CPT 97530 Billing Guidelines. Three words every therapist knows. Three words that can decide whether your work gets recognized or denied. The room smells like rubbing alcohol and effort. A patient lifts, wobbles, steadies. You guide them, one more rep, one more breath, and somewhere behind that motion lies paperwork. Numbers, Codes, and Proof.
That is what this code is about. Proof. Proof that every lift and reach had purpose. That therapy restored life, not just movement. So how do you tell that story the right way? Let’s walk through it, clean, compliant, and real.
What Is CPT 97530 and Why Does it Matter?
Every therapist’s day begins with the same question. What am I billing for? According to the AMA CPT Manual, CPT 97530 means “Therapeutic activities, direct (one-on-one) patient contact (use of dynamic activities to improve functional performance), each 15 minutes.” Forget the jargon for a moment. This is not about counting exercises. It is about helping someone lift a grocery bag, climb stairs, or rise from a chair without fear.
Think of it like this:
• You help them balance on uneven ground: A slow step forward, a shift in weight, a hand reaching for stability. Every wobble matters. You train the body to trust itself again, to react, to recover without panic.
• You teach safe lifting: A weighted box, a bent knee, a braced back. It looks simple, but it saves spines and confidence alike. You rebuild patterns that protect the body in real life, not just on the therapy mat.
• You build the confidence to move again: The moment they stand tall without help is the victory. You see fear fade and function return. That is where therapy stops being routine and becomes transformation.
That is what CPT 97530 Billing Guidelines exist to protect. Not just motion but meaning. Movement that connects therapy to life beyond the clinic walls.
How to Document CPT 97530 the Right Way?
A therapist’s note is a story, and under CMS rules, it must be told with detail. If the story is unclear, payment disappears. Your documentation should show why the activity mattered, how it was done, and what it changed.
| Required Element | Example Entry |
|---|---|
| Functional Goal | “Patient will transfer independently from bed to chair.” |
| Activity Description | “Practiced sit-to-stand transfers for 15 minutes.” |
| Duration | “2 units (30 minutes).” |
| Clinical Rationale | “Improves strength and control for safe transfers.” |
Every detail counts. Every minute must connect to function. CMS expects precision, real time, real goals, real progress. The therapist who writes like a storyteller wins audits. The one who writes like a robot gets denied.
CPT 97530 Billing Guidelines vs 97110
You have felt the confusion. Two codes, same patient, same day. Where is the line? Here it is. CPT 97530 Billing Guidelines cover dynamic, task-based work like lifting, standing, or reaching. 97110 covers repetitive, isolated muscle work like curls, stretches, or resistance training. The difference is intent.
When a patient squats to rebuild leg strength, that is 97110. When they rise from a low chair to practice a transfer, that is CPT 97530 Billing Guidelines. Payers read between the lines. CMS Therapy Billing Rules say you must prove the purpose of each service. If both codes look the same, they will strike one off your claim. Write it clearly. Different goals. Different motions. Different outcomes.
Modifier 59 For CPT 97530 Billing Guidelines
Here is where precision meets payment. When you bill CPT 97530 with 97110 on the same day, Modifier 59 is your shield. It tells the payer, “These services are distinct.” Also attach the GP modifier. It marks the session under a physical therapy plan of care.
Payer expectations:
• CMS: Always wants GP and 59 when multiple timed codes overlap. They measure everything. Minutes. Modifiers. Intent. If two services blend together, they see it. They do not guess or assume. They want proof that each act, each touch of care, stood alone with purpose.
• Aetna: Demands documentation that separates goals. They look for story, not repetition. Each code must have its own heartbeat. Show the difference between strength and function, between motion and meaning. If the goals blur, Aetna pulls the thread and the claim unravels.
• BCBS: Denies if notes sound identical between codes. They read quietly, line by line, searching for copy and paste. A repeated sentence tells them you were rushed. A repeated goal tells them you were careless. Write with intent. Make each session breathe on its own.
Forget a modifier, and your clean claim turns into an appeal letter. Follow CPT 97530 Billing Guidelines carefully and you stay in control.
What Are the Common Denials Under CPT 97530 Billing Guidelines?
Every denial starts with one small oversight. Maybe time overlaps. Maybe the activity sounds too much like an exercise. Maybe the goal is not measurable. These types of denials occur more than you think. It may not look like a threat at first but by the passage of time, it breathes fire and bites into your revenue.
