Medical credentialing services are a special process that hospitals use to double-check that every doctor is qualified, honest, and safe to work with patients. Think of it like a high-tech background check that proves a doctor really graduated from medical school and has a valid license to practice medicine.
Medical credentialing services act as the primary safety gate for healthcare systems. Their job is to perform a deep check of a doctor's professional background. This process confirms that a healthcare provider’s education, training, and licenses are real and meet federal rules.
By organizing this data in one place, these services help hospitals lower legal risks. It also creates the official record needed for a doctor to treat patients and get paid by insurance companies.
Standard Protocols for Medical Credentialing Services
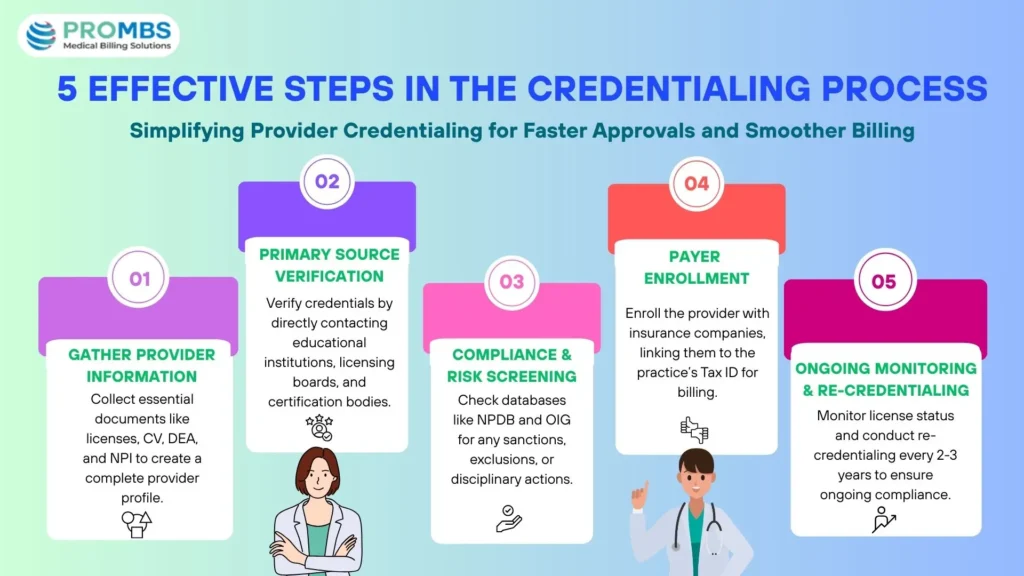
To follow the law, medical credentialing services use strict steps to check facts. This process makes sure no information is used unless it is confirmed directly by the place it came from.
- Primary Source Verification (PSV): This is like a "detective check." Instead of just looking at a copy of a doctor’s diploma, the service calls the college or the medical board directly. This stops anyone from using fake documents to get a job.
- Database Checking: These are digital searches through official national lists. Think of it like a background check for doctors. It looks at systems like the National Practitioner Data Bank (NPDB) to see if a doctor has ever had legal trouble or lost their license in the past.
- Clinical Privileging: This is the hospital's way of giving a doctor "permission" to do certain things. It’s a formal "yes" that allows a provider to do specific surgeries or treatments based on the skills they have proven and the equipment the hospital owns.
2026 Industry Updates for Medical Credentialing Services
In 2026, medical credentialing services have become much faster and more digital. Hospitals are no longer using slow paper forms. Instead, they use "always-on" technology to keep patients safe. Here are the biggest changes happening right now:
- AI-Powered Fact Checking: Computers use Artificial Intelligence (AI) to read thousands of doctor records in seconds. This finds mistakes in a doctor's history much faster than a human could. It can even spot a fake degree or an old license error instantly.
- Interstate Compacts ("Fast-Pass" Licensing): Over 42 states now share a "fast-pass" system for licenses. If a doctor is already checked and working in one state, they can get permission to work in another state in just a few weeks instead of months.
