In the increasingly complex world of medical billing and coding, denials based on mismatched diagnosis and procedure codes continue to be a persistent challenge. Among the most common denial codes issued by Medicare and private payers is CO 11 – Diagnosis Code Inconsistent with CPT Code.
This denial occurs when the ICD-10 code submitted on the claim does not justify the medical necessity of the reported procedure (CPT or HCPCS code). As a result, claims are either denied outright or returned for correction, leading to delays in reimbursement and increased administrative burden.
This guide takes a deep dive into the CO 11 denial reason, its implications for providers, and a detailed approach for resolving and preventing these denials from a billing expert’s perspective.
What Does “Diagnosis Code Inconsistent with CPT” Actually Mean?
A CO 11 denial indicates that the diagnosis code(s) submitted do not clinically or policy-wise support the CPT/HCPCS code according to the payer’s coverage criteria. This can be determined through:
- Payer-specific coverage policies
- CMS National Coverage Determinations (NCDs)
- Local Coverage Determinations (LCDs)
- National Correct Coding Initiative (NCCI) edits
- Clinical guidelines or medical necessity review algorithms
Real-World Example of CO 11 Denial
| CPT Code | Procedure Description | ICD-10 Code | Diagnosis Description | Outcome |
|---|---|---|---|---|
| 45378 | Colonoscopy, diagnostic | Z12.11 | Encounter for screening for colon cancer | Denied – Diagnosis inconsistent with CPT code |
In this case, CPT 45378 indicates a diagnostic colonoscopy, while Z12.11 is used for screening purposes. This mismatch triggered a denial because a screening diagnosis must be paired with an appropriate screening code (e.g., 45378 with modifier 33 or 45378 + G0121).
Common Scenarios That Trigger CO 11 Denials
Incorrect ICD-10 Code Selection
- An unspecified or incorrect diagnosis code that doesn't reflect the provider’s documentation.
- Example: Using “R10.9 – Unspecified abdominal pain” for a therapeutic colonoscopy.
Preventive vs. Diagnostic Mismatch
- Submitting a preventive CPT with a diagnostic ICD-10 code or vice versa.
- This occurs frequently in wellness visits, Pap smears, or colorectal cancer screenings.
Procedure Not Covered for the Diagnosis
- Some procedures are reimbursed only for specific diagnoses. Payers may deny claims when performed for non-covered conditions.
- Example: Physical therapy billed for general fatigue without a documented musculoskeletal issue.
Mismatched Coding Based on NCCI Edits
- CPT and ICD-10 combinations not aligned with NCCI policy edits or LCD/NCD guidance.
Use of Outdated or Deleted Codes
- Using retired ICD-10 or CPT codes that are no longer recognized by payers.
Step-by-Step: How to Resolve a CO 11 Denial
Step 1: Review the Remittance Advice (RA)
- Look for denial code CO 11 or a related Remark Code (e.g., M76).
- Identify which claim line(s) triggered the issue.
- Compare submitted CPT and ICD-10 code pairs.
Step 2: Consult Authoritative Coding Guidelines
Use these tools to validate the code pair:
- ICD-10-CM Official Guidelines for Coding and Reporting
- CPT 2025 Professional Edition
- NCCI Policy Manual
- CMS LCD/NCD database
- Payer’s published policy manuals or bulletins
Step 3: Validate Medical Necessity
- Review the provider’s documentation.
- Confirm whether the diagnosis clearly supports the procedure performed.
- Check for clinical justification in HPI, assessment, and plan sections.
Step 4: Correct Coding and Resubmit the Claim
- If the diagnosis was incorrect or vague, replace it with a more specific code.
- Apply modifiers if needed:
- Modifier 33 for preventive services
- Modifier 25 for significant, separately identifiable E&M services
- Modifier 59 for distinct procedural services
- Ensure proper linkage between the diagnosis and procedure (especially in multi-line claims).
