If your organization is seeing a rise in CO-11 denials, you’re not alone. According to HFMA, CO-11 denials account for nearly 20% of all medical-necessity rejections and cost providers an average of $25–$118 per claim in rework. This denial, defined as “Diagnosis inconsistent with procedure,” is one of the most common and costly in healthcare billing. It indicates that the diagnosis submitted on a claim does not support the billed CPT code based on payer medical-necessity criteria.
While many teams treat CO-11s as coding errors, they are actually signs of a larger issue: misalignment between clinical documentation, coding logic, and payer policy. These mismatches disrupt cash flow, delay payments, and can create compliance exposure if left unresolved.
This article explores the most frequent CO-11 denial scenarios, the role of coverage policies, the value of medical-necessity libraries, and the steps to build an effective prevention and appeal process. As per the AAPC article “Comply with CMS’ Guidance on Accurate and Supportive Documentation,” accurate documentation is critical to ensure ethical billing practices and to maintain the integrity of patient records.
Common CO-11 Denial Scenarios and How to Prevent Them
The key to preventing CO-11 denials is understanding where mismatches originate. Most stem from gaps in coverage interpretation, outdated mappings, or incomplete provider documentation. According to Revco Solutions’ guide “13 Common Denial Codes and How to Prevent Them,” CO-11 is consistently among the top denial drivers due to poor CPT-to-diagnosis alignment and incomplete documentation.
| Scenario | Description | Recommended Prevention Strategy |
|---|---|---|
| Incorrect ICD linkage | The diagnosis submitted does not meet payer criteria for the CPT billed. | Maintain payer-specific ICD-to-CPT crosswalks verified against CMS LCDs, NCDs, and commercial payer policies. |
| Auto-populated EHR codes | Default codes applied by templates fail medical-necessity validation. | Audit EHR auto-coding logic quarterly and verify payer-specific mappings. |
| Coverage policy mismatch | The CPT is used for conditions outside the payer’s covered indications. | Reference the latest payer medical-policy bulletins before billing. |
| Incomplete clinical documentation | Insufficient detail in provider notes to justify the CPT. | Reinforce documentation training and emphasize problem-list accuracy. |
| Multiple CPT line errors | Only one CPT is supported by the diagnosis, but multiple were billed. | Use line-level front-end edits to validate every CPT-Dx pair individually. |
According to the Change Healthcare 2022 Revenue Cycle Denials Index, nearly half of all denials originate from front-end revenue cycle issues, including registration, eligibility, missing/invalid claim data, and authorization errors.
Did You Know?
CO-11 denials are among the most expensive and preventable issues in medical billing. According to HFMA, they account for nearly one in five medical-necessity denials and cost providers an average of $25 to $118 per claim in administrative rework. AAPC reports that over 40 percent of these denials result from inaccurate CPT-to-diagnosis mapping or outdated EHR setups, while CMS attributes about 30 percent to documentation gaps. Minor misalignments between coding, documentation, and payer policy directly increase denial frequency, elevate compliance risk, and contribute to measurable revenue leakage.
Coverage Policies and Medical Necessity Rules
Every CO-11 denial connects to a coverage policy that defines medical necessity. Payers rely on these policies to decide which diagnoses justify specific procedures. Understanding and applying them correctly is central to denial prevention.
| Policy Type | Governing Body | Operational Impact |
|---|---|---|
| National Coverage Determination (NCD) | Centers for Medicare & Medicaid Services (CMS) | Establishes national coverage for Medicare providers. |
| Local Coverage Determination (LCD) | Medicare Administrative Contractors (MACs) | Defines regional coverage criteria for certain services and diagnoses. |
| Commercial Payer Policy | Private health plans and managed care organizations | Determines CPT-Dx pairings, prior authorization needs, and frequency limits. |
| Internal Medical Policy Bulletin | Payer medical review boards | Details payer-specific indications that may be stricter than CMS standards. |
For example, CMS LCD L34833 defines medical necessity for cardiac rhythm device evaluations, while LCD L37757 outlines coverage for musculoskeletal services. These documents specify which diagnosis codes support each CPT, and when a procedure is not covered.
Keeping your organization aligned with these evolving policies is the foundation for cleaner claims and compliant reimbursement.
