Accurate ICD-10 coding is the foundation of clean claim submission and timely reimbursement. For obstetric and perinatal conditions, selecting the correct ICD-10-CM code is more than a routine administrative task; it directly influences maternal and neonatal care validation, payer approval, and overall revenue performance.
These conditions are frequently encountered in both outpatient and inpatient maternal care settings, yet miscoding often occurs due to incomplete provider documentation, insufficient specificity in clinical notes, or misunderstanding of the updated coding guidelines. Such errors not only delay payments but also expose practices to compliance risks and post-payment audits. Proper coding reduces denials, supports payer and regulatory compliance, and strengthens audit readiness by ensuring that claims accurately reflect the clinical scenario.
This guide provides a clear, step-by-step overview of the 2026 ICD-10-CM updates for obstetric and perinatal conditions, helping providers improve coding precision, enhance billing accuracy, and streamline reimbursement workflows while maintaining consistent documentation standards across care settings.
What Are the ICD-10 Obstetric and Perinatal Conditions and Symptoms for 2026?
Key Obstetric & Perinatal Conditions in ICD-10 for 2026
Obstetric and perinatal conditions include disorders and complications affecting the mother during pregnancy, delivery, and postpartum, as well as conditions affecting the fetus or newborn up to 28 days after birth.
Accurate identification and documentation of these conditions are critical for selecting the correct ICD-10-CM codes and ensuring compliant reimbursement.
- Gestational Hypertension: A pregnancy-induced hypertensive disorder that typically develops after 20 weeks of gestation; if unmanaged, it can progress to preeclampsia.
- Gestational Diabetes: A form of glucose intolerance arising during pregnancy, increasing risks for maternal complications and adverse neonatal outcomes such as macrosomia and delivery difficulties.
- Placenta Previa: A placental implantation disorder in which the placenta partially or completely covers the Cervical OS, heightening the risk of antepartum hemorrhage and delivery complications.
- Preeclampsia / Eclampsia: Hypertensive disorder with systemic organ involvement during pregnancy; eclampsia is defined by the presence of seizures and constitutes an obstetric emergency.
- Postpartum Hemorrhage: Excessive blood loss following childbirth that requires prompt clinical intervention to prevent severe maternal morbidity or mortality.
- Neonatal Jaundice: Hyperbilirubinemia in newborns presenting as yellow discoloration of the skin and sclera, often managed with phototherapy to prevent kernicterus.
- Neonatal Respiratory Distress: Breathing difficulty in neonates, frequently associated with prematurity, surfactant deficiency, or perinatal infection, requiring immediate respiratory support.
- Low Birth Weight: Defined as birth weight below 2,500 g, commonly linked to prematurity or maternal health complications, and associated with increased neonatal morbidity and mortality.
- Congenital Infections: Vertical transmission of infectious agents such as rubella or cytomegalovirus (CMV) from mother to fetus, leading to structural or functional neonatal disorders.
- Birth Injuries: Physical trauma sustained by the neonate during labor or delivery, including fractures, brachial plexus injuries, or soft-tissue damage.
Always use the ICD-10-CM 2026 guidelines for accurate coding and compliant reporting.
ICD-10 Symptoms for Obstetric & Perinatal Care
Symptoms are clinical signs seen in pregnant women, fetuses, or newborns that guide diagnosis and coding. Accurate documentation helps establish medical necessity and reduces claim denials.
- Vaginal Bleeding During Pregnancy: May signal serious obstetric complications such as miscarriage, placenta previa, or placental abruption and requires prompt evaluation.
- Hypertension or Gestational Diabetes: Common maternal disorders during pregnancy that necessitate close clinical monitoring to prevent adverse maternal and fetal outcomes.
- Preterm Labor Signs: Includes uterine contractions, cervical effacement or dilation, and leakage of amniotic fluid occurring before 37 weeks of gestation.
- Fetal Growth Restriction: A condition in which the fetus grows below expected percentiles for gestational age, typically identified through ultrasound assessment.
- Neonatal Respiratory Distress: Characterized by rapid or labored breathing in newborns, often due to surfactant deficiency, prematurity, or neonatal infection.
- Jaundice in Newborn: Yellow discoloration of the skin and sclera caused by elevated serum bilirubin levels, frequently requiring phototherapy to prevent complications such as kernicterus.
- Maternal Infections Impacting Fetus: Includes infections such as chorioamnionitis or toxoplasmosis that can compromise fetal development and lead to adverse pregnancy outcomes.
- Postpartum Complications: Conditions such as excessive bleeding (postpartum hemorrhage), infection, or persistent fever occurring after delivery, necessitating timely medical intervention.
