CMS Credentialing Requirements for Providers: Start Right, Get Paid Faster
As of March 2025, according to the Centers for Medicare and Medicaid Services (CMS), approximately 68.6 million individuals are enrolled in Medicare, with 90.1% of those enrollees being over the age of 65. The growing enrollment underscores the importance of ensuring timely CMS credentialing for healthcare providers. Additionally, the nonprofit KFF (Kaiser Family Foundation) notes that in 2024, 32.8 million people enrolled in Medicare Advantage (Part C) plans, accounting for around 54% of the eligible Medicare population. This increasing enrollment highlights the critical need for healthcare providers to comply with CMS credentialing requirements to receive timely reimbursements and avoid claim denials. Failure to meet these requirements could result in delayed payments or loss of Medicare billing privileges. However, with the right steps, credentialing can be a manageable process, setting the foundation for smooth claims processing. In this guide, you’ll learn how to navigate the CMS credentialing process, from submitting the correct forms to staying compliant with federal and state regulations, ensuring your practice gets paid faster and more accurately.
In this guide, you’ll learn:
- What CMS credentialing is and why it’s required
- How to enroll through PECOS and choose the right CMS-855 form
- Credentialing checklists for individual and group providers
- Revalidation timelines and how to avoid deactivation
- The most common credentialing mistakes and how to avoid them
Whether you're a new provider joining Medicare or updating an existing enrollment, this step-by-step breakdown will help you stay compliant, avoid denials, and get reimbursed faster.
What Is CMS Credentialing?
Imagine trying to serve Medicare patients only to find out you’re not authorized to bill for the services you’ve already provided. That’s what happens when CMS credentialing is skipped or mishandled.
CMS credentialing, officially known as Medicare provider enrollment is the formal process of verifying that you (or your organization) are qualified and authorized to deliver services to Medicare beneficiaries and get paid for them. This process ensures that all providers meet federal compliance standards, have the appropriate licensure, and are free of disciplinary or legal restrictions.
Credentialing isn’t just for doctors. It applies to:
- Physicians (MD, DO)
- Nurse Practitioners (NP)
- Physician Assistants (PA)
- Physical/Occupational Therapists
- Group practices
- Clinics, labs, DMEPOS suppliers, and other institutional providers
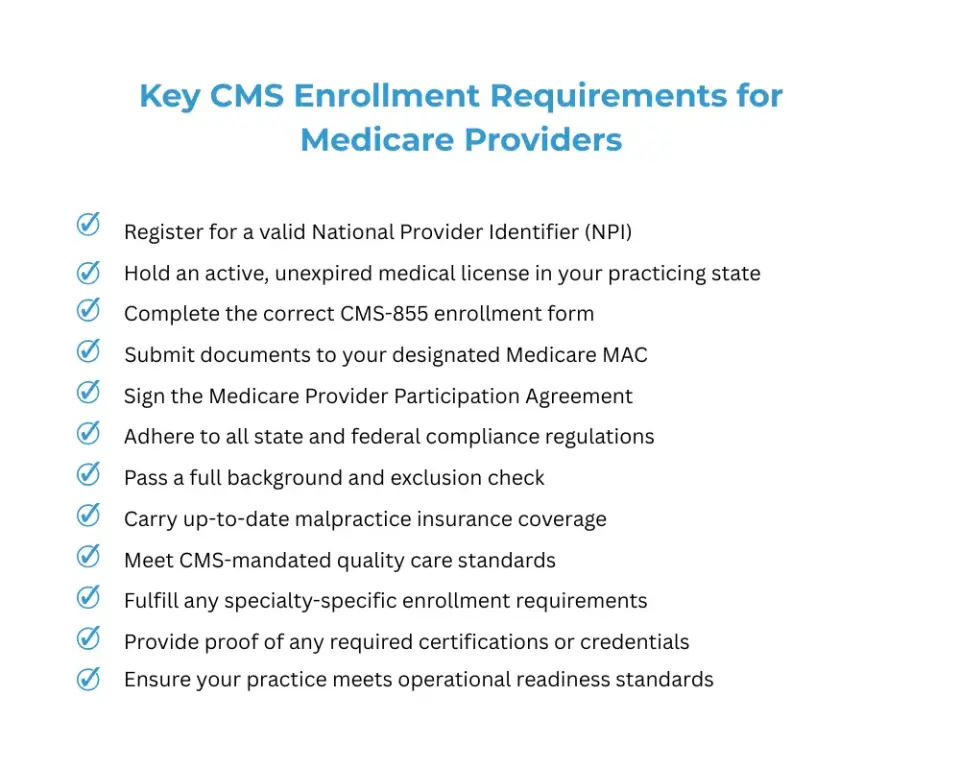
To complete CMS credentialing, you'll need to validate several key aspects of your practice, including:
| Requirement | Purpose |
|---|---|
| State Licensure | Must be active and unrestricted for credentialing and billing |
| Medical Education & Board Certification | Verifies your clinical qualifications and training background |
| NPI (National Provider Identifier) | Required for billing and electronic healthcare transactions |
| Malpractice Insurance | Confirms you have liability coverage in case of legal claims |
| NPDB Report | Screens for malpractice claims or disciplinary actions |
| Ownership Structure | Discloses business ownership (required for groups or entities) |
Step-by-Step CMS Credentialing Process
Credentialing is not just a matter of filling out a form, it’s a structured compliance process that validates your qualifications, protects your revenue, and confirms your eligibility to participate in the Medicare program. If done correctly, it prevents delays in payment, denials, and even loss of billing privileges. This section breaks down each step so you understand what to do, why it matters, and how to complete it successfully even if you’ve never done it before.