Here is what usually goes wrong:
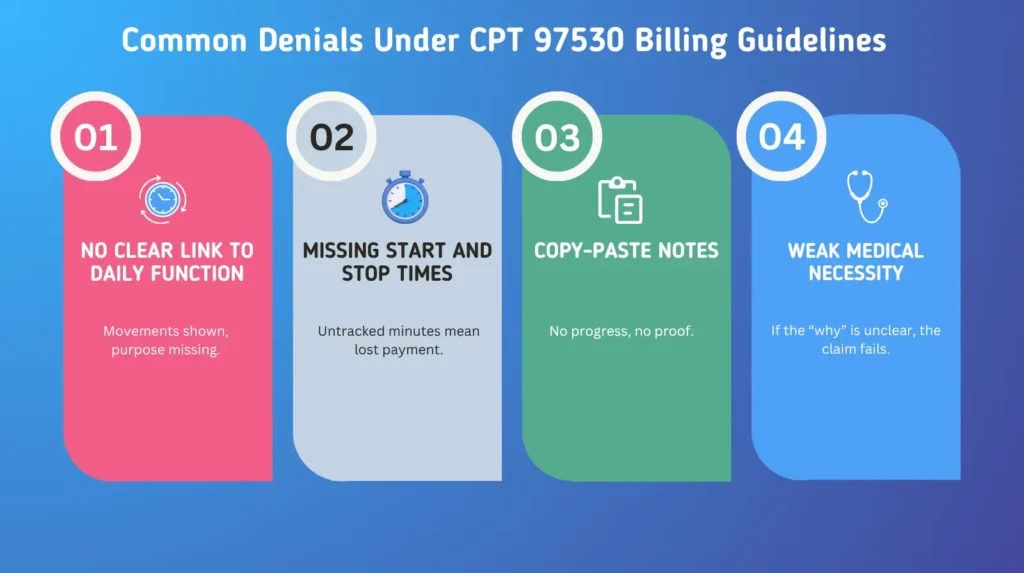
97530 Medical Necessity Documentation is the heart of it all. If you cannot show why the session mattered, payers assume it did not. Ask yourself after each note. Would I believe this was necessary if I did not know the patient?
Best Practices for CPT 97530 Billing Guidelines
You want clean claims. Then you need to follow some best practices for CPT 97530 Billing Guidelines and make your notes bulletproof. Below are the habits:
• Write every goal around function: Do not write “increase strength.” Write “stand from chair without help.” Goals must breathe life, not numbers. Function proves value.
• Document every minute of one-on-one care: Be honest. Be exact. Auditors from CMS read time like truth. One missing minute, and they question the rest.
• Keep tasks distinct between codes: Never let 97530 and 97110 blur together. One builds movement, the other builds muscle. If the difference is not clear, payment fades.
• Update goals when progress happens: Patients change. Notes should too. What worked in week one must evolve by week four. Stagnant goals tell reviewers the care went nowhere.
• Review CMS updates every quarter: Rules shift quietly. Codes change without warning. Stay alert. A single outdated detail can turn clean work into a denial.
Your words are your defense. When the audit comes, those details protect you. Each line you write is a shield. Each note, a record of truth. When questions rise, your documentation stands in the room before you do. If it is clear, you win. If it is vague, you lose time, payment, and trust. Write as if someone will read every word, because they will. Clarity is armor. Precision is survival. And in billing, survival means getting paid for the care you gave.
Reimbursement and Compliance
Numbers matter too. They always do. Under the 2025 Medicare Physician Fee Schedule, CPT 97530 Billing Guidelines tell their own quiet story. A story of minutes, movement, and payment earned through honest care.
| Detail | Description |
|---|---|
| Reimbursement Range | $38 to $45 per unit. It changes with region, but accuracy never does. |
| Unit Definition | One unit means fifteen minutes of real, one-on-one contact. Not estimated. Not rounded. Real time. |
| Two Units | Twenty-three to thirty-seven minutes. Anything less or more, and it no longer fits. |
| CMS Focus | They watch the clock and the story. Time must match purpose. Progress must be visible. |
| Audit Trigger | Repetition without change. Identical notes. Progress missing. They see it and they act. |
Too many sessions that look the same raise questions. CMS Therapy Billing Rules read patterns like open books. Track the story. Let the patient’s growth speak for you. From needing a hand to standing alone, that is what gets paid.
