Chronic respiratory failure ICD 10 coding is a critical component in ensuring accurate reimbursement and avoiding claim denials. As healthcare systems increasingly rely on value-based care models and payer audits, precise chronic respiratory failure ICD 10 coding becomes essential for both compliance and securing appropriate reimbursement.
Given the complexity of chronic respiratory failure, which often involves long-term management due to underlying conditions like obstructive lung diseases, neuromuscular disorders, or thoracic cage abnormalities, coding errors can lead to significant administrative setbacks and financial losses.
Understanding and accurately applying the chronic respiratory failure ICD 10 code ensures that healthcare providers are compensated for the resources used in managing these complex conditions while maintaining compliance with regulatory standards.
What is Chronic Respiratory Failure ICD 10?
Chronic respiratory failure occurs when the respiratory system fails to maintain adequate gas exchange over a prolonged period. This condition is often caused by obstructive lung diseases, neuromuscular disorders, or thoracic cage abnormalities.
Symptoms like fatigue, dyspnea, cyanosis, and morning headaches are common, largely due to hypoxemia (low oxygen) or hypercapnia (high carbon dioxide).
Unlike acute respiratory failure, which demands immediate medical intervention, chronic respiratory failure requires long-term management, often through non-invasive ventilation or oxygen therapy. Accurate diagnosis and coding are vital to ensure patients receive the correct care and that providers are reimbursed appropriately.
What Are the ICD-10 Codes for Chronic Respiratory Failure?
The chronic respiratory failure ICD 10 codes fall under the J96 category, with different sub-codes to capture the condition's specifics.
| ICD-10 Code | Description | Use Case Example |
|---|---|---|
| J96.10 | Chronic respiratory failure, unspecified | Documentation lacks specifics on hypoxia/hypercapnia |
| J96.11 | Chronic respiratory failure with hypoxia | Chronic low oxygen saturation, long-term O2 use |
| J96.12 | Chronic respiratory failure with hypercapnia | Elevated CO₂ on ABG, especially in COPD patients |
| J96.21 | Acute and chronic respiratory failure with hypoxia | Acute exacerbation of chronic failure with hypoxia |
| Z99.81 | Dependence on supplemental oxygen | Long-term oxygen dependence documented |
| Z99.11 | Dependence on respirator (ventilator) status | Chronic ventilator dependence |
Note:
J96.21 is a combination code used for acute exacerbations of chronic respiratory failure with hypoxia. It should be used instead of chronic-only codes (J96.10–J96.12) when both conditions are present.
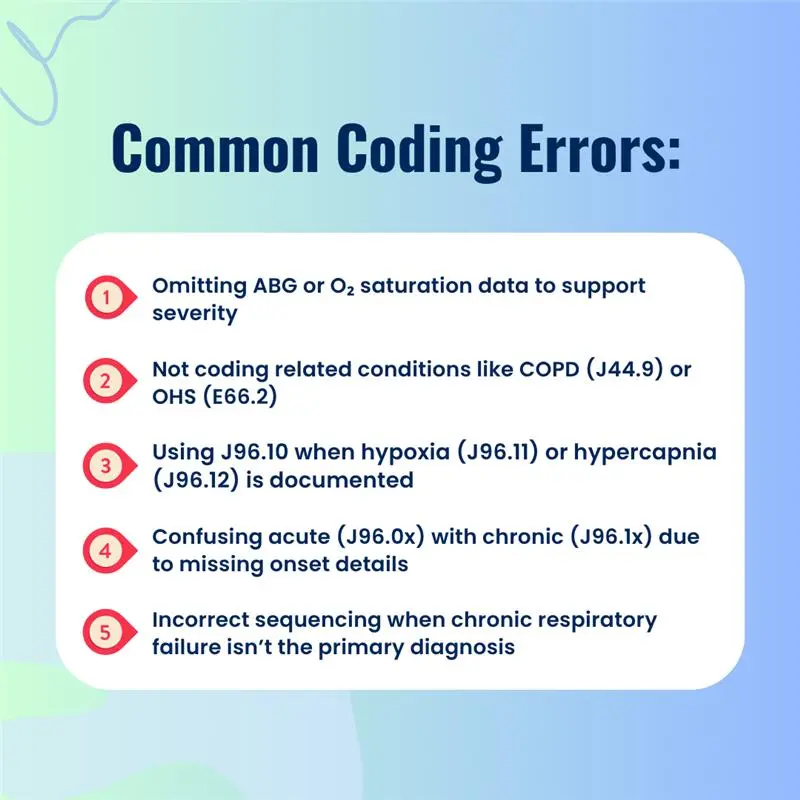
How to Avoid Common Chronic Respiratory Failure ICD 10 Coding Errors?
- Misidentifying Acute vs. Chronic Respiratory Failure
Chronic respiratory failure develops gradually, while acute failure presents suddenly. Incorrectly identifying an acute condition as chronic (or vice versa) is a frequent coding error. Always assess the patient's history and clinical documentation to ensure correct classification.
