Annual Wellness Visit Coding begins with a single question. How do you guide a visit that appears simple on the surface yet carries so much weight beneath it? You sit with the patient. You ask about their health. You sense the story, which they bring with them. And you know, even before the note begins, that this visit shapes their future path.
So what choices will you make? What details will protect the claim? What steps will strengthen the plan? These questions give direction. Because Annual Wellness Visit Coding is not just billing. It is strategy - It is structure - It is the quiet framework behind prevention. Let us walk through this process the same way professionals study a trail. Calm, purposeful, and alert.
What is Annual Wellness Visit Coding and Why Does it Matter in 2025?
What makes an Annual Wellness Visit different? Why does Medicare treat it with such precision? According to CMS, the AWV exists to build a personalized prevention plan. It reviews risks. It identifies gaps, and it informs long-term health. And where does Annual Wellness Visit Coding fit within that purpose? At each step because accurate coding protects reimbursement and supports compliance. It makes sure the visit’s intent is understood and correctly recorded.
If the HRA is missing, the claim fails. If the plan is generic, Medicare questions it. If the documentation is incomplete, auditors notice. This is why Annual Wellness Visit Coding matters so much in 2025. It stands at the crossroads of patient care and operational survival.
How Do G0438 and G0439 Differ in Medicare Wellness Visits?
Two codes define the AWV landscape. Both simple, both powerful, and both requiring absolute clarity. G0438 is the Initial AWV. The first chapter. A one-time event that never repeats. G0439 is the Subsequent AWV. The annual follow-up. A chance to update the plan and address new risks.
So what controls the choice between these codes? Timing, history, and eligibility. Medicare allows G0439 only once every 12 months plus one day. That extra day matters. Without it, the claim breaks.
Code G0438 vs G0439
| Code | Visit Type | Core Requirements | Frequency | Notes |
|---|---|---|---|---|
| G0438 | Initial AWV | First time risk and history review | Once per lifetime | Establishes baseline plan |
| G0439 | Subsequent AWV | Updated assessment and prevention plan | Every 12 months plus 1 day | Cannot precede initial AWV |
What Documentation Is Required for G0438 and G0439 in 2025?
Why does Medicare focus so heavily on documentation? Why does each required element matter? Because each part shapes the prevention plan. Each one adds to the risk picture. Each contributes to long term care decisions. According to CMS, every AWV must include: The Health Risk Assessment. Medical and family history. Medication review. Provider and supplier list.
Routine measurements such as height, weight, BMI, and blood pressure. Cognitive assessment. Depression screening, fall risk assessment, functional ability review, and home safety review. A personalized prevention plan. If you miss any part, the AWV becomes incomplete. And incomplete visits do not survive the demands of Annual Wellness Visit Coding.
Which AWV Elements Must Be Documented to Avoid Coding Denials?
Now let us explore each required element with rhythm and clarity. Because each one affects the visit’s fate.
Health Risk Assessment Structure
Why does the HRA matter so much? Because it reflects the patient’s experience. Their habits. Their struggles. Their risks. The patient completes it. You review it. You build the plan from it. CMS expects a clear link between the HRA and the prevention plan.
List of Risk Factors
What risks shape a patient’s future? Activity levels, diet patterns, chronic conditions, family history, vision changes, and balance issues. You list these openly and clearly. They give structure to your counseling and plan. They guide Annual Wellness Visit Coding toward accuracy.
Screening Schedule
What should the next 5 to 10 years look like for this patient? Screenings follow USPSTF and CMS coverage guidance. Diabetes checks. Colonoscopies. Vaccines. Mammograms. Bone density testing. This schedule must reflect the patient’s unique profile. Not a template. Not a copy. A genuine plan.
Advance Care Planning
Patient Counseling
Personalized Wellness Plan
Required AWV Documentation Elements
| Element | Description | Who Completes It |
|---|---|---|
| HRA | Lifestyle and risk review | Patient and provider |
| History | Past medical and family details | Provider |
| Medication review | Updated medication list | Provider |
| Cognitive check | Basic cognitive screen | Provider |
| Depression and fall risk | Standard tools used | Provider |
| Function and safety | ADLs and home safety | Provider |
| Prevention plan | Personalized plan | Provider |
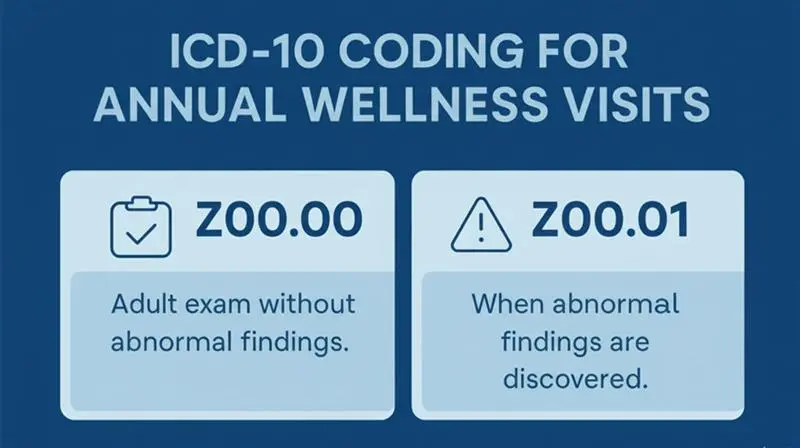
ICD-10 Coding for Annual Wellness Visits
Does Medicare require a specific ICD-10 for AWVs? According to CMS, the answer is no. But two codes guide these visits:
- Z00.00 for general adult exam without abnormal findings.
- Z00.01 when abnormal findings are discovered.
The rule is simple. If you code it, you must show it. If the finding is not documented, do not use Z00.01. Clear ICD selection supports clean Annual Wellness Visit Coding.
What Add-On Services Can Be Billed with G0438 or G0439 AWVs?
What can you add to an AWV? Which services fit the visit without breaking its purpose? Medicare allows several add-ons, each with its own rules, each with its own weight.
- G0444 for depression screening: This code supports a structured, evidence-based tool that looks for early signs of depression. The screen must be documented with care and tied to the risks the patient carries.
- G0442 for alcohol misuse: This service uses a brief, validated assessment to uncover harmful drinking patterns. You must record the tool used, the findings, and the discussion that follows.
- G0446 for cardiovascular counseling: This code applies when you guide the patient through behavior changes linked to heart health. Diet. Activity. Daily habits. The advice must reflect the patient’s real risks.
- G0447 for obesity counseling: Use this when the patient’s BMI reaches 30 or higher. The conversation should stay focused on weight-related risks and small, realistic steps toward change.
- 99497 and 99498 for advance care planning: These codes belong to moments when patients choose to discuss future decisions. You document the time. You document the topics. Directives. Proxies. Wishes for the road ahead.
Each add-on stands on its own. Each demands its own note. Each must connect directly to the risks uncovered in the visit. Handled with care, these services strengthen your work and support clean Annual Wellness Visit Coding.
Add-On Services Allowed with AWVs
The fight inside Internal Medicine RCM Challenges is not won with paper or patience. It is won with precision. With tools that do not blink and do not tire. Each one built for purpose. Each one exact in its strike. They move together. Silent. Certain. One cleans. One tracks. One predicts. In their rhythm, billing changes. It becomes steady. Sharp. Alive.