Many labs still rely on paper-based credentialing and claim submission. In previous CMS rollouts, this delay caused weeks of claim denials and disrupted cash flow. The upcoming CLIA paperless mandate is not just a compliance update. It is a critical turning point for labs that want to avoid costly denials and keep reimbursements flowing.
As per the Centers for Medicare & Medicaid Services (CMS), all Clinical Laboratory Improvement Amendments (CLIA) processes will transition to a fully paperless model by 2026. According to the CMS CLIA Modernization Roadmap (2024), this shift is not just a technical upgrade but fundamentally changes how credentialing, billing, and payer communication must be managed.
For revenue cycle teams, this means re-engineering workflows to align with electronic documentation and audit-ready data exchange. Providers, billers, and coders who prepare early can mitigate claim delays and denials, while those relying on outdated manual processes risk compliance gaps and revenue disruption.
What Is the CLIA Paperless Transition?
The CLIA program ensures clinical labs meet federal standards for quality and accuracy. Historically, many CLIA processes including credentialing, updates, and billing compliance, have relied on paper documentation.
Starting in 2026, these processes will move to fully electronic systems. This affects:
- Credentialing and renewals now handled digitally.
- Billing and claim edits payers will expect electronic CLIA verification.
- Compliance checks automated flagging will replace manual paperwork.
This change matters because paper-based errors and delays often stall reimbursement. A fully digital process should increase efficiency, but only if staff are trained and systems are updated.
Why the CLIA Shift Matters in 2025?
The CLIA shift in 2025 is critical as labs must begin preparing for the 2026 paperless mandate. According to CMS’s CLIA page and the CLIA Transition to Paperless Toolkit (2025), early action ensures smooth reimbursement workflows, maintains certification compliance, and strengthens audit readiness.
Timely Reimbursement
The shift to a paperless CLIA system means payers will reject any claim missing the required digital CLIA details. Revenue cycle teams must ensure that these identifiers are captured and transmitted accurately within claims to prevent denials. Delays in updating workflows could lead to slower reimbursements and potential revenue loss.
Compliance for Certification
Laboratories will be required to follow the new electronic submission standards to maintain their CLIA certification. Failure to meet these requirements could result in compliance violations or even loss of certification, disrupting both patient care and revenue streams. Preparing in advance ensures a seamless transition without regulatory setbacks.
Audit Readiness
Paper-based records will no longer meet compliance expectations once the paperless system is in effect. Providers and billing teams will need to store and maintain electronic records that can be readily accessed during audits. Early adoption of compliant systems in 2025 will help organizations focus on Audit Readiness and reduce the risk of penalties or delayed payments.
The Biggest Workflow Shifts Labs Must Prepare For
The CLIA paperless transition 2026 introduces major operational changes that affect how labs handle credentialing, billing, and compliance. Understanding these changes below helps revenue cycle teams prepare their systems and avoid disruptions.
No More Paper Forms
All CLIA applications, renewals, and updates will move fully online. Laboratories will no longer be able to rely on mailed paper forms for regulatory actions, making early adoption of digital systems essential.
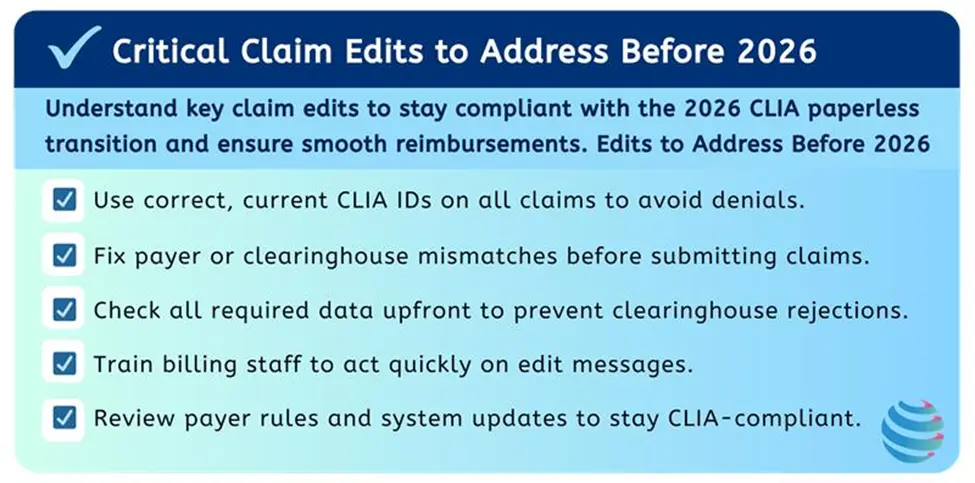
Electronic Payer Validation
Claims will need to include verifiable CLIA identifiers that can be electronically validated by payers. Missing or incorrect digital details will result in claim denials, highlighting the need for accurate integration of CLIA data into billing workflows.
Audit Trail Requirements
Digital logs will replace mailed paper forms as proof of compliance. Revenue cycle teams must ensure their systems can capture and store these logs in an accessible, audit-ready format to avoid compliance gaps.
Credentialing and Payer Updates for CLIA
Credentialing is one of the first areas to undergo significant change with the CLIA paperless transition 2026. This shift requires labs and revenue cycle teams to modernize their processes to ensure compliance and uninterrupted reimbursement.