- Lack of Specificity
The most common coding error is using the unspecified code J96.10 due to insufficient documentation. If the provider doesn't specify hypoxia or hypercapnia, the default is J96.10, but it's crucial to query the physician for more details. For instance:
- J96.11 should be used when chronic hypoxemia is present, as documented by oxygen saturation levels consistently below 88% or PaO2 <55–60 mmHg.
- J96.12 is appropriate when hypercapnia is observed (PaCO2 >45 mmHg), and the pH is typically near normal (7.35–7.45) despite the high CO₂. If the pH is low, it is likely Acute on Chronic Respiratory Failure ICD 10 (J96.22).
- Failing to Capture Comorbidities
Chronic respiratory failure often coexists with conditions like COPD, obesity hypoventilation syndrome, and heart failure. Each must be coded separately, but their clinical significance must guide sequencing. If COPD is the primary condition, it should be sequenced before the respiratory failure code. Make sure to use J44.9 (COPD) alongside J96.1 or J96.10–J96.12 for accurate reporting.
How Does Acute on Chronic Respiratory Failure ICD 10 Impact Coding?
- Code Selection: Use J96.10 for unspecified cases, J96.11 for hypoxia, and J96.12 for hypercapnia.
- Acute on Chronic: J96.21 should be used for acute exacerbations of chronic respiratory failure, as it impacts DRG assignment.
- Clinical Correlation: Always correlate with clinical markers like ABGs, oxygen saturation, and imaging results.
- Comorbidities: Ensure correct sequencing when chronic respiratory failure coexists with other conditions like COPD or heart failure.
Note:
J96.21 (Acute and chronic respiratory failure with hypoxia) is an MCC (Major Complication or Comorbidity), significantly increasing the DRG weight compared to standard chronic codes like J96.10–J96.12.
What Are the Best Practices for Chronic Respiratory Failure ICD 10 Coding?
- Query Providers for Missing Details: If documentation is vague, always request clarification.
- Correct Code Sequencing: Follow ICD-10-CM Official Guidelines for sequencing, typically coding the underlying etiology (like COPD or MD) as the principal diagnosis unless the respiratory failure is the reason for the encounter.
- Use Specific Codes for Hypoxia/Hypercapnia: Always specify whether the patient is experiencing hypoxia or hypercapnia as part of the chronic respiratory failure diagnosis.
- Clinical Validation: Ensure the medical record doesn't just list the code but describes the treatment. For example, documenting 'Chronic Respiratory Failure' but not showing the patient is on home oxygen or a ventilator can lead to a 'Clinical Validation Denial' where the payer removes the code entirely.
How Does Chronic Respiratory Failure ICD 10 Affect Reimbursement?
The accurate selection of the ICD 10 code for chronic respiratory failure directly impacts reimbursement. Codes such as J96.11 and J96.12 are categorized as CCs (Complications or Comorbidities), while J96.21 (Acute on Chronic) is an MCC (Major CC). This distinction is the primary driver of DRG shifts and higher reimbursement.
By capturing these details, healthcare providers ensure proper reimbursement while promoting better clinical care for patients.
How Does Pro-MBS Ensure Accurate Chronic Respiratory Failure ICD 10 Coding?
At Pro-MBS, we understand that chronic respiratory failure ICD 10 coding is a complex and critical task. Our certified coders work closely with healthcare providers to ensure all clinical indicators, including hypoxia and hypercapnia, are accurately captured.
We apply payer-specific guidelines, adhere to DRG optimization strategies, and use clinical documentation improvement (CDI) protocols to ensure compliance, mitigate denials, and protect revenue integrity.
Frequently Asked Questions
What is Chronic Respiratory Failure ICD 10, and why is it important?
Chronic respiratory failure ICD 10 codes are vital for accurate reimbursement. These codes help differentiate between chronic and acute conditions. Proper coding ensures compliance and prevents claim denials, ensuring healthcare providers are paid for managing complex respiratory conditions like COPD or neuromuscular disorders.
What are the most common coding errors in Chronic Respiratory Failure ICD 10?
Common errors include misidentifying acute vs. chronic failure and using the unspecified code J96.10 when documentation lacks details. Accurate coding of chronic hypoxemic respiratory failure ICD 10 requires specifying hypoxia or hypercapnia to ensure proper reimbursement and avoid denials.
How does acute on chronic respiratory failure affect ICD 10 coding?
Acute on chronic respiratory failure ICD 10 requires J96.21 as a combination code, replacing chronic-only codes. Using J96.21 ensures proper DRG assignment and higher reimbursement by reflecting both conditions' complexity in the patient’s diagnosis.
How can clinical validation affect Chronic Respiratory Failure ICD 10 coding?
Clinical validation ensures that codes like J96.11 for hypoxia are supported by treatment details, such as oxygen therapy. Without validation, payers may deny claims, highlighting the importance of comprehensive documentation to prevent clinical validation denials and ensure accurate reimbursement.