A behavioral health clinic in North Las Vegas providing Applied Behavior Analysis (ABA) services was facing a confusing and familiar challenge. Their billing team was overwhelmed. Their claims were getting denied, payments were delayed, and manual follow-ups were taking important and valuable time that could have been spent serving patients. The owners knew they needed expert help to bring order, structure, visibility, and consistency back into their revenue and manage this whole cycle. That’s when they reached out to Pro-MBS. Within six weeks, their clean claim rate jumped to 97%, denials fell to 11.05%, average payment turnaround dropped from 55 days to just 25, and monthly revenue grew by 36%.
Here is how we made that happen.
About the Client
The client is a small ABA therapy practice based in North Las Vegas, Nevada, serving around 20-25 families every month. Their sole mission is to provide behavioral therapy that helps children achieve meaningful and developmental milestones. They used Central Reach (CR) for billing and Office Ally as their clearinghouse. With only a few staff members handling multiple payers and complex rules, billing accuracy often took a back seat and malfunctioning began to happen. The result was the only constant struggle to keep revenue stable and operations compliant.
Challenges Faced by the Practice
Before we stepped in, the practice’s Behavioral Health Billing system was more reactive than proactive. The team spent most of their time fixing problems after denials came back instead of preventing them from happening in the first place.
Here’s what we uncovered during our initial assessment:
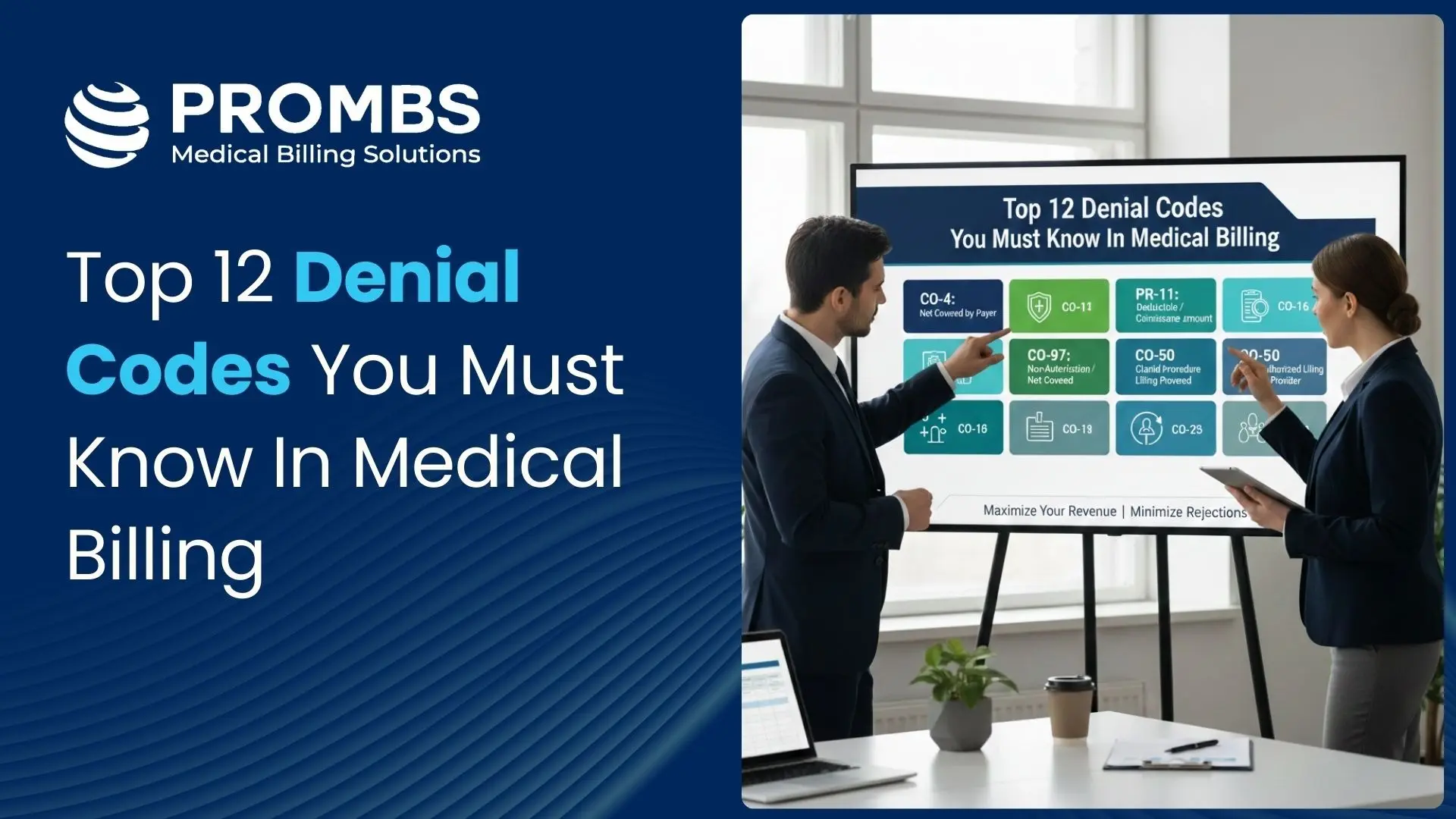
- Low clean claim rate (85.01%) and high denial rate (20.52%), creating long payment delays, sometimes up to 55 days.
- Authorization gaps, with some requests missing or expired before sessions took place.
- Incorrect or missing modifiers such as UD, HM, HO, and 76, causing automatic rejections.
- CPT/ICD-10 mismatches that triggered medical necessity denials.
- Missed payer deadlines due to manual claim tracking.
- Outdated insurance data and missing treatment plans that slowed approvals.
- No denial tracking system, so recurring issues went unnoticed.
- Manual follow-ups and payment posting consuming staff time.
- Denied claims not being reworked promptly, leading to unnecessary write-offs.