- Continuous Monitoring (24/7 Safety): In the past, hospitals only checked a doctor's records every two years. In 2026, systems watch records every single day. If a doctor gets into trouble on a Tuesday morning, the hospital is alerted by Tuesday afternoon.
- Tighter Deadlines: New rules (like those from the NCQA) have shortened the time allowed for checks. Hospitals now have only 120 days to finish primary source verifications, down from 180 days in the past.
- Monthly Exclusion Checks: New rules now require hospitals to check national lists (like the OIG and SAM.gov) every 30 days for all employees and vendors. This ensures that no doctor, employee, or vendor is involved in patient care if they have been banned from federal programs like Medicare.
- 30-Day Decision Notification: Once a committee reviews a doctor's file, new NCQA rules require the hospital to notify the doctor of the final decision within 30 calendar days. This ensures doctors aren't left waiting for months to start working.
- Enhanced Telehealth Rules: Virtual Direct Supervision: For doctors seeing patients over video, CMS now requires 2026-certified technology. Credentialing teams must verify that a doctor's digital equipment meets these high safety and privacy standards before they are allowed to treat patients remotely. Additionally, as of January 1, 2026, CMS allows doctors to provide Virtual Direct Supervision via real-time audio-video technology. This allows providers to supervise clinical activities remotely, increasing flexibility and access to care.
Did You Know? Monthly Exclusion Checks Are Important
Every 30 days, hospitals must check if any staff or vendors are banned from programs like Medicare. This helps make sure no one who shouldn't be working with patients is doing so. If this check is missed, the hospital could face penalties.
Compliance Standards in Medical Credentialing Services
Following the rules set by groups like the National Committee for Quality Assurance (NCQA) is the main goal of medical credentialing services.
These groups set strict timelines for how data is collected. For example, while some state laws allow a license to be checked within 180 days before a doctor is hired, the NCQA's 2026 standards have tightened this to 120 days.
If a hospital misses these deadlines, it can lose its official accreditation. This would stop the hospital from being able to accept government funding or even stay open.
Did You Know? Telehealth Tech Must Be Certified
Doctors who do telehealth need to use certified equipment. CMS now requires this to make sure digital tools are safe. Credentialing teams must check the technology before doctors can treat patients remotely.
The Role of Credentialing Verification Organizations (CVO)
Many hospitals hire an outside company called a CVO to help. A CVO is a specialist in the medical credentialing services verification process. By using a CVO, a hospital can move the heavy paperwork load to experts who handle it faster.
Why Certified CVOs are Faster: In 2026, the NCQA sets different speed limits for data. While hospitals (Accredited) have 120 days to finish a check, a professional CVO (Certified) is required to finish verifications in just 90 days. This 30-day "head start" is why hospitals use CVOs to get doctors approved and billing insurance much faster.
The CVO gathers a "clean file" and sends it back to the hospital’s leaders. The hospital then makes the final legal choice on whether to allow the doctor to work there.
Data Security and Privacy Rules
Since medical credentialing services handle private data—like Social Security numbers and NPI (National Provider Identifier) codes—the system must be very secure. This includes:
- Data Encryption: All provider files are "scrambled" using high-level digital locks so hackers cannot read them.
- Controlled Access: Only specific people in the HR or medical office are allowed to see a doctor's private files.
- Digital Logs: The system keeps a record of every person who looks at or changes a file. This ensures the data stays accurate for future audits.
Payer Enrollment: Joining the Insurance Network
Even after a doctor is fully checked out, they still cannot send bills to insurance companies right away. They must first go through Payer Enrollment. This is the official way a doctor joins an insurance group (like Blue Cross or Aetna).
- Signing the Contract: The doctor’s office must sign a legal promise with the insurance company. This paper decides how much money the doctor will get for their work.
- Getting a Secret ID Number: Once the doctor is joined up, they get a special ID number for that insurance company. Without this number, the insurance company will not pay the office.
- The Start Date: This is the most important part! A doctor cannot get paid for any patient they saw before their official start date in the insurance computer.
Enrollment Strategies for Medical Credentialing Services
A common mistake in medical credentialing services is forgetting to link the doctor to the specific office where they work. This is called Provider Enrollment. It is like making sure the doctor's name is on the right office door.