Accurate documentation of these symptoms is essential for selecting the correct ICD-10-CM 2026 codes, ensuring medical necessity, and preventing claim denials.
Which ICD-10-CM Codes Cover Obstetric & Perinatal 2026?
| ICD-10-CM Code | Condition | Key Documentation Notes |
|---|---|---|
| O14.0 | Pre-eclampsia | For pregnancies with mild to moderate hypertension and proteinuria. Requires notes on gestational age and maternal condition. |
| O14.03 | Mild to Moderate Pre-eclampsia, Third Trimester | Use trimester-specific codes to indicate when the condition occurred. Accurate trimester reporting supports medical necessity validation. |
| O36.4XX_ | Intrauterine Death | For maternal care when pregnancy is complicated by fetal demise. Documentation must include gestational age and timing. |
| O80 | Normal Delivery | For full-term, uncomplicated deliveries. Must confirm absence of risk factors or complications. |
| P07.3 | Preterm Newborn | For infants born before 37 weeks when exact gestational age is not specified. Critical for neonatal reporting. |
| P22.0 | Respiratory Distress | For newborns with breathing problems due to lung immaturity. Requires clinical confirmation and detailed care notes. |
| P59.0 | Neonatal Jaundice | For jaundice in preterm infants. Documentation should include bilirubin levels, gestational age, and treatment details. |
Why Are These Codes Important for Billing?
Did You Know? 💡 Accurate ICD-10-CM and CPT® coding plays a pivotal role in reducing improper payment errors, which CMS reports at 7.38% in 2025. By ensuring precise code selection and thorough documentation, providers can significantly improve first-pass claim approvals, minimize costly denials, and maintain steady revenue flow.
When Should ICD-10 Obstetric & Perinatal 2026 Codes Be Used?
Use obstetric and perinatal codes as the primary diagnosis when:
- The patient encounter is directly related to pregnancy, delivery, or neonatal conditions.
- No more specific secondary diagnosis explains the clinical picture.
Do not use these codes when:
- The complication is clearly due to a different underlying medical condition.
- Documentation is vague or lacks clinical confirmation.
Correct sequencing of ICD-10-CM and CPT® codes is essential for meeting payer compliance requirements and securing accurate reimbursement. Proper order of primary and secondary diagnoses reduces the risk of claim rejections, minimizes audit exposure, and supports consistent revenue integrity across all encounters.
Related ICD-10 Codes for Obstetric & Perinatal Conditions – 2026
| ICD-10 Code | Description |
|---|---|
| O13 | Gestational hypertension without proteinuria |
| O24.4 | Gestational diabetes mellitus |
| O36.5XX_ | Maternal care for poor fetal growth |
| P05.1 | Small for gestational age |
| P59.9 | Neonatal jaundice, unspecified |
| P96.1 | Neonatal withdrawal symptoms from maternal drugs |
CPT Codes Commonly Paired with ICD-10 Obstetric & Perinatal Codes
CPT Codes Commonly Paired are procedure codes frequently linked with obstetric and perinatal ICD-10 diagnoses to document services like monitoring, delivery, and neonatal care for accurate billing.
| CPT Code | Description |
|---|---|
| 59400 | Routine obstetric care, vaginal delivery |
| 59510 | Cesarean delivery, including antepartum and postpartum care |
| 59610 | VBAC (Vaginal birth after C-section) |
| 99460 | Initial hospital care for newborn |
| 99464 | Attendance at delivery |
