Credentialing healthcare providers is a rigorous process that typically takes three to six months to complete. Every qualification, license, and work history entry must be verified from its primary source before a provider can join a payer’s network.
Because of this lengthy timeline, more healthcare organizations are adopting delegated credentialing, a model that streamlines onboarding, reduces paperwork, and accelerates reimbursement. In this setup, the payer authorizes another qualified entity to handle credentialing tasks on its behalf.
When implemented correctly, delegated credentialing shortens enrollment timelines, speeds payer decisions, and ensures providers can start delivering care and getting paid sooner.
This guide explains everything you need to know: what delegated credentialing is, who can perform it, what data is required, the role of delegated providers, regulatory oversight, requirements, and the pros and cons you must weigh before getting started.
Understanding Delegated Credentialing
Delegated credentialing is a formal arrangement in which one healthcare entity transfers the responsibility for credentialing providers to another entity through a written agreement.
For example, a health plan may authorize a hospital’s credentialing department to verify provider qualifications and make participation decisions for its network. The delegated entity must follow the payer’s approved policies and is subject to regular audits to ensure compliance with industry standards.
Under a delegated arrangement, the authorized organization can verify and review:
- State licensure
- DEA registration
- Board certifications
- Work history and professional experience
- Malpractice coverage and claims history
Sanctions, exclusions, or disciplinary actions
While the delegated entity carries out the work, the delegating payer remains legally responsible for compliance with federal, state, and accreditation standards.
Data Required for Delegated Credentialing
The delegated entity is responsible for collecting and verifying a wide range of provider information. Common data elements include:
- Licensure – Active, unrestricted state licenses with verification from the medical board
- Board Certification – Confirmation from ABMS, AOA, or other recognized boards
- Education & Training – Medical school, residency, fellowship records
- DEA & CDS Registrations – Federal and state-level prescribing authority
- Malpractice Insurance – Policy details and coverage limits
- Claims & Settlement History – Documentation of past professional liability claims
- Sanctions & Disciplinary Actions – NPDB queries, OIG exclusions, state disciplinary records
- Employment & Privileges – Work history and hospital affiliations
- Attestations & Disclosures – Signed statements confirming accuracy of information
All verifications must come from primary sources, as defined by the payer or accreditation body.
Examples of Delegating Entities
- Commercial health plans (e.g., Cigna, Aetna, BCBS)
- Managed care organizations (MCOs)
- Preferred provider organizations (PPOs)
- Accountable care organizations (ACOs)
- Medicaid managed care programs
Examples of Delegated Entities
- Hospitals and health systems
- Large provider networks
- Independent practice associations (IPAs)
- NCQA/URAC-accredited CVOs
- Specialty provider networks (dental, vision, behavioral health)
Some organizations, such as IPAs and specialty networks, can serve both roles delegating certain functions while being delegated others.
Delegated Providers
A delegated provider is a healthcare professional whose credentialing is performed by a delegated entity rather than directly by the payer.
For example:
If a hospital holds delegated authority from a payer, its employed physicians are credentialed by the hospital’s internal team. The results are then sent to the payer for network inclusion, eliminating the need for separate payer-led credentialing.