Why CPT 97530 Billing Guidelines Matter?
This is not just codework. It is narrative. Each 15-minute block is a chapter in someone’s recovery. You are not documenting motion. You are documenting change. A patient rising without help. A shoulder lifting without pain. A step that used to tremble now steady.
When you apply CPT 97530 Billing Guidelines correctly, you turn those moments into measurable outcomes. That is what payers understand. So ask yourself. Did my note show growth? Did it show function, not just form? If it did, that is mastery.
Pro-MBS Insight: Clean Claim Mastery
Even when your notes are flawless, the system can still trip you. Wrong modifier. Overlapping units. A code left unpaired. That is where Pro-MBS comes in. We turn billing chaos into clarity with automation and training that mirror CMS expectations.
Our tools check modifier use for CPT 97530 Billing Guidelines, audit timed codes in real time, and coach your staff to document progress like pros. It is not magic. It is method. And it keeps your focus on what truly matters, the work that heals, not the forms that haunt.
The leaks stopped. The process breathed again. Claims moved faster. Cash flow steadied. Confidence returned.
Now, Adams Physical Therapy runs with precision. Their team moves in sync. Their data speaks the truth. Their payments come on time. The chaos is gone. The calm remains. At Pro-MBS, we don’t just manage billing. We restore rhythm.
If you’re ready to see similar results, visit www.prombs.com to learn how our team can help your clinic cut denials, speed up reimbursements, and regain control of revenue.
Frequently Asked Questions
What Is CPT Code 97530 Billing Guidelines?
CPT 97530 Billing Guidelines define how therapists bill for Therapeutic Activities CPT Code that rebuild function, not just strength. Each fifteen-minute unit must prove purpose and progress. CMS wants evidence, not guesswork. Time, goal, and outcome must align. Pro-MBS helps you master this rhythm so every claim stands clean.
Can A CPT 97530 Be Billed Alone?
Yes, when it earns the right. CPT 97530 Billing Guidelines allow solo billing if the session meets Medical Necessity Documentation. The care must restore movement that matters. No overlap, no filler, just focused, functional work. Pro-MBS ensures each minute you record has meaning, proof, and payment behind it.
What Is Medical Necessity For 97530?
It means reason. It means purpose. 97530 Medical Necessity Documentation proves that every task was vital to recovery. A lift, a reach, a transfer, each one tied to life beyond therapy. Without that link, the code collapses. Pro-MBS trains your team to write notes that speak with clarity and strength.
How Many Units Can You Bill For PT?
Time is truth. Under Physical Therapy Timed Code Rules, one unit equals fifteen minutes of real contact. Two units mean twenty-three to thirty-seven minutes. Push further, and proof must follow. CPT 97530 Billing Guidelines demand precision, not padding. Pro-MBS keeps your timing tight and your claims flawless.
What Documentation Is Needed For 97530?
Clarity. Function. Purpose. That is what payers read first. CPT 97530 Documentation Requirements include goals, tasks, minutes, and the reason it mattered. Vague notes lose battles. Sharp ones win audits. Pro-MBS audits your words so every line stands like armor.
How To Bill Medicare for Physical Therapy Services?
Follow the rules, not assumptions. CPT 97530 Billing Guidelines for Medicare Physical Therapy require the GP and 59 modifiers, timed documentation, and functional proof. Each code must tell a separate story. CMS Therapy Billing Rules read closely. Pro-MBS keeps your Medicare claims fast, clean, and compliant.
How Pro-MBS Helps with Physical Therapy Billing?
Pro-MBS turns confusion into order. We teach Physical Therapy Billing Guidelines, validate modifiers, and check every timed code before it reaches the payer. Our system refines CPT 97530 Billing Guidelines from the inside out. Work with Pro-MBS and turn denials into clean approvals.
What Is The 8-Minute Rule for Physical Therapy Billing?
Eight minutes. That is the threshold. The line between billable and lost. CPT 97530 Billing Guidelines follow CMS Therapy Billing Rules. Less than eight minutes, and you cannot bill the unit. Time matters. Truth matters. Pro-MBS teaches precision so your time never goes unpaid.