CPT 97140 Modifier Guidelines. Four words that make every therapist pause. You did the work, you wrote the note. Then the denial came. Why? A missing modifier. A tiny code error that wipes out your effort. It happens every day in Manual Therapy Billing. One wrong step and the claim falls apart.
So, what is the best way to stop that? Know your codes. Understand Physical Therapy CPT Codes completely. Learn how modifiers affect payment. Let’s keep it simple. No filler, no corporate tone. Just real talk about CPT 97140 Documentation, modifiers, and getting paid for the care you give.
Understanding CPT 97140 Modifier Guidelines and Manual Therapy Techniques
What is CPT 97140? According to the American Medical Association (AMA), it covers manual therapy techniques like mobilization, manipulation, manual lymphatic drainage, and manual traction for one or more regions, each 15 minutes. It sounds simple. It isn’t.
Because it’s time-based. You must record when the session started and ended, which body part you treated, and why. Miss one of those details and Medicare or any commercial payer will flag your claim. Every note must read like proof. Every word must show purpose. That is the foundation of strong CPT 97140 Documentation.
Did You Know?
According to CMS, CPT 97140 is one of the most frequently audited codes in outpatient physical therapy due to missing or incorrect modifiers.
When To Use CPT 97140 Modifier Guidelines In PT?
When does manual therapy deserve its own billing code? Think of stiffness after surgery. Scar tissue that won’t loosen. Swelling that limits motion. Muscles so tight they fight your hands. This is the heart of Manual Therapy Billing. Your hands do what no machine can. They restore motion, reduce pain, and change function.
To bill it right, your notes need more than numbers. They need to sound like you were there.
- The reason for treatment: Why was the patient on your table? Pain? Tightness? Scar tissue that refused to let go? Say it plainly. Make it real.
- The body part treated: Be exact. Left shoulder. Lumbar spine. Post-surgical knee. The payer should know exactly where your hands worked.
- The duration of care: Write the time. Start and stop. CPT 97140 runs on the clock, and missing it means payment lost.
- The patient’s response: What changed? Less pain? Easier movement? That moment matters. It shows the therapy worked and the care was necessary.
Every bullet tells the story of your session. Clear, honest, human. Exactly what good documentation should be. For Example, “Manual therapy (97140) performed on right shoulder for soft tissue mobilization. Duration: 15 minutes. Goal: reduce stiffness and increase range of motion. Patient tolerated well.” Short. Direct. Clear. Exactly what auditors and CMS reviewers expect.
Understanding Modifier 59 And X Modifiers in CPT 97140 Modifier Guidelines
Now, let’s talk about modifiers. Modifier 59 PT means one thing: this service stands alone. It signals that the procedure was distinct and not part of another bundled service under NCCI Edits 97140. But CMS now prefers X modifiers for accuracy. They make your billing cleaner and more specific.
| Modifier | Meaning | When To Use |
|---|---|---|
| 59 | Distinct procedural service | When no other X modifier fits |
| XE | Separate encounter | Different time or session |
| XS | Separate structure | Different body part |
| XP | Separate practitioner | Another therapist performed it |
| XU | Unusual non-overlapping service | Different purpose or function |
If you mobilized the neck (97140) and exercised the knee (97110), that is separate. If both were on the shoulder, they are bundled. That is how CPT 97140 Modifier Guidelines keep your billing accurate and compliant.
Did You Know?
The NCCI automatically flags claims when 97140 and 97110 appear together without a modifier, even if they’re clinically justified.
Documentation Tips for Modifier Justification
What makes a strong note? It’s clear, specific, and easy to read. “Manual therapy (97140) on left shoulder for joint mobilization. Therapeutic exercise (97110) on right knee for strengthening. Separate regions justify modifier 59.”