Let’s walk through the credentialing process in full detail so that even if you’re starting from scratch, you’ll understand exactly what to do:
Step 1: Create or Verify Your NPI
What is an NPI and Why Is It Important?
The National Provider Identifier (NPI) is a unique 10-digit number issued by CMS to healthcare providers and organizations across the United States. It serves as your digital identity for all administrative, billing, and HIPAA-compliant transactions with Medicare, Medicaid, and commercial payers.
Without a valid NPI, you legally cannot bill Medicare or participate in any part of the CMS credentialing process. It acts as the anchor that connects your licensure, taxonomy (specialty classification), practice location, and Medicare enrollment data.
Why This Step Matters:
How to Complete This Step:
- Visit the official NPPES website to apply for a new NPI or verify your existing one.
- Carefully check that your:
- Legal name and degree/title
- Practice location address
- Taxonomy code (e.g., Family Medicine, Internal Medicine, DME Supplier)
- Contact information are all current and accurate.
- If anything is outdated or incorrect, update it in NPPES immediately.
- Save a copy of the confirmation for your credentialing file this will be needed later in your CMS application.
Taking time to get your NPI right before moving forward prevents costly delays and positions you for a smoother enrollment experience.
Step 2: Gather Required Documentation
What Is This Step and Why It Matters
Before you begin your CMS application, you must have all required documents organized and ready. These documents serve as proof of your professional qualifications, licensure, and legal right to operate. Incomplete or missing paperwork is the #1 cause of application delays and rejections.
This step ensures that once you begin the CMS-855 or PECOS application, you won’t need to pause and track down critical forms, licenses, or signatures. Preparing ahead saves you time, reduces errors, and increases the chances of first-time approval.
How to Complete This Step:
| Requirement | Details | Action Tip |
|---|---|---|
| State License(s) | Must be active, unrestricted, and free from any disciplinary actions or investigations | Verify license status with your state board and renew if needed |
| Board Certifications & Education | Includes medical school diplomas, residency certificates, and board certifications | Keep all credentials in one labeled digital folder |
| Malpractice Insurance Certificate | Proof of current coverage that meets payer and CMS minimum liability requirements | Request the most recent COI (certificate of insurance) |
| NPDB Report | Your National Practitioner Data Bank self-query showing malpractice history or disciplinary records | Order at HRSA Gov |
| Ownership Disclosures | Required for anyone with 5% or more ownership, including name, role, and percentage owned | Prepare a disclosure document per CMS-855 requirements |
| Accreditation Certificates | Applies to DMEPOS suppliers, ASCs, labs, and certain facilities as required by CMS | Check if accreditation (e.g., from ACHC, The Joint Commission) applies to your entity |
| File Format | All documents should be scanned and saved in PDF format for digital upload and storage | Organize a credentialing folder for easy access and upload |
Step 3: Choose the Right CMS-855 Form
What Is This Step and Why It Matters
CMS requires different versions of its Form 855 depending on your provider type and how you intend to bill? Choosing the wrong form can derail your entire application or delay enrollment by weeks.