Payers Will Only Accept Electronic CLIA Updates: All credentialing information must now be submitted through secure electronic channels instead of mailed paper forms. Labs that do not keep their CLIA details updated digitally risk delays in approval or outright claim denials, which can quickly affect reimbursement and cash flow.
Labs Must Integrate Payer Portals or Clearinghouses: To comply with the new paperless rules, labs need to connect their systems with payer portals or clearinghouses. These integrations make it easier to submit credentialing updates, check approval statuses in real time, and minimize errors that often occur in manual workflows.
Credentialing Specialists Must Track Digital Renewals Proactively: Keeping track of renewal dates and ensuring timely updates in payer portals is now essential. Missing even one update can lead to compliance issues, denied claims, and reimbursement delays. Designating a staff member to oversee these updates helps maintain accuracy and reduces the risk of revenue disruption.
How Should You Train Your Billing and Credentialing Teams?
Technology delivers results only when staff know how to use it effectively. Focus training on the key areas below to prepare for the paperless transition 2026.
| Training Area | Purpose | Outcome |
|---|---|---|
| Navigating Payer Credentialing Portals | Teach staff how to access and update payer systems efficiently. | Ensures timely and accurate CLIA updates, reducing risk of denials. |
| Handling Electronic Renewals | Show staff how to process renewals in a digital environment. | Keeps credentials current and prevents compliance lapses. |
| Interpreting Claim Edit Messages | Train billers to understand and act on edit flags from payers or clearinghouses. | Speeds up issue resolution and reduces payment delays. |
The Roadmap to Going Fully Paperless
Understanding the timeline is essential for labs, billing teams, and credentialing staff to prepare for a smooth transition.
Preparation Phase: Late 2024 to Early 2025
CMS begins releasing detailed guidance, and payers start testing electronic submission processes. This period sets the foundation for providers to assess their current workflows and prepare for upcoming requirements.
Early Transition Phase: Mid 2025
Credentialing updates must be submitted in digital format. Labs and billing teams need to adapt their workflows to ensure compliance with payer expectations.
Enforcement Phase: Early 2026
Payers start rejecting paper-based submissions. Claims missing required digital CLIA details face denials, emphasizing the need for complete adoption of the new system.
Full Implementation Phase: January 2026
All CLIA applications, renewals, and claims transition to the paperless model. Providers and billing teams must be fully compliant to maintain uninterrupted reimbursement.
In-House vs Outsourced Transition
| Aspect | In-House Billing | Outsourced Billing |
|---|---|---|
| Model | Advantages | Challenges |
| In-House | Greater control over workflows and compliance, direct oversight of staff. | Requires significant staff training, manual portal management, and higher resource investment. |
| Outsourced | Brings specialized expertise, advanced technology, and built-in compliance monitoring. | Less direct control, dependent on vendor performance and reporting. |
The Cost of Not Preparing
This paperless transition is more than a compliance update, it represents a complete overhaul of how revenue cycle teams manage credentialing, billing, and audits.
Failing to adapt in time could mean denied claims, certification risks, and serious cash flow disruptions. By proactively fixing credentialing workflows, strengthening claim edits, and training staff before the 2026 deadline, providers can safeguard compliance, prevent costly denials, and maintain financial stability.
Let Pro-MBS Handle Your Transition to CLIA 2026
The CLIA paperless transition is approaching quickly, and the cost of not preparing could mean months of denials, compliance issues, and disrupted cash flow. Pro-MBS supports providers and laboratories through our Credentialing and Compliance Services, helping them strengthen credentialing workflows, keep payer records current, and ensure staff are ready for the 2026 paperless mandate.
By leveraging our expertise, organizations can minimize denials, stay compliant with evolving payer rules, and maintain a smooth revenue cycle throughout the transition.
- See our Credentialing Services for CLIA compliance support.
- Explore our Denial Management Services.
FAQs
What is CLIA certification?
CLIA certification is the federal approval under the Clinical Laboratory Improvement Amendments (1988), administered by CMS to ensure labs meet quality and accuracy standards for human diagnostic testing. It is required for billing Medicare, Medicaid, and most commercial payers and depends on test complexity, with renewal every two years to maintain compliance and avoid claim denials.
What is the purpose of CLIA?
The Clinical Laboratory Improvement Amendments (CLIA) set federal quality standards for all U.S. laboratories that test human specimens. Its purpose is to ensure accuracy, reliability, and timeliness of lab results, regardless of lab size or specialty.
Why is CLIA transitioning to paperless by 2026?
Labs must apply for the correct certificate type, pay biennial CMS fees, and comply with federal quality standards. A valid CLIA number must be displayed and included on claims. Failure to comply can result in denials or loss of certification.
What happens if labs don’t prepare?
Failure to prepare could lead to denied claims, delays in credentialing renewals, and potential compliance violations. Labs that continue relying on paper processes risk cash flow disruptions and, in severe cases, loss of CLIA certification.
How can ProMBS help with CLIA readiness?
ProMBS provides end-to-end support, including denial management services, credentialing assistance, and full RCM optimization. By aligning workflows with the CLIA 2026 requirements, ProMBS helps labs stay compliant, reduce denials, and protect revenue.