Delegated vs. Non-Delegated Credentialing
| Factor | Delegated Credentialing | Non-Delegated Credentialing |
|---|---|---|
| Authority | Payer authorizes another entity to credential | Payer performs credentialing directly |
| Processing Time | Faster (often 30–45 days) | Longer (60–120+ days) |
| Administrative Control | Higher for provider organization | Controlled by payer |
| Audit Oversight | Regular payer audits | Internal payer reviews |
| Compliance Risk | Higher for delegated entity | Risk borne by payer |
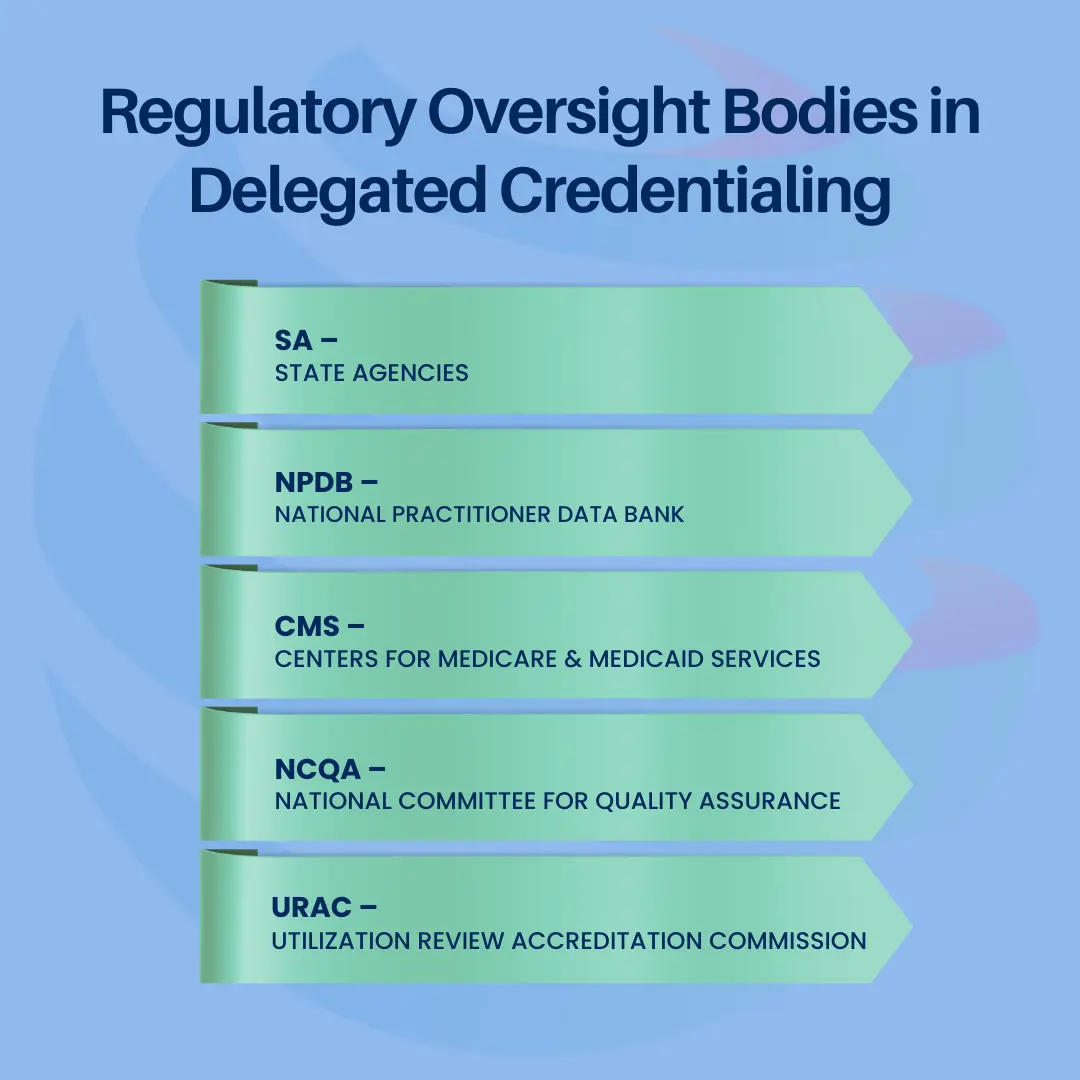
Regulatory Oversight Bodies in Delegated Credentialing
Delegated credentialing in healthcare is not an unregulated process, it operates under strict oversight from multiple authorities to ensure patient safety, compliance, and quality control.
There are five key regulatory and accrediting bodies that influence how delegated credentialing is structured, monitored, and audited:
1- NCQA – National Committee for Quality Assurance
The NCQA is the primary accrediting organization for healthcare quality programs in the U.S. It sets credentialing and delegation standards that many payers require their network partners to follow.
