Introduction
In today’s healthcare environment, efficient practice operations rely on seamless coordination between administrative systems and clinical systems. The Practice Management System (PMS) handles the financial and operational side of a practice, while the Electronic Health Record (EHR) focuses on patient care and clinical documentation.
When PMS and EHR systems are fully integrated, they streamline workflows, improve coding accuracy, enhance compliance, and reduce revenue leakage. For healthcare providers, coders, and administrators, understanding how PMS interacts with EHR is essential for optimizing both revenue cycle management and patient care.
Coders and healthcare providers must work together to ensure that documentation is both thorough and clinically justified. This blog provides a technical roadmap to help mitigate denials through precise code usage, detailed clinical correlation, and proper claim sequencing. to help mitigate denials through precise code usage, detailed clinical documentation, and proper claim sequencing.
Understanding PMS (Practice Management System)
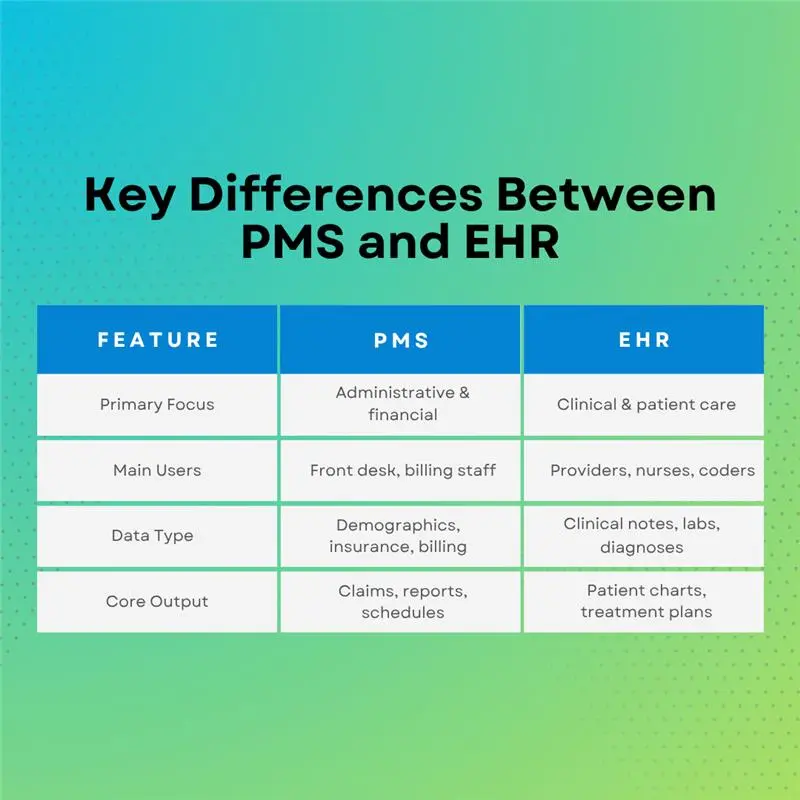
A PMS is primarily an administrative and billing platform designed to manage the non-clinical operations of a medical practice.
Core Functions Include:
- Scheduling & Appointment Management: Tracks patient appointments, provider availability, and room assignments.
- Insurance Eligibility & Verification: Confirms coverage before visits to avoid claim rejections.
- Medical Billing & Coding Support: Generates claims, applies CPT/ICD codes, and submits to payers.
- Reporting & Analytics: Produces revenue cycle KPIs, denial reports, and productivity metrics.
Types of PMS:
| Type | Description | Pros | Cons |
|---|---|---|---|
| On-Premise | Installed locally within practice servers | High control, data stored internally | High upfront costs, maintenance burden |
| Cloud-Based | Hosted online, accessible from anywhere | Scalability, lower maintenance | Dependent on internet, subscription costs |
| Hybrid | Mix of on-premise and cloud | Flexibility, redundancy | More complex to manage |
Understanding EHR (Electronic Health Record)
An EHR is a clinical information system that stores and manages patient health data.
Key Capabilities Include:
- Comprehensive Patient Records: Includes medical history, allergies, medications, lab results, imaging, and clinical notes.
- Clinical Decision Support: Alerts providers to drug interactions, abnormal lab results, or preventive care needs.
- Order Entry & Result Tracking: Facilitates e-prescriptions, lab orders, and result reporting.
- Care Coordination: Shares data across providers and facilities to ensure continuity of care.
From a coder’s perspective, EHR documentation is the primary source for assigning ICD-10-CM, CPT, and HCPCS codes making its accuracy critical for compliance and reimbursement.