The team was doing its best, but without proper analytics or automation, there was no clear picture of where money was being lost.
How Pro-MBS Addressed the Challenges
We came in with one clear goal: to rebuild thei billing workflow into something lean, accurate, and fully compliant. Our strategy was structured but flexible enough to adapt to the practice’s real-world challenges.
We followed a five-step improvement plan, each designed to deliver visible results within weeks rather than months.
1. Comprehensive Workflow and Compliance Audit
2. Strengthening Front-End Accuracy
We tackled errors at the source before claims were even created.
By introducing real-time eligibility and benefits verification, every patient’s coverage was confirmed before the visit. We also set up a centralized authorization tracker with automatic alerts for expiring or pending approvals. This alone prevented dozens of denials that previously came from authorization lapses or outdated coverage.
3. Pre-Billing Validation and Denial Prevention
4. AR Optimization and Payment Automation
5. Performance Monitoring and Staff Empowerment
The Results
In just six weeks, the practice began to see measurable amount of improvements across every metric that mattered the most.
| KPI | Before | After (6 Weeks) |
|---|---|---|
| Clean Claim Rate | 85.01% | 97% |
| Denial Rate | 20.52% | 11.05% |
| Avg. Reimbursement Time | 55 Days | 25 Days |
| Staff Hours Saved | — | 30 Hours/Month |
| Revenue Growth | — | +36% |
Their billing team now operates with confidence, backed by clear data and automated systems. Claims go out clean, payments come in faster, and the clinic finally has the Soothing breath room to focus on what they do best and that is patient care.
Looking Ahead
The improvements we brought for them were not short-term. By integrating automation, training, and consistent reporting, the practice built a foundation for long-term stability. Today, their billing operations run with super clarity, accountability, and measurable control. Instead of chasing denials, the team now focuses only on maintaining compliance and growing their practice.
Visit our website to schedule your free RCM audit and discover how Pro-MBS can help you reduce denials, improve compliance, and accelerate cash flow.
Ready to strengthen your revenue cycle? Schedule your free RCM audit with Pro-MBS and discover how a structured, data-driven billing process can reduce denials, improve compliance, and accelerate your revenue growth.