Cross-Department Billing Teams are what keep a hospital’s financial engine running. In a multi-specialty setup, every department, including cardiology, behavioral health, and radiology, has its own billing rules, codes, and payer requirements. Keeping all those moving parts in sync can be tough.
When billing processes differ from one department to another, small errors start to snowball. Denials rise, cash flow slows, and staff spend more time fixing mistakes than submitting claims. The Healthcare Financial Management Association (HFMA) notes that poor workflow coordination is one of the biggest causes of revenue loss in large healthcare organizations.
Ever wondered why some hospitals manage multi-specialty billing so smoothly while others struggle with constant denials? The good news is that with the right structure and communication, managing Cross-Department Billing Teams becomes much easier. Below are six simple, proven ways to keep your billing operations unified, compliant, and efficient.
Standardize Billing Workflows to Create Consistency
The first step is to make sure every department follows the same billing process, including charge entry, coding, claim submission, and AR follow-up. When each department does things differently, confusion and delays are almost guaranteed. For example, one team might enter charges daily while another waits until the end of the week. Coders may interpret documentation differently, creating inconsistent use of modifiers or diagnosis codes.
Written Standard Operating Procedures (SOPs) solve this problem. They act like a rulebook for billing tasks so everyone follows the same steps. The American Medical Association (AMA) recommends consistent coding and documentation guidelines to reduce claim rejections and administrative waste.
Why it matters?
Standardized workflows reduce costly errors, speed up reimbursements, and make onboarding simpler for new staff. They also create consistency across departments, which helps managers monitor performance and ensures patients are billed accurately every time.
Standardized Billing Workflow Steps
| Step | Description | Goal |
|---|---|---|
| Charge Entry | Enter charges promptly and accurately | Prevent missed revenue |
| Coding | Apply correct CPT/ICD-10 codes | Stay compliant |
| Claim Submission | Send clean claims to payers | Lower denial rates |
| AR Follow-up | Track unpaid claims quickly | Improve collections |
When every department follows the same structured process, billing becomes predictable and reliable. Standardized workflows help teams avoid confusion, reduce rework, and speed up payment cycles. They also make it easier for managers to identify where delays occur and fix them before they impact revenue.
Use a Centralized Billing or RCM System for Better Oversight
What happens when every department uses its own billing tool instead of one shared system? Using separate billing tools for each department is like having different languages in one office. A centralized Revenue Cycle Management (RCM) system fixes that problem. When all teams share a single platform, data becomes consistent and easy to track. Managers can see clean claim rates, denial patterns, and AR days across all departments in one dashboard.
Example: If the cardiology department’s denial rate suddenly increases, leadership can spot the trend right away through the centralized dashboard. With that visibility, they can quickly investigate the root cause, such as coding errors or missing documentation, and fix the issue before it affects other departments or slows down reimbursements.
Why it matters?
Centralized billing aligns with Centers for Medicare & Medicaid Services (CMS) guidance, which emphasizes data transparency and system integration. A single, connected RCM platform helps reduce duplicate claims, speeds up reimbursements, and ensures leadership has a clear, accurate view of financial performance across all departments.
Key Benefits of a Centralized RCM System
| Benefit | Description |
|---|---|
| Unified Dashboard | Track all billing KPIs in one view |
| Consistent Reporting | No more mismatched data |
| Streamlined Operations | Fewer manual processes |
| Better Oversight | Leadership sees real-time performance |
Once connected to automation tools like claim scrubbing or electronic remittance posting, a centralized RCM system can cut manual work dramatically and increase revenue accuracy. It also gives billing leaders better control over the entire payment process, reduces human error, and helps staff focus on higher-value tasks like denial prevention and payer follow-up.
Cross-Train Your Staff to Strengthen Team Flexibility
Billing departments often rely heavily on specialized staff. That’s fine until someone is out sick or the workload suddenly jumps. Cross-training your billing and coding teams is one of the smartest ways to stay flexible. A coder in orthopedics doesn’t need to become an expert in behavioral health, but they should know the basics, such as documentation or authorization rules. This allows staff to fill in gaps when needed without slowing down the billing process.
The American Academy of Professional Coders (AAPC) recommends cross-training as a proven way to build adaptable, well-rounded billing teams. When staff understand multiple specialties, they can step in where needed, balance shifting workloads, and keep the entire revenue cycle running without interruption.
Why it matters?
Cross-training keeps billing operations running smoothly, even when a department is short-staffed or facing higher claim volumes. It strengthens collaboration across teams, reduces burnout, and builds confidence by ensuring everyone understands how their role connects to the larger revenue cycle.
Essential Cross-Training Focus Areas
| Cross-Training Focus | Result |
|---|---|
| Coding for Other Specialties | Smoother teamwork |
| Payer Rule Differences | Fewer denials |
| Denial Management | Faster resolution |
| System Navigation | Easier coverage across teams |
When your staff understands more than one specialty, you build a safety net that keeps operations running smoothly even during staffing changes or high-volume periods. This flexibility protects revenue, maintains productivity, and ensures patients receive uninterrupted billing support across every department.