Key Differences Between PMS and HER
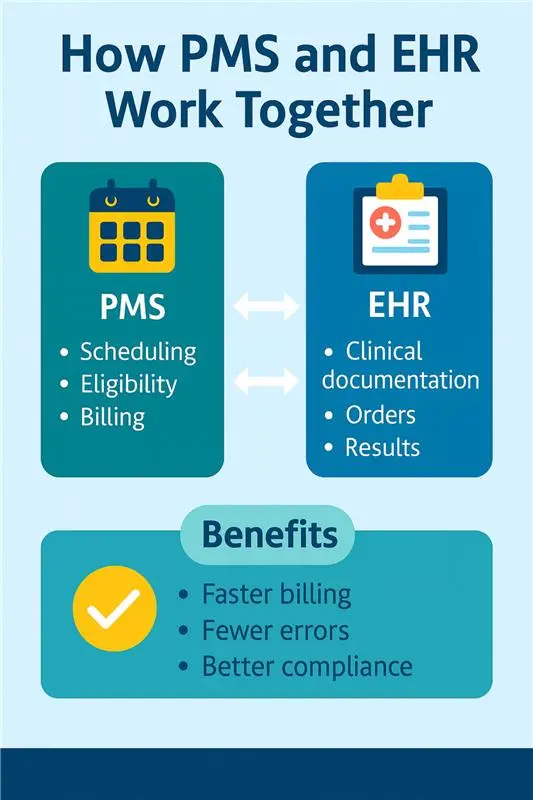
Why Integration Matters
When PMS and EHR operate in silos, duplicate data entry, coding inconsistencies, and billing delays occur. Integration:
- Ensures real-time synchronization of demographic, clinical, and billing data.
- Reduces errors by eliminating manual re-entry.
- Improves coding specificity since coders can directly access the clinical details from the EHR in the PMS claim creation process.
- Enhances patient satisfaction with smoother scheduling, billing, and care coordination.
How PMS Interacts with EHR
Key Interaction Points:
- Patient Demographics – Entered once in PMS, synced to EHR for clinical use.
- Appointment Scheduling – PMS updates provider schedules in EHR, triggering clinical prep.
- Clinical Documentation to Billing – EHR visit notes populate PMS billing modules with ICD-10 and CPT codes.
- Claim Submission – PMS sends claims to payers using codes pulled from EHR documentation.
- Payment Posting & AR – Payments posted in PMS, linked back to clinical encounters in EHR for tracking.
Example Workflow:
PMS: Schedules patient → Verifies insurance → Generates encounter ID.
EHR: Provider documents visit, selects ICD-10 and CPT codes.
PMS: Pulls codes → Creates claim → Submits to payer → Posts payment.
⚠ Coding Impact Considerations:
- Risk of Code Mismatches – Poorly configured integration can cause ICD-10 or CPT codes to transfer incorrectly, leading to denials or compliance flags.
- Real-Time Code Mapping – When PMS and EHR exchange coding data instantly, coders can validate diagnosis-procedure linkage, improving DRG optimization and risk adjustment accuracy.
Compliance, Security, and Interoperability
- HIPAA Compliance: All Protected Health Information (PHI) exchanged between the PMS and EHR must be encrypted and transmitted securely to prevent unauthorized access. This includes both real-time data transfers and stored records.
- HL7 / FHIR Standards: Health Level Seven (HL7) and Fast Healthcare Interoperability Resources (FHIR) protocols provide the framework for standardized, interoperable data exchange ensuring that patient demographics, scheduling, billing, and clinical records flow accurately between systems without manual re-entry.
- Audit Trail Requirements: Both PMS and EHR platforms must maintain comprehensive audit logs capturing every instance of access, modification, or transmission of data. These logs are essential for compliance monitoring and responding to regulatory inquiries.
From a medical coding and billing perspective, synchronized and secure PMS–EHR integration is not just operationally efficient, it is a compliance safeguard.
Payer Audit Angle:
- Many payers check for date mismatches between PMS billing entries and EHR documentation timestamps, flagging any discrepancies as potential compliance risks.
- Some Medicare Administrative Contractors (MACs) require that high-dollar CPT codes be backed by EHR-sourced documentation before payment is approved, making accurate, synchronized data critical.
Conclusion
For modern healthcare organizations, PMS–EHR integration is not just a convenience, it is a critical safeguard for both revenue integrity and regulatory compliance. A well-synced EHR ensures that every clinical note, diagnosis, and test result is accurately documented, while the PMS translates that clinical data into precise claims, eligibility checks, and payment postings. This seamless exchange eliminates duplicate data entry, reduces the likelihood of coding and billing errors, and ensures that claims are supported by robust, audit-ready documentation.
From a coding and billing perspective, the value is clear: accurate coding starts with accurate data. When PMS and EHR systems communicate flawlessly, coders have the complete clinical context, and billers have the exact financial details needed to submit clean claims on the first pass. The result is faster reimbursements, fewer denials, improved compliance, and a stronger overall revenue cycle while also supporting better continuity of care for patients.