If you're a healthcare provider new to billing Medicaid, you might feel unsure where to begin. Unlike commercial insurance, Medicaid is managed by state governments and comes with unique billing rules. From getting credentialed to submitting clean claims, every step in the medical billing process matters if you want to get paid on time and avoid denials.
This guide is written for providers who are completely new to Medicaid billing. We’ll explain everything clearly so you can build confidence and start billing correctly.
What Is Medicaid and Who Is It For
Medicaid is a public health insurance program that provides medical coverage to low-income individuals and families. It’s funded jointly by the federal government and each state, but managed at the state level. That means every state has its own rules for eligibility, services covered, and how providers bill the program.
In general, Medicaid covers services like physician visits, hospital care, mental health support, nursing home services, and prescriptions. Understanding what your state’s Medicaid plan covers is essential before providing services or submitting claims.
Enroll as a Medicaid Provider
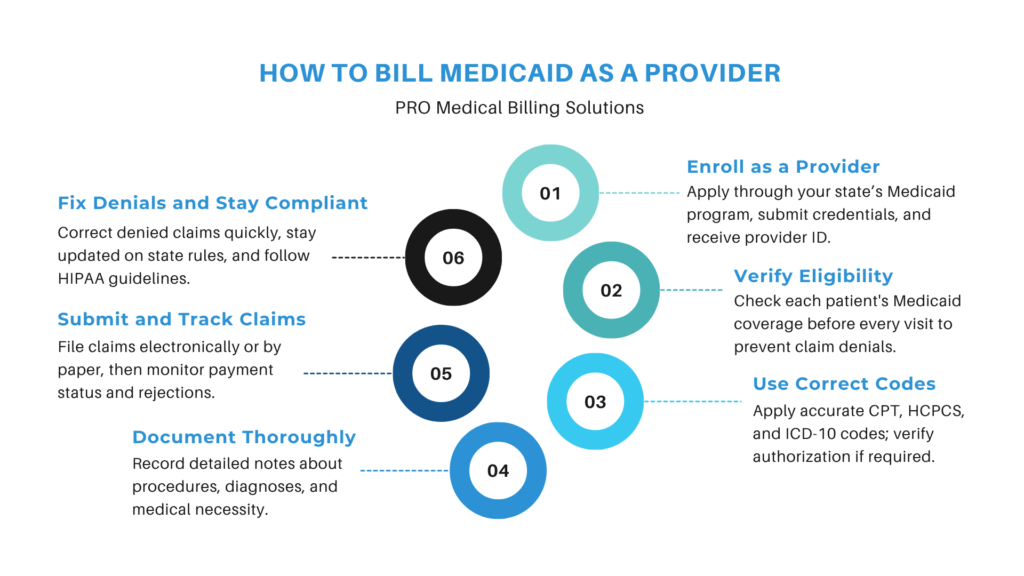
Before you can bill Medicaid, you must be enrolled and approved as a Medicaid provider. This process involves submitting an application to your state’s Medicaid agency. You’ll need to provide your National Provider Identifier (NPI), medical license, tax ID, and other credentials. Once you're approved, you’ll receive a Medicaid provider number or ID, which is required when billing.
Enrolling may take a few weeks, so it’s a good idea to begin this process as early as possible. Keep in mind that many states also require revalidation or recredentialing every few years to maintain your active status.
Verify Patient Eligibility
After you’re enrolled, the next step is confirming whether a patient has active Medicaid coverage. This must be done before every appointment. Medicaid eligibility can change from month to month, so never assume that a patient who was covered last time still has valid coverage.
You can check a patient’s Medicaid status using your state’s online portal, a billing software tool, or a third-party clearinghouse. Confirming eligibility in advance prevents claim denials and ensures that you’re offering services that are actually reimbursable.
Understand Billing Requirements and Coding
Once you’ve confirmed a patient is eligible, you need to make sure the service you’re providing is covered under Medicaid and that you're using the right billing codes. Medicaid uses standard CPT, HCPCS, and ICD-10 codes, but some codes may be restricted or require prior authorization. Each state publishes a Medicaid fee schedule that outlines the reimbursable codes and the amount paid for each service.
Using the correct combination of diagnosis and procedure codes is critical. A simple error can cause your claim to be denied or delayed. You should also check whether any modifiers are required and whether the procedure needs to be linked to a specific diagnosis.
Document Services in Detail
Accurate documentation is the foundation of successful billing. After every patient visit, make sure your notes clearly reflect what services were performed, why they were medically necessary, and how much time was spent (if applicable).
This documentation should include the patient’s symptoms, diagnoses, treatment plan, procedures performed, and any referrals or follow-up instructions. If your state requires it, include prior authorization numbers or attach any supporting documents. Good documentation doesn’t just support your billing it also protects you in case of audits or claim reviews.
Submit Your Claims
Once documentation is complete, you’re ready to submit your Medicaid claim. Most states prefer electronic claim submissions, which are faster and easier to track. Electronic claims can be submitted through your practice management software, a clearinghouse, or your state’s Medicaid provider portal. Some providers still use paper claim forms, such as the CMS-1500 or UB-04, but these take longer to process.
When preparing the claim, be sure to include the patient's Medicaid ID, the date of service, your provider ID, the correct procedure and diagnosis codes, and the appropriate charges. Double-check all details to avoid simple errors that can lead to denials or payment delays.
Track Claim Status and Payments
Submitting a claim isn’t the end of the process. You need to actively follow up to make sure your claim is being processed. Most Medicaid programs offer tools that let you check claim status online. You’ll be able to see if the claim was accepted, rejected, or paid.
It’s important to review your remittance advice or explanation of benefits (EOB) carefully. If something was denied or underpaid, the EOB will include a reason code that explains what went wrong.
Correct and Resubmit Denied Claims
Even when you do everything right, some Medicaid claims may still get denied. The most common reasons include incorrect codes, missing documentation, invalid patient eligibility, or incomplete provider credentialing. Don’t ignore these rejections each one represents lost revenue.
To fix a denied claim, first review the denial reason. Then make the necessary corrections, add any missing information, and resubmit the claim. Most states allow resubmission within a certain time window, so act quickly. In some cases, you may need to file an appeal if the denial was based on medical necessity or another complex issue.
Stay Compliant with Medicaid Regulations
Billing Medicaid isn’t just about submitting claims it also requires ongoing compliance. Each state sets its own rules for documentation, coding, and recordkeeping. You must keep patient records for a set number of years, follow HIPAA privacy laws, and stay current with state billing updates.
Some states also require providers to complete annual compliance training or update their credentials regularly. Staying compliant not only helps you get paid, but also protects your practice from audits, fines, or even removal from the Medicaid program.
Consider Outsourcing Your Medicaid Billing
Conclusion
Learning how to bill Medicaid as a provider can seem intimidating at first, but once you understand the process, it becomes manageable. Start by enrolling, check eligibility before each visit, use accurate coding, document everything thoroughly, and follow up on each claim. With the right system in place, you’ll reduce denials, get paid faster, and stay compliant with state regulations.
Whether you handle billing in-house or outsource it, this step-by-step approach will help you build a strong Medicaid billing workflow that supports your practice and your patients. Get a free consultation with PROMBS today and let our team simplify your Medicaid billing while helping you avoid audits, denials, and documentation issues.