What Is Panic Disorder?
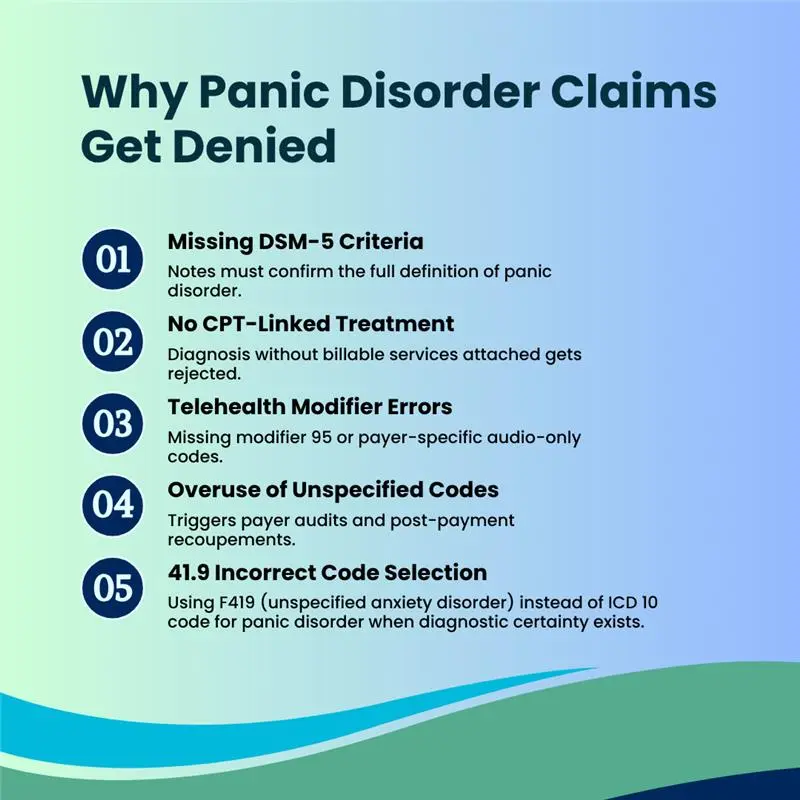
Why Panic Disorder Claims Get Denied
Panic disorder claims are highly scrutinized by payers in 2025, with even minor coding or documentation errors leading to denials, delays, or post-payment audits. Understanding the most common denial triggers allows providers and billing teams to proactively address gaps, maintain compliance, and protect revenue integrity.
DSM-5 diagnostic criteria require:
- Recurrent unexpected panic attacks without a situational trigger.
- At least one month of concern, avoidance, or behavioral change after attacks.
- No symptoms attributable to substances or other medical conditions.
- Not better explained by another mental disorder.
Accurate documentation is critical. Without it, even correctly assigning the ICD 10 code for panic disorder (F41.0) can lead to denials.
Primary ICD-10 Code for Panic Disorder
| ICD-10 Code | Description | When to Use |
|---|---|---|
| F41.0 | Panic disorder [episodic paroxysmal anxiety] | When all DSM-5 criteria are met and no medical cause exists. |
Use F41.1 or F41.9 only when panic-specific criteria are not met. Overusing unspecified codes instead of the ICD 10 code for panic disorder (F41.0) increases denial risk.
Subcategories & Related ICD-10 Codes
| ICD-10 Code | Description | Usage Notes |
|---|---|---|
| F41.0 | Panic disorder (episodic paroxysmal anxiety) | Primary diagnosis for confirmed panic disorder |
| F41.1 | Generalized anxiety disorder | Not for discrete panic episodes |
| F41.8 | Other specified anxiety disorders | For atypical anxiety |
| F41.9 | Unspecified anxiety disorder | Avoid unless documentation is incomplete |
Important: F41.1 (Generalized anxiety disorder) should never be used to bypass missing panic disorder documentation, it’s clinically distinct.
Clinical Documentation Requirements for F41.0
To prevent denials when using the ICD 10 code for panic disorder (F41.0), documentation must:
- Cite DSM-5 criteria met by the patient.
- Include onset date and attack frequency.
- Show functional impact (work, social, daily life).
- Rule out medical causes.
- Link diagnosis to treatment (therapy, medication, or both).
Relevant CPT Codes for Panic Disorder Billing
| CPT Code | Service Description |
|---|---|
| 90791 | Psychiatric diagnostic evaluation |
| 90832 | Psychotherapy, 30 min |
| 90834 | Psychotherapy, 45 min |
| 90837 | Psychotherapy, 60 min |
| 99213–99215 | E/M visits with medical management |
| 99417 | Prolonged outpatient visit |
| G2012 | Virtual check-in |
Always apply modifier 95 for telehealth and verify POS codes when billing the ICD 10 code for panic disorder (F41.0).
Telehealth Modifier Note: Modifier 95 is correct, but some payers in 2025 have shifted to POS 10 (telehealth home) or POS 02 (telehealth other). This distinction is important to prevent denials.
Payer Policy Insights for Panic Disorder Claims
Payers such as BCBS, Aetna, and UnitedHealthcare require that claims for the ICD 10 code for panic disorder (F41.0) include full DSM-5 criteria documentation, with a clear link between the patient’s functional impairment and the established medical necessity for treatment. They also expect to see evidence-based treatment plans such as cognitive behavioral therapy (CBT) or pharmacotherapy along with detailed, ongoing progress notes that demonstrate either improvement or justified modifications to the care plan.
Medicare similarly covers panic disorder services under its mental health benefits, but it enforces strict incident-to billing rules for certain provider types. This means that services billed under a supervising provider’s NPI must meet specific supervision and documentation requirements, making compliance critical to avoid claim denials or post-payment audits.