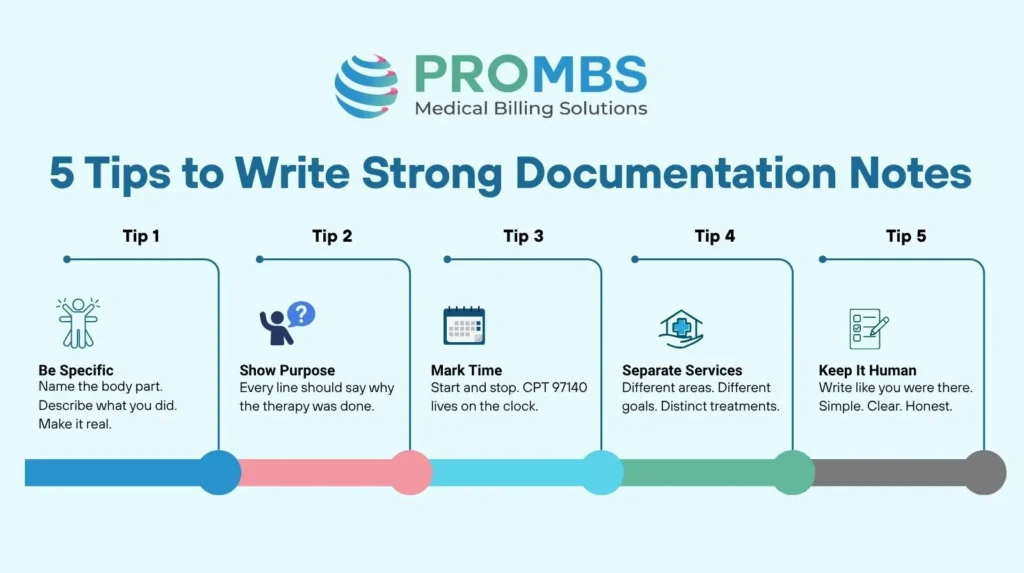
That is strong. Medicare reviewers love this kind of clarity. It is human. It is simple. Each line should answer one question: was this service truly distinct? If yes, your modifier is justified.
Payer-Specific Rules and Audit Red Flags
Medicare and The X Modifiers
Medicare is strict. Unforgiving. It wants clarity in every modifier. The X modifiers are not just letters. They are signals of separation. Different body. Different time. Different intent. If your documentation does not spell that out, the system does not guess. It denies. Medicare wants to see the difference, not imagine it. Give it proof. Give it precision.
Blue Cross Blue Shield and Modifier 59
UnitedHealthcare and Documentation Demands
UnitedHealthcare does not just want codes. It wants the story behind them. Every claim with a modifier must speak for itself. What did you do? Why did it matter? How was it distinct? Leave those answers out, and payment slows. Documentation is not busywork. It is your defense. Write like someone will read it. Because they will.
Audit Red Flags That Never Stay Hidden
Auditors from CMS and private payers do not chase small mistakes. They look for the rhythm of repetition, the quiet pattern that tells them something is off. They do not read one claim. They read a hundred. They see what repeats. They hear what sounds the same. That is how they find you. So, what do they look for?
- Billing 97140 With 97110 Every Session: When the same pairing appears day after day, it stops looking clinical. It starts looking mechanical. Show them variation. Show intent. Each session should earn its reason.
- Notes That Repeat Word for Word: Copy. Paste. Send. It is fast, but it is dangerous. Auditors see the sameness and know it is not care, it is convenience. Write what happened. Real words for real moments.
- Treated Regions That Lack Detail: A shoulder is not just a shoulder. Was it the rotator cuff? The joint capsule? The scar that restricted movement? Say it. Be exact. Let the payer see the work.
Patterns speak louder than effort. Break the pattern. Write each note like a story that belongs only to that patient, on that day, in that moment. Your words prove the work. Let them breathe. Let them stand. Let them tell the truth.
Common Denial Reasons for CPT 97140 Modifier Guidelines
Denials rarely shout. They whisper. A missed detail here. A wrong letter there. And suddenly, the work you did becomes invisible. Most errors are simple. They hide in habit, in haste, in notes written too fast. But the fix is simple too. Precision. Intention. Words that show what truly happened. Here is where claims stumble and how to steady them.
| Denial Reason | What It Means | How To Fix It |
|---|---|---|
| Missing Modifier | The claim stands half-built. The payer stops reading before it begins. | Check before you send. The right modifier completes the story. Without it, payment never starts. |
| Wrong X Modifier | One wrong letter and the meaning falls apart. The payer sees confusion, not care. | Choose carefully. XE for time, XS for structure, XP for practitioner, XU for function. Let the code fit the work. |
| Overlapping Documentation | Two services blend into one. The payer cannot tell where one ends and the next begins. | Separate by purpose and time. Write what came first. Write why both mattered. Give each its own heartbeat. |
| Same Area For Multiple Codes | The note blurs. One joint, one muscle, too many claims. The payer sees duplication. | Be specific. Name each region like a character in its own story. Shoulder. Knee. Spine. Make them stand apart. |
| Reused Templates | Repetition kills truth. Identical notes sound like echoes, not evidence. | Write fresh. Each session has its own tone. Each line should sound alive, not copied. |
Most denials begin quietly. A missing word. A repeated note. A tired habit. But precision speaks louder. In Manual Therapy Billing, every detail tells the payer you were present, focused, and right. That truth always wins.
Compliance And Reimbursement Optimization
Want to stop denials before they start? Build habits that hold when things get busy. Habits that turn accuracy into instinct. Precision does not come from pressure. It comes from practice. Here is how you keep your claims clean and your revenue steady.