Building a Medical-Necessity Library That Prevents CO-11 Denials
1. Automating CPT-Dx Crosswalks with Policy-Based Rules
2. Maintaining Version Control for Audit-Ready Compliance
3. Aligning Clinical Documentation with Payer Coverage Criteria
4. Role-Based Access to Medical-Necessity Libraries for Coders and CDI Teams
Assign access to coders, compliance officers, and CDI specialists to update or review mappings. Shared ownership ensures accuracy across all teams.
A strong medical-necessity library doesn’t just reduce denials; it also reinforces provider education and strengthens audit defensibility.
Front-End Edits and Pre-Claim Validation to Prevent CO-11 Denials
Preventing CO-11 denials starts long before claim submission. Embedding payer-specific edits in front-end workflows enables early detection of CPT-Dx mismatches and prevents downstream denial risk. AHIMA notes that organizations implementing medical-necessity validation before submission can reduce denials by more than 30 percent.
Steps to Build a Pre-Claim Validation Framework:
- Translate payer policies into coded rules that validate CPT-Dx compatibility.
- Integrate those edits directly into charge capture and claim creation.
- Define “hard” edits that block submission and “soft” edits that prompt coder review.
- Route flagged claims to a QA queue for resolution before submission.
- Conduct monthly reviews of recurring front-end edits to identify systemic deficiencies and reinforce coder education.
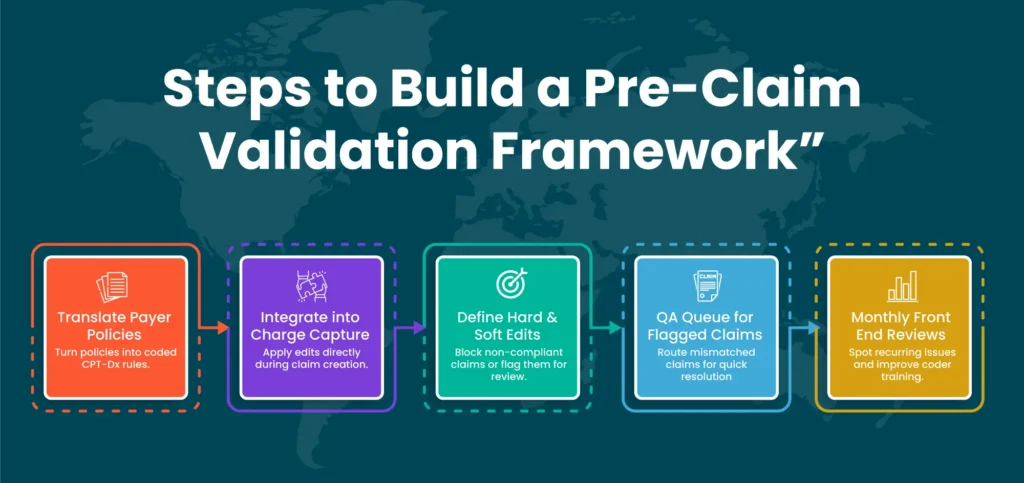
Once implemented, pre-claim validation frameworks have been shown to reduce manual rework by more than 30%, according to AHIMA case studies. This improvement results from early detection of CPT-Dx mismatches, which decreases downstream denial volume and accelerates clean-claim submission.
Using Analytics to Predict and Prevent CO-11 Denials
Analytics provide visibility into why denials happen and where to focus improvement efforts. Instead of reacting to denials, RCM leaders can predict and prevent them.
Key Performance Indicators (KPIs):
• CO-11 Denial Rate: Measures the overall frequency of claims denied due to diagnosis-procedure (CPT-Dx) mismatches. A rising CO-11 denial rate highlights gaps in denial analytics, payer compliance, and medical-necessity validation, often linked to documentation errors or weak front-end edits in the revenue cycle.
• Top CPT/Dx Pairs: Identifies the most common CPT-to-diagnosis pairings that trigger CO-11 denials. Tracking these trends enables targeted denial prevention strategies, provider education, and updates to crosswalks to ensure alignment with payer coverage policies and medical-necessity rules.
• Appeal Success Rate: Reflects the percentage of denied claims successfully overturned through appeals. Low success rates typically point to inadequate medical-necessity documentation, weak alignment with payer policy guidelines, or poorly structured appeal packets. These are critical factors in denial recovery performance.
• Average Rework Days: Calculates the time required to correct and resubmit claims denied for CO-11 reasons. Monitoring this KPI highlights inefficiencies in denial resolution workflows. Extended rework cycles increase days in accounts receivable and indicate the need for enhanced front-end validation and policy-aligned denial prevention controls.