Improve Communication to Keep Departments Connected
Good communication might seem simple, but it’s often the piece that gets overlooked in hospital billing workflows. When billing leads, coders, and managers don’t stay in regular contact, small errors slip through, and the same mistakes keep repeating. Consistent communication keeps everyone aligned and helps problems get solved before they turn into revenue delays.
Hold short, consistent check-ins, weekly or biweekly works best. Use shared channels like Slack or Microsoft Teams for quick updates. Keep a shared denial log so everyone can see recurring payer issues and how they were fixed. The HFMA points out that regular communication between revenue cycle teams cuts denial turnaround time by up to 30 percent.
Why it matters?
A culture of open communication prevents small issues from turning into bigger revenue problems. It encourages billing teams to share solutions, learn from each other’s experiences, and resolve challenges faster. Over time, this teamwork improves accuracy, reduces stress, and keeps the entire revenue cycle running efficiently.
Recommended Communication Tools for Billing Teams
| Communication Tool | Use |
|---|---|
| Slack or Teams | Quick daily coordination |
| Shared Denial Log | Learn from common issues |
| Monthly Reports | Review progress and KPIs |
Communication doesn’t just improve results, it builds trust and teamwork across departments. When billing teams stay connected and share information openly, it strengthens collaboration, reduces frustration, and creates a culture where everyone works toward the same financial and patient service goals.
Track KPIs by Department to Drive Better Decisions
Data tells the real story behind how well your billing teams perform. Without accurate metrics, decisions are based on assumptions rather than evidence. Tracking billing performance by department helps you see patterns in claim errors, identify workflow bottlenecks, and measure how efficiently each specialty contributes to the overall revenue cycle. It turns guesswork into actionable insight that leads to smarter management and stronger financial results.
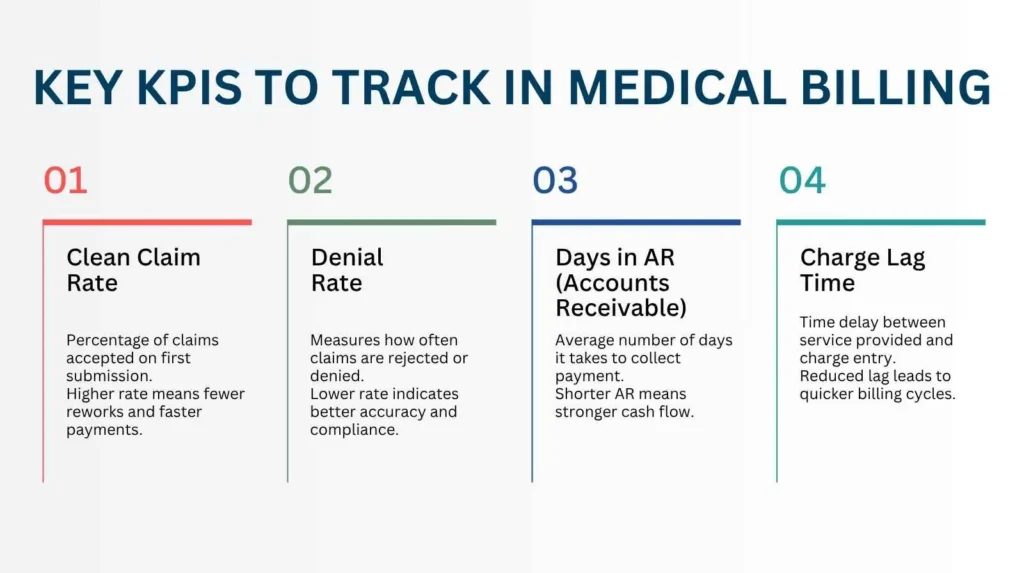
The Medical Group Management Association (MGMA) says consistent KPI monitoring is one of the strongest indicators of long-term financial health in multi-specialty practices.
Why it matters?
Tracking data gives leaders a clear picture of how each department is performing. It highlights which areas need extra support, training, or process improvements, and which teams are meeting or exceeding goals. Consistent performance tracking also helps uncover trends early, so issues can be fixed before they affect reimbursements or compliance.
Core KPIs for Cross-Department Billing Performance
Tracking data gives leaders a clear picture of how each department is performing. It highlights which areas need extra support, training, or process improvements, and which teams are meeting or exceeding goals. Consistent performance tracking also helps uncover trends early, so issues can be fixed before they affect reimbursements or compliance.
| KPI | Target | What It Shows |
|---|---|---|
| Clean Claim Rate | 95% or higher | Accuracy of submissions |
| Denial Rate | Below 5% | Coding and compliance quality |
| Days in AR | Under 40 days | Collection efficiency |
| Charge Lag | 1 to 2 days | Billing turnaround speed |
Sharing KPI dashboards openly creates transparency and accountability across the organization. When every department can see its performance and compare results, it naturally encourages improvement. This visibility turns data into motivation, helping teams take ownership of outcomes and work together toward higher accuracy and faster reimbursements.