- Doctor ID vs. Office ID: Every doctor has a personal ID number. But every business has its own "office" ID number. The team must link these two numbers together in the system.
- Sending the Check to the Right Place: There is a special form that tells the insurance company: "Please pay the office, not the doctor's house." If this is not done right, the money might get sent to the doctor’s home by mistake!
- Checking the Address: If a doctor works at three different clinics, they must be signed up at every single address. If the address is wrong, the insurance company might not pay the bill.
Pro Tip: Link IDs to Prevent Payment Mistakes
Make sure the doctor’s ID matches the office ID in your billing system. If this isn’t done right, the insurance payment could go to the wrong place. Linking the IDs helps payments go smoothly.
Revenue Impact of Medical Credentialing Services
Credentialing is also vital for the financial health of a medical practice. Insurance companies will not pay a doctor until they have been fully checked and added to the network.
| Phase | Technical Requirement | Impact on Income |
|---|---|---|
| Payer Enrollment | Sending verified files to insurance companies. | Allows the office to send bills for payment. |
| CAQH Maintenance | Regularly updating a national doctor database. | Keeps the doctor “in-network” so patients can visit. |
| Re-credentialing | Checking all facts again every 2 to 3 years. | Makes sure the doctor stays eligible to get paid. |
Optimizing Workflows for Medical Credentialing Services
The biggest challenge for medical credentialing services is the massive amount of paperwork that expires. Efficiency is improved by using software that automatically tracks dates for state licenses and insurance. If a doctor’s license expires, they face an "administrative suspension."
This means they are legally blocked from seeing patients until the paperwork is fixed. Modern systems use cloud-based portals to keep these files ready for quick reviews by regulators.
Pro Tip: Use Automation to Track Expirations
To avoid missing important dates, use automated systems that remind you when licenses and certifications need renewal. This helps keep everything up-to-date without mistakes.
Strategic Efficiency in Medical Credentialing Services
The rules for doctors are changing fast in 2026. If you try to do the paperwork yourself, it can take too long. This can stop your office from making money. You need a partner who can handle the rules and help you get paid.
At Pro-MBS, we make this hard work easy. We help your practice stay healthy and strong:
- Get Paid Faster: We use a special 90-day "fast track" to check your doctors. This helps them start billing insurance a month sooner than other places.
- We Know Your Work: We know the rules for over 40 types of doctors. Whether you fix hearts or help with mental health, we get your forms right the first time.
- Always Watching: Our team works all day and night. We check safety lists every 30 days. This makes sure every worker is allowed to help patients.
- Simple Billing: We link our doctor checks to your billing system. This stops small mistakes that cause insurance companies to say "no" to a bill.
When you pick Pro-MBS, you trade messy files for "quiet control." Our medical credentialing services let your doctors focus on patients while we handle the rest.
Frequently Asked Questions
How much do medical credentialing services cost in 2026?
In 2026, medical credentialing services typically cost $150 to $400 per provider, per payer. For a new physician joining five panels, the total cost averages $1,500 to $2,500. Outsourcing prevents revenue loss, as credentialing delays can cost practices $2,500+ daily in unbillable services.
What is the difference between initial credentialing and re-credentialing
Initial credentialing is a comprehensive background audit for new hires taking 90–120 days. Re-credentialing is a periodic renewal occurring every 2–3 years. In 2026, the primary difference is the addition of continuous monthly monitoring of licenses and sanctions between these major cycles.
Why are medical credentialing applications denied in 2026?
The three primary reasons for 2026 credentialing denials are:
- Undocumented Work Gaps: Any gap over 30 days requires written explanation.
- Document Expiration: Licenses or malpractice policies expiring during the 120-day review.
- Data Inconsistency: Mismatches between CAQH profiles and state board records.
How Pro-MBS Can Help You Today?
Don't let "pending" status drain your practice's bank account. Pro-MBS provides expert oversight to ensure your applications are "first-time final," getting your doctors to work 30 days faster than the industry average.