days.
- Distinct notes without copy-pasting or “cloned” templates.
And remember the new rule confirmed by APTA: if a physician’s referral is signed and dated, it can serve as certification as long as your POC reaches them within that 30-day window.
Want to stay audit-proof? Try this mini checklist:
Compliance isn’t optional. It’s your defense against take-backs and audits. Every note you write matters. Every signature, every modifier, every minute on that timesheet tells a story. CMS isn’t just checking boxes; it’s checking for truth. Solid documentation shields you from denials and delays. It proves your care had purpose. In 2025, compliance is more than a rule. It’s protection. It’s credibility. It’s the difference between getting questioned and getting paid.
Medicare Reimbursement Trends and MPPR
Wondering how much you will actually get paid this year? Let’s look at what changed.
The 2025 conversion factor drop to $32.35 slightly cuts unit payments. That means each CPT code earns a bit less, about a 2.8% reduction overall, according to CMS’s final rule. And don’t forget the Multiple Procedure Payment Reduction (MPPR). When you bill multiple therapy codes in one session, the second and later codes get a reduced rate on their practice expense portion. CMS still enforces this rule in 2025.
So, what can you do? Optimize your scheduling. Spread out same-day procedures when appropriate. Make sure every billed service is fully justified and clearly documented.
Let’s look at the averages:
| Code | 2024 Avg Rate | 2025 Avg Rate |
|---|---|---|
| 97110 | ~$29.29 | ~$28.79 |
| 97112 | ~$33.62 | ~$32.02 |
The difference may seem small, but over hundreds of visits, it adds up fast. This is why outcome-based care is becoming the long game. Medicare’s gradual shift toward value reflects its push for results over volume. PTs who prove patient improvement through data and documentation will always come out ahead.
Partner with Pro-MBS for PT Billing and Medicare Compliance
Medicare billing in 2025 isn’t simple. The rules shift, modifiers change, and documentation demands keep growing. That’s where Pro-MBS steps in. We know CMS inside out, and we make compliance easier to manage. Our team helps you bill cleanly, track your numbers, and stay audit proof. No guesswork, no chaos, just clarity and control over your revenue.
At Pro-MBS, we believe precision pays. We look at every modifier, every claim, every signature before it becomes a problem. You treat patients, we handle the paperwork. Together, we keep your claims clean, your payments fast, and your compliance solid. Stay compliant, reduce denials, and strengthen your reimbursement with Pro-MBS, your Medicare billing partner for 2025.
Frequently Asked Questions
What are the changes in Medicare for 2025?
Everything shifted. Medicare Updates For PT Billing 2025 cut the conversion factor, raised the therapy threshold, and redefined PTA supervision. CMS tightened compliance. Every note now speaks for or against you. At Pro-MBS, we translate these new rules into clear action so your claims stay compliant, fast, and audit-proof.
What is the reimbursement rate for physical therapy in 2025?
Lower but precise. Under Medicare Updates For PT Billing 2025, the conversion factor dropped to $32.35, with average payments near $28.79 for code 97110. Margins shrink, but clean claims still win. Pro-MBS keeps your coding exact and documentation airtight so every dollar you earn reaches your account.
What is the final rule for MIPS 2025?
The law is simple. Medicare Updates For PT Billing 2025 makes outcomes the measure and data the judge. Miss reporting and you lose 9 percent. Prove value and you rise above penalties.
Pro-MBS builds MIPS compliance into your workflow so every report turns data into strength and payment into certainty.
What are the changes in Medicare July 2025?
July brings enforcement, not surprises. Under Medicare Updates For PT Billing 2025, CMS intensifies review on KX modifiers, the 8-minute rule, and MPPR reductions. No leniency. No guesswork. Pro-MBS keeps your documentation aligned with every policy update so denials never find a way in.
Will Medicare pay for physical therapy?
Yes, when you play by the rulebook. Medicare Updates For PT Billing 2025 demands medical necessity, valid CPT codes, and flawless documentation. Miss one, and payment dies on arrival. Pro-MBS ensures your notes, modifiers, and claims flow in rhythm, which is compliant, clean, and ready for approval.
How many units can you bill for PT?
Time rules all. Under Medicare Updates For PT Billing 2025, 8 to 22 minutes earns one unit, 23 to 37 earns two, 38 to 52 earns three. The 8-minute rule never sleeps. Pro-MBS audits your timing and documentation so every billed minute stands firm under CMS scrutiny.
What is the Medicare code for physical therapy?
There’s no single code, only purpose in numbers. 97110 for exercise. 97112 for neuromuscular re-ed. 97530 for therapeutic activity. Together they form the backbone of Medicare Updates For PT Billing 2025. Pro-MBS ensures each code tells the right story, earning the payment your work deserves.