Encourage Continuous Improvement to Sustain Growth
Managing Cross-Department Billing Teams isn’t something you set up once and forget. It needs regular attention and fine-tuning. Schedule quarterly performance reviews and workflow audits to catch inefficiencies early, before they grow into bigger revenue or compliance issues.
Ask your billing staff for feedback. They’re the ones who see where bottlenecks happen. Recognize and reward teams who meet or exceed KPI goals. The Centers for Medicare & Medicaid Services (CMS) recommends ongoing internal audits and staff training to maintain compliance and improve reimbursement efficiency.
Why it matters?
Continuous improvement keeps your billing processes evolving instead of stagnating. It helps teams stay sharp, engaged, and proactive about solving problems. Regular updates and feedback loops also strengthen compliance and ensure your revenue cycle keeps pace with payer and regulatory changes.
| Improvement Step | Description |
|---|---|
| Quarterly Review | Identify workflow gaps |
| Process Audit | Verify accuracy and compliance |
| Staff Feedback | Gather real ideas from daily users |
| Recognition | Reward high-performing teams |
When staff know their efforts are valued and recognized, motivation naturally grows. Teams work together more effectively, take pride in what they do, and stay focused on shared goals. This kind of positive culture boosts morale, improves accuracy, and strengthens both team performance and financial results.
It Is Time to Partner with Pro-MBS
Managing Cross-Department Billing Teams takes experience, structure, and the right technology. Pro-MBS partners with hospitals, multi-specialty clinics, and group practices to simplify multi-department medical billing and bring consistency to complex operations. Our experts help standardize hospital billing workflows, unify departmental processes, and implement centralized RCM for multi-specialty practices that improve transparency and reduce denials.
At Pro-MBS, we understand the daily challenges that come with billing across multiple specialties. Our approach focuses on real results such as cleaner claims, faster reimbursements, and stronger team collaboration. Whether your goal is to optimize clinic billing team management or streamline billing across specialties in healthcare, partnering with Pro-MBS gives your organization the structure and insight it needs for long-term financial success.
Frequently Asked Questions
What is a Cross Department?
A Cross Department means multiple hospital teams moving as one. Cardiology. Radiology. Behavioral Health. Each with its own rules, yet bound under one Billing Workflow and RCM System. It is the structure that keeps revenue clean and operations steady. At Pro-MBS, we design these systems so every department speaks the same billing language, flawlessly and fast.
How to Work Effectively with Cross-Functional Teams?
Working with Cross-Department Billing Teams demands structure and rhythm. Set clear workflows. Centralize your RCM System. Keep communication alive. When each team moves in sync, denials fall and claims flow clean. Pro-MBS turns scattered departments into one precise billing engine that never misses a beat.
What are the KPIs for Cross-Functional Teams?
The key KPIs for Cross-Department Billing Teams are Clean Claim Rate, Denial Rate, Days in AR, and Charge Lag Time. These are not just numbers. They are the pulse of your revenue cycle. Track them, refine them, and your cash flow grows stronger. At Pro-MBS, we monitor every metric like a heartbeat to keep your billing system alive and sharp.
What are the Four Cross-Functional Teams?
In healthcare billing, four teams hold the system together. Coding. Charge Entry. Claim Submission. AR Follow-Up. Each one vital. Each one linked. Pro-MBS unites these functions through shared workflows and centralized RCM control, creating precision that never wavers.
What is the Difference Between Cross-Departmental and Cross-Functional?
Cross-Departmental means full departments like Orthopedics or Radiology working together. Cross-Functional focuses on the roles within billing and coders, billers, compliance experts. Different scopes, one goal: clean claims and faster payments. Pro-MBS aligns both worlds into one seamless structure where collaboration drives revenue.
What are the Four Types of Organizational Structure?
Functional. Divisional. Matrix. Flat. In healthcare billing, the Matrix Structure rules best. It balances control with collaboration, allowing teams to share one RCM System across departments. Pro-MBS builds these frameworks so billing stays organized, compliant, and ready for scale.
What is the Difference Between Cross-Departmental and Interdepartmental?
Cross-Departmental is unity with purpose. Departments share workflows, KPIs, and billing goals. Interdepartmental is communication without full integration. Both matter, but only one drives real results. At Pro-MBS, we move your teams beyond coordination into true collaboration that builds predictable revenue.
What is an Example of Cross-Departmental Collaboration?
Picture your billing, coding, and AR teams using one Centralized RCM Platform. They share denial logs, analyze reports, and recover payments together. That is Cross-Department Collaboration in action. At Pro-MBS, we make this a daily reality with systems that unite every department under one pulse.
How to Improve Cross-Departmental Communication?
Keep it simple. Keep it steady. Hold weekly check-ins. Share reports openly. Use tools like Teams or Slack. When departments talk, errors shrink and trust grows. Pro-MBS builds this culture into your billing operations, turning communication into clarity and teamwork into revenue.
Final CTA
Every department. One process. One rhythm. That is how billing becomes strength instead of struggle. Partner with Pro-MBS to build your next-generation Cross-Department Billing Team and transform confusion into control. Get your free billing audit today.