• Repeat Denial Frequency: Tracks how often the same claim types experience CO-11 denials repeatedly. High recurrence indicates systemic weaknesses such as outdated CPT-Dx crosswalks, insufficient staff training, or gaps in payer policy compliance. These issues require process-level intervention rather than one-off claim fixes.
Research from Advisory Board shows that organizations monitoring denial metrics weekly, rather than monthly, resolve errors 25 percent faster and see steady decreases in repeat CO-11 activity. Analytics-driven prevention also identifies which payer rules or specialties create the highest mismatch volume, enabling targeted interventions.
Writing CO-11 Denial Appeal Letters That Win Reimbursements
Even with strong controls, some denials will occur. The appeal process serves as a formal mechanism to validate compliance with payer-defined medical-necessity criteria and to substantiate coverage through documented evidence.
| Appeal Element | Example Wording | Purpose |
|---|---|---|
| Medical Necessity Statement | “CPT 29880 was performed for a medial meniscus tear, supported by ICD-10 M23.21 and documented MRI findings.” | Establishes a clear medical-necessity link. |
| Supporting Documentation | Include operative notes, clinical records, and imaging results. | Provides factual evidence of necessity. |
| Policy Citation | “Per CMS LCD L34833, CPT 29880 is covered when performed for diagnosis M23.21.” | Demonstrates alignment with payer rules. |
| Provider Attestation | “I attest that the service performed was medically necessary for the patient’s documented condition.” | Adds professional validation and accountability. |
According to AAPC, Appeals that incorporate payer-specific policy citations and comprehensive clinical documentation demonstrate higher compliance integrity and achieve superior overturn rates.
Collaborative Roles in CO-11 Denial Prevention
Preventing CO-11 denials is not a single-department task. It takes coordinated effort among coding, documentation, billing, and analytics teams to maintain medical-necessity compliance and ensure accurate claim submission. Each group has a distinct role in reducing mismatches and strengthening compliance governance.
Coding and Compliance: The Foundation of Accurate Claims
The coding and compliance team is responsible for maintaining current CPT-to-ICD crosswalks and keeping up with evolving payer coverage policies. Their oversight ensures every claim aligns with the latest CMS, LCD, NCD, and commercial payer requirements. By managing coding audits and policy updates, they help create defensible claims that withstand payer scrutiny.
Clinical Documentation Improvement: Capturing Medical Necessity at the Source
CDI specialists bridge the gap between clinical language and coding rules. Their focus is on educating providers to document specific findings, diagnoses, and medical necessity clearly in the health record. Effective CDI programs transform vague clinical notes into documentation that fully supports CPT selection, preventing CO-11 denials before coding even begins.
Preventing CO-11 denials is not a single-department task. It takes coordinated effort among coding, documentation, billing, and analytics teams to maintain medical-necessity compliance and ensure accurate claim submission. Each group has a distinct role in reducing mismatches and strengthening compliance governance.
Billing Operations: The Gatekeepers of Clean Claims
Revenue Integrity and Analytics: Turning Data into Prevention
The revenue integrity and analytics team provides the intelligence that drives continuous improvement. By monitoring CO-11 denial trends, they can pinpoint root causes, evaluate the effectiveness of front-end edits, and measure financial impact. Their insights turn data into action, guiding targeted training and policy updates that reduce denials long term.
HFMA data indicates that organizations with multi-department denial committees reduce recurring CO-11 denials by as much as 40 percent and achieve faster appeal resolutions.
How Technology and AI Help Eliminate Denials
Revenue Integrity and Analytics: Turning Data into Prevention
Automation allows teams to scale compliance and maintain consistency across large claim volumes.
| Technology | Function | Result |
|---|---|---|
| AI-Based Coding Validator | Flags potential CPT-Dx mismatches before submission. | Prevents errors and saves audit time. |
| Policy Ingestion Engine | Imports LCD, NCD, and commercial payer updates automatically. | Keeps validation rules current. |
| NLP Documentation Scanner | Reviews provider notes for missing or conflicting indications. | Improves documentation completeness. |
| Denial Analytics Dashboard | Visualizes CO-11 trends by payer, specialty, and facility. | Enables targeted improvement strategies. |
According to MGMA, practices using AI-driven validation tools recover up to 15 percent more revenue from denials within the first quarter of deployment.