Common Causes of Claim Denials in ICD-10 Obstetric & Perinatal
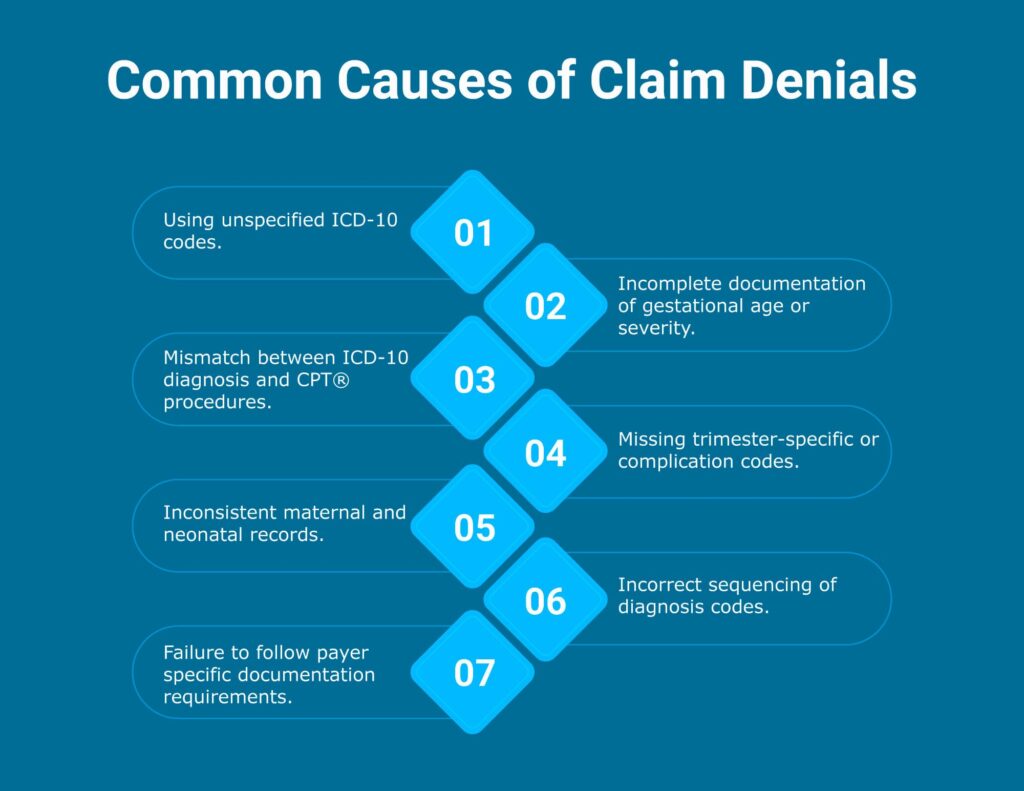
Frequent denial triggers include:
- Utilization of unspecified ICD-10-CM codes despite availability of more specific trimester- or condition-based codes.
- Incomplete clinical documentation of gestational age, severity, onset, or maternal/fetal outcomes.
- Discrepancy between ICD-10-CM diagnosis codes and CPT® procedure codes, leading to validation failures.
- Omission of trimester-specific or complication-related codes required for accurate reporting.
- Inconsistencies between maternal and neonatal records, resulting in claim rejection or payer queries.
- Improper sequencing of diagnosis codes, failing to assign obstetric conditions as the primary diagnosis when appropriate.
- Non-adherence to payer-specific documentation and coding requirements, impacting medical necessity validation and reimbursement.
How to Avoid Denials in ICD-10 Obstetric & Perinatal 2026 Codes?
Documentation Checklist
Provider documentation should include:
Comprehensive, detailed documentation is essential for accurate ICD-10-CM code assignment and payer compliance. Clear, structured records not only justify the reported codes but also support medical necessity and reduce claim denials. The following elements are critical for obstetric and perinatal encounters:
- Gestational age and trimester: Specify the exact gestational week and clearly document the trimester at the time of the visit or procedure to ensure correct selection of pregnancy-related diagnosis codes.
- Maternal complications (HTN, diabetes, infections): Record all relevant maternal conditions such as chronic or gestational hypertension, gestational diabetes, or infections, as these impact risk adjustment and affect code specificity.
- Delivery type (vaginal, C-section, VBAC): Clearly document the delivery method and any related procedures, as this directly drives the selection of both ICD-10-CM and CPT® codes for labor and delivery services.
- Neonatal outcomes (Apgar scores, prematurity, birth weight): Include immediate newborn assessments such as Apgar scores, gestational age at birth, prematurity status, and birth weight to ensure accurate perinatal condition coding.
- Relevant labs, imaging, and therapy details: Capture all pertinent test results, ultrasound findings, and therapeutic interventions that support the clinical decision-making process and validate the coded diagnoses and procedures.
Partner with Pro-MBS for Smarter, Compliance-Driven Medical Billing
At Pro-MBS, we deliver end-to-end medical billing and coding solutions designed for the unique challenges of healthcare providers and billing firms.
Our certified specialists work as an extension of your team, ensuring accurate code selection, precise charge capture, and full alignment with payer policies and compliance standards to minimize delays, reduce denials, and keep your cash flow strong.
We go beyond routine claim processing. By combining advanced billing protocols, streamlined workflows, and proactive denial-management strategies, we help you optimize the entire revenue cycle, from charge entry to final payment.
Our consultative approach focuses on documentation integrity, real-time error resolution, and ongoing process improvement, empowering you to achieve higher first-pass acceptance rates, faster reimbursements, and sustainable financial growth, all while allowing your clinical team to stay focused on delivering exceptional patient care.