What Is a Medical Billing Company and What Services Do They Provide?
A medical billing company plays a far more complex role than simply submitting claims to payers. The best medical billing companies deliver end-to-end medical billing services that include medical claims processing, denial management services, credentialing support, and complete RCM services for doctors. These functions are essential for practices that want to maintain compliance, reduce administrative burden, and secure consistent reimbursements.
Beyond traditional claim submission, a strong partner provides integrated practice management solutions that streamline workflows across scheduling, eligibility verification, and reporting. Many leading vendors in medical billing outsourcing also deploy advanced billing software for healthcare that connects seamlessly with EHR systems. By leveraging HIPAA-compliant billing services and compliance monitoring, these companies not only safeguard patient information but also improve overall healthcare revenue cycle management. For providers exploring how to choose the best medical billing company for your practice, the depth and breadth of these services are critical factors in driving cash flow stability.
How to Choose the Best Medical Billing Company for Your Practice
Selecting the right medical billing company can transform the financial health of your practice. With ever-changing payer rules, compliance requirements, and complex reimbursement policies, healthcare providers must carefully evaluate whether to manage billing in-house or partner with an external vendor. A well-chosen partner in medical billing services not only streamlines healthcare revenue cycle management but also enhances patient satisfaction and operational efficiency.
Benefits of Outsourcing Medical Billing
Outsourcing to a professional medical billing company offers practices measurable financial and operational advantages. One of the primary benefits is cost efficiency, practices no longer need to maintain full in-house billing departments, cutting expenses tied to salaries, training, software, and compliance management. With outsourced medical billing services, providers gain access to expert coders, advanced billing software for healthcare, and real-time reporting systems that improve accuracy in medical claims processing. This not only lowers administrative overhead but also accelerates reimbursements and stabilizes cash flow.
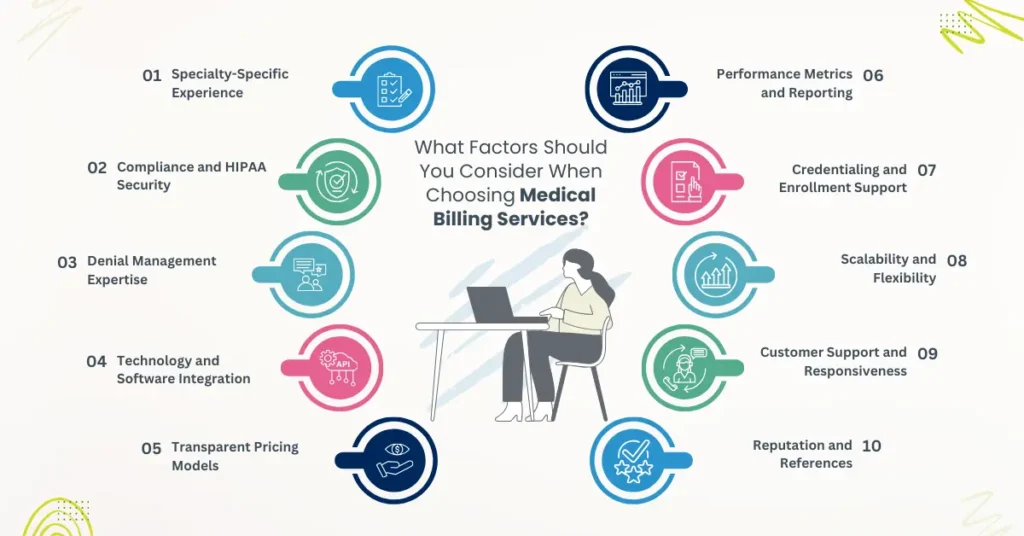
What Factors Should You Consider When Choosing Medical Billing Services?
Outsourced Medical Billing offers several measurable benefits that impact both financial performance and operational efficiency. Below is a detailed breakdown of the advantages providers typically experience when choosing Outsourced Medical Billing Services over in-house billing models.
1. Specialty-Specific Experience
When evaluating a medical billing company, one of the most critical factors is its familiarity with your specialty. Different specialties such as cardiology, gastroenterology, or behavioral health have unique coding challenges, payer rules, and reimbursement patterns.
For example:
- Oncology billing requires precise coding of chemotherapy and infusion services (CPT 96413, 96415, etc.), where even a small modifier error can result in denials.
- Gastroenterology billing often involves the correct application of modifiers for endoscopic procedures (e.g., CPT 45378–45385) to prevent bundling denials.
- Cardiology billing has payer-specific coverage nuances for procedures like echocardiograms (CPT 93306) and stress tests (CPT 93015), requiring detailed documentation to support medical necessity.
A partner already equipped with workflows, coding protocols, and payer-specific edits for your specialty ensures cleaner claims, fewer denials, and maximum reimbursements. This expertise is especially valuable for providers looking to select a billing company that can manage complex procedure codes with confidence.