Why Using F41.0 Correctly Matters in 2025
Using the ICD 10 code for panic disorder (F41.0) correctly in 2025 is more than just a compliance step, it plays a critical role in protecting revenue and reducing audit exposure. Specific codes like F41.0 help prevent claims from being flagged by payer audit systems, which increasingly target nonspecific or vague diagnoses such as F41.9. By meeting the highest level of diagnostic specificity, providers reduce the likelihood of prepayment reviews, post-payment recoupments, and other costly administrative interventions. This accuracy also prevents downcoding, where claims are reimbursed at a lower rate due to insufficient detail, ultimately speeding up payment cycles and ensuring cleaner claim submissions.
Beyond compliance and payment speed, correct use of the ICD 10 code for panic disorder (F41.0) also improves the quality of data used in population health reporting, payer quality measures, and internal analytics. Accurate coding allows providers to track treatment outcomes more effectively, measure the success of interventions, and meet requirements for value-based care programs. This not only enhances patient care but also strengthens a provider’s ability to secure favorable contracts and participate in performance-based reimbursement models. In short, coding F41.0 accurately supports both financial stability and clinical excellence.
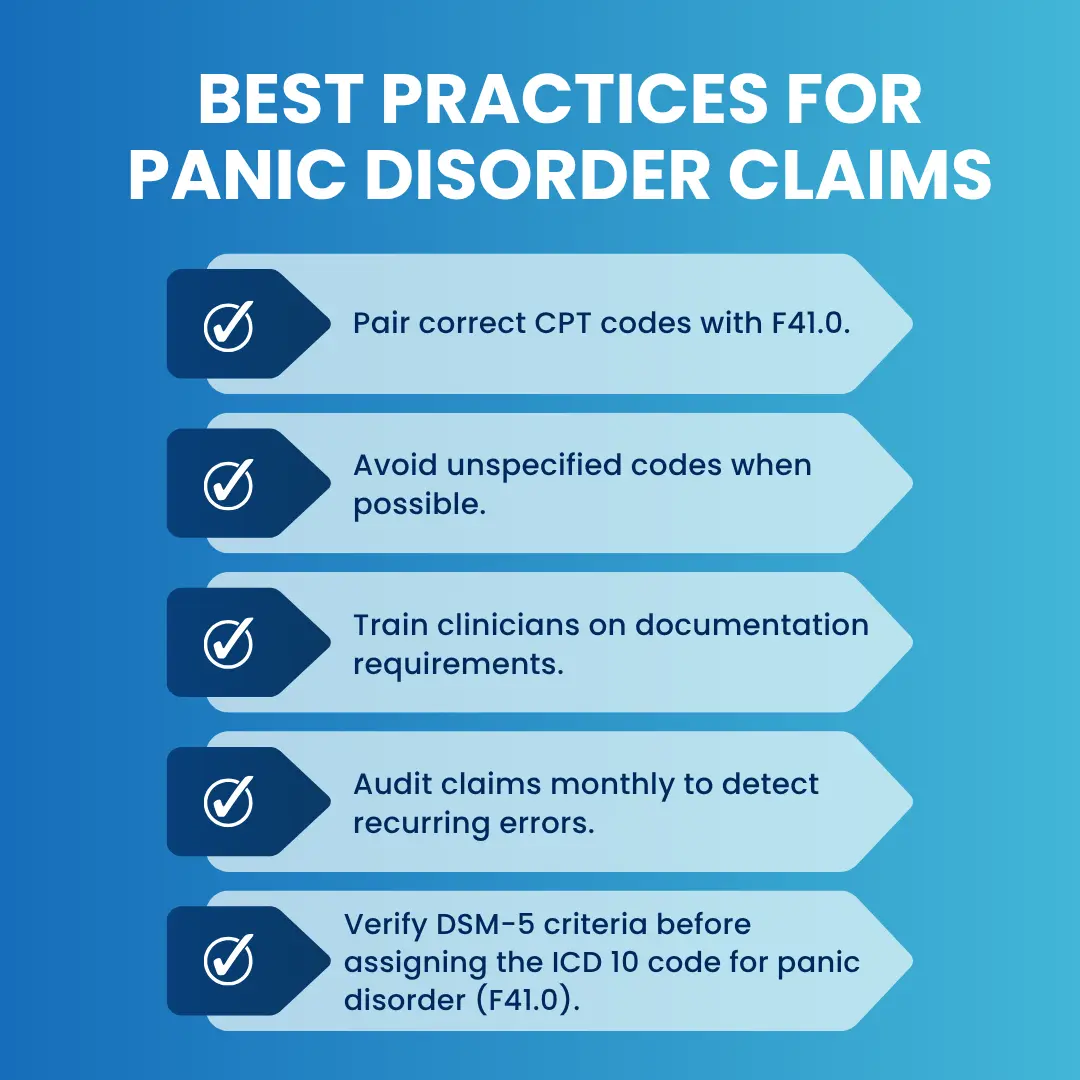
Best Practices for Panic Disorder Claims
How Pro-MBS Helps with Panic Disorder Billing
Pro-MBS applies a compliance-driven approach to managing claims involving the ICD 10 code for panic disorder (F41.0), ensuring they meet the highest technical and regulatory standards. Each claim is thoroughly reviewed for full DSM-5 criteria documentation, accurately paired with the appropriate CPT codes, and supported with correct modifier usage to satisfy payer-specific requirements.
Our team continuously monitors denial trends, applying proactive strategies to address payer edits before submission. This rigorous process enables behavioral health providers to minimize claim rejections, accelerate reimbursement cycles, and maintain strict adherence to evolving 2025 payer compliance guidelines.