- Train Your Team Regularly on NCCI Edits 97140: Knowledge fades when it is not used. Keep your staff sharp. Review updates. Discuss real cases. Let everyone know how edits change and how to stay ahead of them.
- Audit Random Charts Each Week: Do not wait for an audit to find your mistakes. Catch them first. A small review every week keeps patterns visible. It is better to find one weak note today than twenty denials next month.
- Add EHR Alerts for Modifier Checks: Technology should protect you, not slow you down. Set smart prompts in your EHR. When a risky pairing appears, the system should whisper before the payer shouts.
- Track Denials by Payer to Find Weak Points: Every denial has a story. Follow it. Was it the same modifier? The same service combination? The same therapist? Track it, fix it, and teach from it. That is how you build a team that learns, not one that repeats.
When your team educate themselves the reason behind each modifier, compliance feels natural. Mistakes drop, and your revenue stays steady. That is the power of strong CPT 97140 Documentation.
Did You Know?
Over 40% of PT claim denials come from missing or misused modifiers. That is something Pro-MBS audits can catch before submission.
Why Should You Trust Pro-MBS For CPT 97140 Modifier Guidelines and Reimbursement?
Here’s the truth. Precision is not paperwork. It is power. CPT 97140 Modifier Guidelines are not just billing codes. They are proof that your care was skilled, compliant, and real. Each modifier tells the payer a story that your work was distinct, necessary, and supported by documentation. Before you send that claim, pause for a moment.
Ask yourself. Did I show what I did? Where I did it? Why it mattered? If yes, you are solid. If not, fix it now before the denial lands. Clean notes. Clear modifiers. Confident billing. That is how you keep your revenue steady and your compliance safe.
At Pro-MBS, we believe in that same precision. We help therapy providers stay ahead of Medicare, CMS, and payer audits. From Manual Therapy Billing reviews to NCCI Edits 97140 checks, we make complex rules simple and compliance effortless. Getting paid should never feel like a fight. Need a partner who understands every CPT code and why it matters? Connect with Pro-MBS today. Protect your payments. Guard your practice. Bill with confidence.
Frequently Asked Questions
What is CPT code 97140 billing guidelines?
The CPT 97140 Modifier Guidelines are not paperwork. They are law in motion. Each session must have time stamped, purpose defined, and action proved. Miss one, and payment dies before it’s born. This code demands discipline. Every move written. Every second accounted for. Pro-MBS trains your team to write with precision so no effort ever fades into denial.
Does CPT 97140 need a modifier?
Yes. Always. Without a modifier, 97140 stands incomplete. The CPT 97140 Modifier Guidelines require 59 or XS to separate what is distinct from what is bundled. It is the difference between proof and presumption. Pro-MBS builds that clarity into your workflow with clean, unshakable billing.
What can be billed under manual therapy?
Manual therapy is the language of hands. Mobilization. Manipulation. Traction. Drainage.
Under the CPT 97140 Modifier Guidelines, every action must carry a reason and a clock. Each line in your note must show skill, not habit. Intention, not repetition. Pro-MBS turns that understanding into structure where every movement earns its place and every word earns its pay.
Can you bill 97140 for dry needling?
No. Dry needling walks another path. It belongs to 20560 and 20561, not 97140. Mixing them is like crossing wires. Sparks. Audits. Denials. The CPT 97140 Modifier Guidelines draw a clean border between touch and technique. Pro-MBS keeps you on the right side of that line. Compliant. Precise. Untouchable.
How many units can you bill for 97140?
One unit. Fifteen minutes. Nothing less. Nothing blurred. The CPT 97140 Modifier Guidelines are built on time, and time does not bend. Each tick of the clock must live in your documentation. Pro-MBS audits every second and every signature until your claims move like clockwork. Smooth. Fast. Exact.
What is the reimbursement rate for 97140 CPT code?
CPT 97140 pays between $28 and $33 per unit, but the rate means nothing without accuracy. Payment follows precision, not effort. Your notes must breathe proof. Your modifiers must align with purpose. Pro-MBS shapes that precision so every claim that leaves your clinic returns with payment in full.
Can CPT codes 97012 and 97140 be billed together?
Yes, if the purpose divides cleanly. Traction pulls. Manual therapy restores. One machine. One mind. Two goals. The CPT 97140 Modifier Guidelines demand proof that they stood apart. Pro-MBS helps you draw that line with clarity and control so payers see truth, not duplication.
Is CPT code 97140 covered by Medicare?
Yes, but Medicare believes only what it can read. Your notes must show time, need, and the modifier that ties it all together. The CPT 97140 Modifier Guidelines are the map, and every line is a direction. Pro-MBS makes sure you follow it step by step until compliance becomes instinct and denials fall silent.