For delegated credentialing, NCQA defines:
- Approved primary source verification (PSV) methods
- Required credentialing file elements
- Oversight and auditing requirements for delegation agreements
Organizations with NCQA accreditation often have an easier time securing delegation status with payers because accreditation serves as proof of compliance and quality standards.
2- CMS – Centers for Medicare & Medicaid Services
CMS is the federal agency that oversees Medicare, Medicaid, CHIP, and ACA-related programs. For delegated credentialing, CMS requires that:
- Medicare Advantage and Medicaid managed care organizations
- All providers undergo credentialing before delivering services to program beneficiaries
- Ongoing monitoring is performed to ensure compliance with participation requirements
Non-compliance with CMS rules can lead to penalties, loss of reimbursement, and removal from federal programs.
3- URAC – Utilization Review Accreditation Commission
URAC is an independent accrediting body that evaluates healthcare organizations, including health plans, provider networks, and credentialing verification organizations (CVOs).
In delegated credentialing, URAC accreditation demonstrates that an organization:
- Maintains a structured and compliant credentialing process
- Uses qualified personnel for verification activities
- Follows consistent decision-making policies for provider participation
Many payers accept URAC accreditation as equivalent to or in place of NCQA accreditation for delegation purposes.
4- State Agencies
Every state has its own department of insurance or health that may impose additional credentialing requirements. These can include:
- Provider license verification rules
- State-specific reporting or renewal timelines
- Background check requirements for certain specialties
Delegated entities must comply with both payer and state rules, ensuring no conflict between contractual obligations and statutory regulations.
5- NPDB – National Practitioner Data Bank
The NPDB is a federal database maintained by the U.S. Department of Health and Human Services. It contains information about:
- Medical malpractice payments
- Adverse licensure actions
- Clinical privilege restrictions
- Federal and state exclusions
Delegated entities are required to query the NPDB during initial credentialing and at re-credentialing to ensure providers have no undisclosed sanctions or disciplinary actions. This step is essential for protecting patient safety and maintaining payer compliance.
Delegation Requirements
To qualify for delegation, an entity typically must:
- Hold NCQA or URAC accreditation (or equivalent credentialing program approval)
- Pass a pre-delegation audit by the payer
- Maintain a credentialing committee for decision-making
- Have documented policies and procedures for initial credentialing, re-credentialing, and ongoing monitoring
- Meet turnaround and accuracy metrics as defined in the delegation agreement
Delegated Credentialing Process
The process generally follows these steps:
1. Develop Internal Credentialing Program
2. Complete Pre-Delegation Audit
3. Sign Delegation Agreement
4. Perform Credentialing Activities
5. Submit Reports to Payer
6. Participate in Ongoing Oversight
Pros and Cons of Delegated Credentialing
Advantages
- Faster provider onboarding
- Eliminates redundant verifications
- Increases provider satisfaction
- Enables quicker payer reimbursement decisions
- Improves administrative control for large organizations
Disadvantages
- Shifts compliance responsibility to delegated entity
- Requires significant investment in staff and infrastructure
- Failure to meet standards can result in loss of delegation
- Regular audits can be resource-intensive
Conclusion
Delegated credentialing has evolved into a widely adopted operational framework for health systems, large provider groups, and payer networks seeking to reduce enrollment timelines and enhance compliance management. By authorizing a qualified delegated entity to perform primary source verification and credentialing determinations, organizations can accelerate provider onboarding, maintain greater administrative control, and improve network responsiveness. However, this approach also transfers significant regulatory and contractual responsibility, requiring strict adherence to NCQA, CMS, URAC, and payer-specific standards to avoid audit deficiencies, financial penalties, or loss of delegation status.
Successful implementation depends on a rigorous readiness assessment and the presence of core operational safeguards. These include accredited credentialing infrastructure, documented and compliant workflows, trained personnel capable of meeting accuracy and timeliness benchmarks, and a proactive internal audit program. When these elements are in place, delegated credentialing becomes a strategic advantage supporting network growth, ensuring regulatory integrity, and sustaining high-quality provider participation.