Each CMS-855 form type corresponds with a specific role (individual, group, supplier), so it’s important to know where you fit in before proceeding with the application.
How to Complete This Step:
CMS has different versions of the 855 forms, depending on your provider type:
| Form | Description |
|---|---|
| CMS855I |
For individual practitioners (MDs, NPs, PAs, therapists). Use for new enrollments, revalidations, updates, and reassignment of benefits.
As of September 2023, reassignment is handled within this form—CMS855R is no longer submitted separately. |
| CMS855B |
For group practices or organizations enrolling with Medicare. Used to enroll, revalidate, or update group information.
Note: Individual members must also submit CMS855I. |
| CMS855R | Deprecated. As of late 2023, this form is no longer submitted independently. All reassignment actions must be done through CMS855I. |
| CMS855S | For DMEPOS suppliers (Durable Medical Equipment, Prosthetics, Orthotics, and Supplies). Use this to enroll or update supplier information. |
Make sure you’re using the most current version of the form from the CMS website.
Step 4: Submit Your Application via PECOS (Preferred Method)
What Is This Step and Why It Matters
Submitting your application is the official step where you enroll with Medicare. PECOS (Provider Enrollment, Chain, and Ownership System) is CMS’s secure web-based platform that simplifies and speeds up enrollment.
Submitting through PECOS instead of paper CMS-855 forms improves accuracy, allows document uploads, and enables real-time status tracking. It’s also the most direct way to communicate with CMS and your Medicare Administrative Contractor (MAC).
How to Complete This Step:
- Log into the PECOS portal using your I&A (Identity & Access) credentials.
- Step through the application interface carefully. Double-check each section for accuracy.
- Upload supporting documents (scanned licenses, NPI info, insurance, etc.).
- Review the completed application before submission. Submit electronically and print the submission confirmation for your records.
Why use PECOS? Applications submitted electronically through PECOS are processed faster and have fewer rejection rates compared to paper submissions.
Step 5: Respond to Additional Requests or Corrections
What Is This Step and Why It Matters
How to Complete This Step:
After submission, your Medicare Administrative Contractor (MAC) may contact you:
- They may request clarification on documents, signatures, or inconsistencies.
- Always respond quickly CMS often sets a strict deadline (e.g., 15–30 days) to respond or the application is dismissed.
- If corrections are needed, log back into PECOS, make the updates, and resubmit the necessary parts.
Step 6: Complete Site Visit or Accreditation (If required)
What Is This Step and Why It Matters
How to Complete This Step:
Certain providers, especially facilities or DME suppliers, must:
- Undergo a site visit by a CMS contractor (e.g., National Site Visit Contractor).
- Maintain a clean, compliant, operational office space.
- Be prepared with signage, hours of operation, staff presence, and required documentation on-site.
- Alternatively, some providers may submit proof of accreditation from CMS-approved agencies like The Joint Commission or ACHC.
Site visit failures are a leading cause of CMS credentialing denial for suppliers and facilities.
Step 7: Track Your Status and Maintain Records
What Is This Step and Why It Matters
How to Complete This Step:
- Log into PECOS regularly to track your application progress.
- Once approved, print and save your approval letter.
- Maintain all credentialing documents (digital and physical) for at least 10 years.
- Add reminders to track revalidation cycles (typically every 3 or 5 years depending on provider type).
Credentialing Timelines and Common Delays
- Use PECOS over paper forms to avoid unnecessary mailing delays.
- Double-check your NPI and credentials to avoid mismatches.
- Resolve any NPDB red flags early, before CMS reviewers see them.
- Assign a credentialing point person or use a checklist to ensure all forms and attachments are ready.
- Track your submission and respond promptly to CMS communications to avoid auto-denials.
Let's Get You Credentialed Fast and Right with Pro-MBS
Waiting too long to credential (or revalidate) can put your revenue and reputation at risk. Whether you're adding new providers, opening a second location, or simply trying to stay ahead of CMS deadlines, the right support makes all the difference.
Book your free credentialing consultation with Pro-MBS today. Our experts will assess your current status, flag any risks, and help you complete the CMS credentialing process with zero guesswork. Let us help you avoid delays and denials. Get credentialed correctly right from the start.