2. Compliance and HIPAA Security
A reputable billing partner must provide HIPAA-compliant billing services with strong data security frameworks. Compliance failures not only expose practices to legal risks but also compromise patient trust. The best medical billing services for small practices and large groups alike include strict protocols for PHI protection, encrypted transmissions, and adherence to federal guidelines.
When you choose a medical billing company, always confirm its compliance certifications and security audits. A vendor’s ability to maintain safe handling of sensitive data is non-negotiable in today’s environment of increasing cybersecurity threats.
3. Denial Management Expertise
Effective denial management services are a hallmark of the best medical billing company. Denials often stem from coding errors, missing documentation, or payer-specific rules. An experienced vendor should not only resubmit claims but also provide root-cause analysis and workflow improvements to prevent repeat issues.
For practices evaluating factors to consider before outsourcing medical billing, denial management expertise is essential. A company that consistently reduces denials directly improves collections and strengthens overall healthcare revenue cycle management.
4. Technology and Software Integration
Modern medical billing services depend heavily on robust technology. The vendor you select should offer billing software for healthcare that integrates seamlessly with your EHR and practice management system. Features such as claim scrubbing, eligibility verification, and automated reporting accelerate workflows and minimize human error.
When analyzing how to evaluate a medical billing company’s performance, ask about its technology stack and integration capabilities. The best medical billing company provides real-time dashboards and analytics to help providers monitor claims and revenue cycle performance.
5. Transparent Pricing Models
Pricing structures among medical billing companies for private practices vary. Most charge a percentage of monthly collections, usually within the 4%–10% range, while others may use flat-fee models.
It’s important to understand how this range applies:
- 4–6% is standard for larger practices with high claim volume.
- 7–10% is more common for small practices or complex specialties such as oncology or behavioral health, where coding and payer rules demand more effort.
Practices should look for transparency, with no hidden costs or charges that cut into profitability. When determining how to choose the best medical billing company for your practice, evaluate whether the cost aligns with the value delivered. Affordable models exist, but the focus should remain on compliance, accuracy, and improved cash flow rather than price alone.
6. Performance Metrics and Reporting
One of the factors to consider before outsourcing medical billing is the reporting capability of the vendor. Metrics such as first-pass claim acceptance rate, AR days, and denial percentages are essential to measure efficiency. A vendor unwilling to provide clear reporting may not deliver consistent performance.
By selecting a medical billing company that provides regular, detailed reports, practices gain transparency into their revenue cycle. This enables providers to track progress, adjust workflows, and hold vendors accountable.
7. Credentialing and Enrollment Support
In addition to medical billing services, many vendors also offer credentialing services to help providers get enrolled with insurance networks. Credentialing errors can delay reimbursements and prevent providers from receiving payment for services.
While some firms include credentialing support as part of a bundled practice management solution, in many cases it is treated as a separate, add-on service with its own fee structure. Practices should confirm whether credentialing is included or billed separately before choosing a vendor.
The best medical billing company ensures credentialing workflows are accurate and timely, so new providers are onboarded quickly and time-to-revenue is minimized.
8. Scalability and Flexibility
A strong billing partner should adapt as your practice grows. Whether you expand to multiple locations, add providers, or increase patient volume, the vendor must scale without disrupting operations. Outsourced medical billing services offer flexibility that in-house billing teams often cannot match.
For practices comparing choosing between in-house and outsourced medical billing, scalability is a decisive factor. The ability to expand seamlessly ensures that the vendor remains a long-term partner rather than a temporary solution.
9. Customer Support and Responsiveness
Communication is often overlooked but critical when selecting the best medical billing company. A dedicated account manager, regular updates, and fast responses to queries help practices resolve claim issues quickly and avoid revenue delays.
Providers looking for what to look for in a medical billing company should evaluate client support quality as much as technical expertise. Responsive service ensures billing errors are corrected before they affect revenue cycle outcomes.
10. Reputation and References
Finally, a company’s reputation is one of the most reliable indicators of quality. Ask for references, review case studies, and check client testimonials. Industry-recognized firms with proven track records are safer choices than untested providers.
For practices seeking affordable medical billing services for doctors, reputation is as important as pricing. Choosing a trusted partner ensures stability, compliance, and measurable improvements in RCM services for doctors.
Why Choose Pro-MBS as Your Medical Billing Company
Selecting the right billing partner is often the difference between a stable revenue cycle and one burdened by denials, payment delays, and compliance risks. Our Pro-MBS team partners with practices to optimize every stage of the revenue cycle from accurate claims processing to denial prevention, credentialing, and compliance oversight. We bring proven expertise across multiple specialties, delivering scalable, technology-enabled solutions tailored to your unique workflow.
With Pro-MBS, practices gain measurable results:
- Boost revenue by up to 30%
- Achieve 98.9% first-pass acceptance
- Recover aged AR, even 120+ days old
- Get 24/7 support from certified experts
For providers evaluating how to choose the best medical billing company in 2025, Pro-MBS offers a consultative approach that combines industry expertise, transparent reporting, and measurable financial outcomes ensuring revenue integrity and long-term growth.