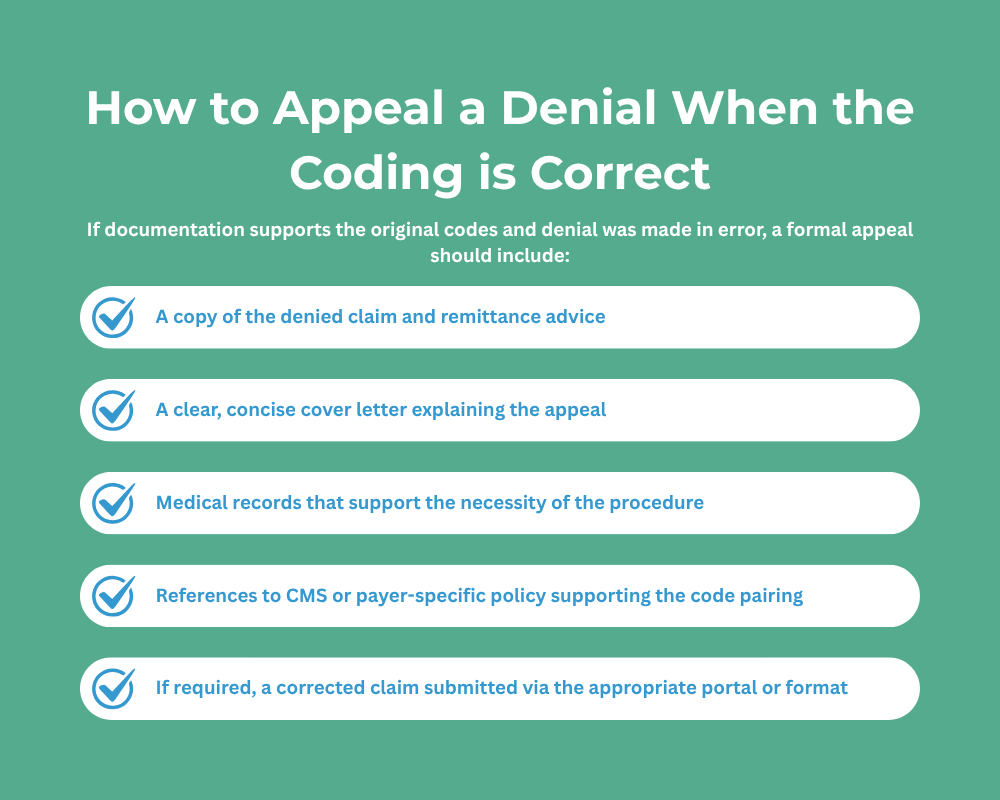
How to Appeal a Denial When the Coding is Correct
| Strategy | Action Items |
|---|---|
| Accurate Documentation | Ensure clinical notes fully justify procedures and indicate necessity clearly. |
| Up-to-date Coding Tools | Use latest ICD-10, CPT, and HCPCS manuals or software like Optum or Find-A-Code. |
| Link Diagnoses Correctly | Make sure diagnosis codes are linked to the correct procedure on each line. |
| Coding Reviews | Conduct periodic internal audits or peer reviews. |
| Modifier Use | Understand and apply modifiers based on NCCI edits and payer requirements. |
| Payer Policies Check | Cross-reference LCDs/NCDs and commercial payer coverage policies before billing. |
| Staff Education | Provide ongoing training for front desk, coders, and billers on evolving policies. |
Common CPT-Diagnosis Code Mismatches to Watch For
| CPT Category | Frequent Coding Issue |
|---|---|
| Colonoscopy/Endoscopy | Using diagnostic code for screening procedure or vice versa. |
| Radiology | Lack of documented signs/symptoms for MRI/CT scans. |
| Dermatology | Skin tag or mole removals billed as medically necessary without justification. |
| Pain Management | Injections billed without corresponding ICD-10 for chronic pain/sciatica. |
| Physical Therapy | Insufficient documentation of functional deficits or qualifying diagnosis. |
Partner with Pro-MBS to Improve Billing Accuracy and Denial Prevention
We help practices eliminate coding inconsistencies and minimize revenue disruption with:
- Pre-bill claim scrubbing and diagnosis validation
- Payer-specific coding intelligence
- Appeals and denial recovery services
- Ongoing staff training and compliance oversight