How Pro-MBS Helps Resolve and Prevent CO-11 Denials?
We partner with healthcare organizations to transition denial management from a reactive, case-based workflow to a data-driven, policy-aligned compliance framework. CO-11 denials often reveal deeper systemic gaps in policy alignment, documentation accuracy, and front-end validation. Pro-MBS addresses these challenges by combining regulatory expertise with intelligent automation to help clients achieve measurable denial reduction and stronger revenue integrity.
Our key capabilities include:
Policy-driven denial governance that aligns with OIG and MGMA recommendations, ensuring cross-department accountability and standardized compliance.
- Automated medical-necessity validation using real-time payer policy data, including LCD and NCD coverage updates.
- Denial analytics dashboards that convert raw claim data into actionable insights for faster root-cause identification.
- Clinical documentation and coding alignment through targeted audits, provider education, and CPT-Dx mapping reviews.
- Predictive denial prevention technology powered by AI and machine-learning models to flag high-risk claims before submission.
By integrating these solutions, Pro-MBS enables revenue cycle teams to prevent CO-11 denials at the source, recover lost revenue efficiently, and maintain long-term compliance confidence. With our policy-based approach and advanced analytics, your organization can turn denial management into a proactive, sustainable part of operational excellence.
Schedule your CO-11 Denial Audit today and discover how accurate CPT-Dx alignment can improve compliance, accelerate reimbursement, and reduce denial rework while helping clients reduce repeat CO-11 denials by up to 30% and improve clean-claim acceptance rates.
FAQs
What is denial code CO-11?
Denial code CO-11 means the diagnosis code reported on a claim is inconsistent with the procedure or service billed, so the payer considers it not medically necessary under their coverage policies. This often occurs when the ICD-10 code chosen does not justify why the CPT/HCPCS procedure was performed, such as a mismatch between the documented condition and the service, use of a nonspecific diagnosis, outdated payer guidelines, or front-end configuration gaps. Correcting it typically involves verifying payer medical-necessity policies, updating the diagnosis or documentation to support the service, and resubmitting or appealing the claim.
How do you prevent CO-11 claim denials?
To reduce claim denials like CO-11, focus on strong front-end validation: verify patient eligibility, check CPT-ICD-10 compatibility against payer medical-necessity policies, and ensure proper documentation before submission. Keep payer guidelines updated, use automated edits in your EHR or clearinghouse to flag mismatches, and analyze denial trends to fix recurring issues. Consistent provider education and timely appeals help maintain a high clean-claim rate and minimize CO-11 denials.
Can a CO-11 denial be appealed, and how?
Yes, a CO-11 denial can be appealed if the service was medically necessary and properly documented. To do this, review the payer’s medical necessity policy and confirm that the documentation supports the procedure for the reported diagnosis. If the diagnosis code was incorrect, correct it and resubmit the claim. If the original code was appropriate, submit a formal appeal letter with the claim, including the provider’s medical notes, test results, and any supporting payer guidelines or LCD/NCD references that justify the service. Timely filing is crucial because appeals must be submitted within the payer’s appeal window, usually 30 to 90 days.
Why do payers issue a CO-11 denial?
Payers issue a CO-11 denial when the diagnosis code on a claim does not support the medical necessity of the procedure or service billed. This often happens due to mismatches between the CPT and ICD-10 codes, use of nonspecific or outdated diagnosis codes, failure to follow payer medical necessity guidelines, or gaps in provider documentation. Essentially, the payer’s system flags that the reported diagnosis does not justify why the billed service was performed.
What does denial code CO-11 mean in medical billing?
Denial code CO-11 in medical billing means that the diagnosis code submitted on the claim does not support the medical necessity for the billed procedure or service. This occurs when there is a mismatch between the ICD-10 diagnosis and the CPT or HCPCS procedure code, such as using an unrelated or nonspecific diagnosis, not following payer medical necessity policies, or having insufficient documentation. As a result, the payer rejects the claim until the issue is corrected or properly appealed.
Does CO-11 denial mean the claim is not covered at all?
No, a CO-11 denial does not mean the claim is permanently not covered. It indicates that the payer believes the diagnosis provided does not justify the medical necessity for the billed service. In most cases, the claim can be corrected and resubmitted by updating the diagnosis code to one that meets the payer’s medical necessity policy or by submitting an appeal with supporting clinical documentation to prove that the service was appropriate for the reported condition.