F41.1 ICD-10 Guide: Avoid Mental Health Billing Errors in 2025
Anxiety disorders affect over 40 million adults in the U.S. each year, making them the most common mental health condition in the country and Generalized Anxiety Disorder (GAD) is among the most frequently diagnosed. According to the Anxiety & Depression Association of America (ADAA), GAD alone impacts 6.8 million adults annually, yet only a fraction receive proper treatment and documentation.
As mental health services expand, the need for accurate medical billing becomes even more critical. And that’s where ICD-10 code F41.1 used for Generalized Anxiety Disorder often becomes a stumbling block. Despite its routine use, this code is frequently misapplied, leading to claim denials, delayed payments, audit triggers, and care disruptions.
If you're a therapist, mental health coder, or billing specialist, you need more than just the right code, you need to understand how to document, justify, and apply F41.1 correctly for both compliance and reimbursement.
In this blog, you’ll learn:
- What F41.1 represents and when it should be used
- How to document symptoms that meet DSM-5 and CMS criteria
- The most common billing mistakes that lead to denials and how to avoid them
- How to distinguish F41.1 from other behavioral codes like F32.x (Depression), F43.x (PTSD), and F90.x (ADHD)
- What every billing note must include to support reimbursement and compliance
What Is F41.1 ICD-10?
- Persistent anxiety and worry lasting six months or more
- At least three associated symptoms, such as:
- Fatigue
- Restlessness
- Sleep disturbances
- Muscle tension
- Difficulty concentrating
- Irritability
- That the anxiety interferes with daily functioning
- That other medical or psychiatric conditions have been ruled out
Common Errors When Coding F41.1
1. Using F41.1 Without Meeting Time or Symptom Criteria
2. Omitting DSM-5 Criteria From Documentation
- Symptoms lasting 6+ months
- At least 3 qualifying symptoms (e.g., fatigue, irritability, sleep issues)
- Clear impact on daily functioning
- Exclusion of other causes
ICD-10 Mental Health Coding Reference Table
Common I10 Denials and Fixes
Understanding GAD in isolation isn’t enough many providers also struggle with codes for MDD, PTSD, and ADHD. Here’s a quick reference table to help you understand how to document and code these conditions correctly:
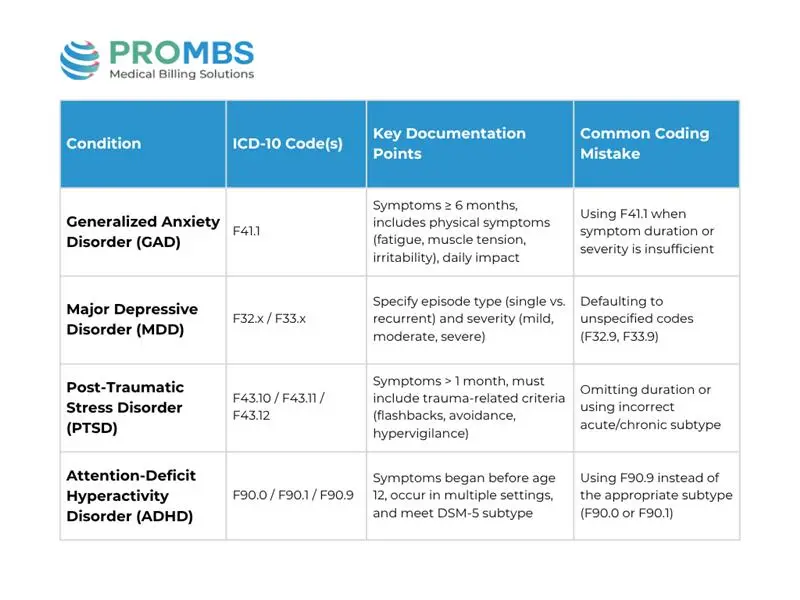
Breakdown of Other Mental Health Codes and Mistakes to Avoid
a) Major Depressive Disorder (MDD)
- Use F32.x for a single episode, F33.x for recurrent.
- Always document:
- Episode type (single vs recurrent)
- Severity (mild, moderate, severe)
- Key symptoms (low mood, appetite changes, sleep disturbances, suicidal ideation)
b)Post-Traumatic Stress Disorder (PTSD)
- Use:
- F43.10 for unspecified PTSD
- F43.11 for acute (symptoms present less than 3 months)
- F43.12 for chronic (symptoms 3 months or longer)
Document trauma exposure, symptom duration, and key behaviors like:
- Nightmares or flashbacks
- Hypervigilance or startle response
- Emotional numbing or avoidance
Common Mistake: Failing to indicate how long the symptoms have lasted.
c)Attention-Deficit Hyperactivity Disorder (ADHD)
- Use:
- F90.0 for inattentive type
- F90.1 for hyperactive-impulsive type
- F90.2 for combined type
- F90.9 only if subtype is unclear
Document:
- Onset before age 12
- Symptoms in two or more settings
- Impact on academic, occupational, or social functioning
Common Mistake: Defaulting to F90.9 when subtype is known or can be inferred from documentation.
How to Improve Documentation for Mental Health Billing
- Symptom description (onset, frequency)
- Impact on life (work, school, social)
- Screening tool results (e.g., GAD-7, PHQ-9)
- Rule-outs of other causes
- DSM-5 diagnostic criteria
- Supports medical necessity
- Proves functional impairment
- Adds objective data to your diagnosis
- Shows that symptoms aren't due to another illness
- Aligns with payer expectations and coding rules
💡 Mental Health Billing Tips (For F41.1 and Beyond)
Use these five key strategies to avoid billing errors:
1. Use Specific ICD-10 Codes
Avoid vague codes unless documentation truly doesn’t support specificity.
2. Match Documentation to DSM-5 Criteria
Always note how symptoms meet official diagnosis standards.
3. Link Diagnosis Codes to Services Rendered
For example, if billing a 60-minute therapy session (90837), ensure the note supports the severity and complexity of the diagnosis (e.g., F41.1 for GAD).
4. Include Comorbid Diagnoses When Relevant
If a patient has GAD and depression, code for both conditions (e.g., F41.1 + F33.1).
5. Know Payer-Specific Rules
Some insurers require modifiers, treatment plans, or medical necessity justifications for behavioral health services.
Why Accurate Coding Does More Than Get You Paid
- Guide clinical treatment plans
- Prove that care is medically necessary
- Support quality reporting in value-based care models
- Prevent audits and overpayment recoupments
Why Choose Pro-MBS for Mental Health Billing
Accurate mental health coding isn’t just about cleaner claims it’s about ensuring patients receive the care they deserve while staying fully compliant with payer guidelines. That’s where our Pro-MBS team stands out.
We specialize in behavioral health billing and understand the complexities behind codes like F41.1 for Generalized Anxiety Disorder. With our support, your practice benefits from:
- Diagnosis codes that align with DSM-5 and CMS criteria
- Proper linkage between ICD-10 and CPT codes
- Fewer denials through accurate documentation and submission
- Protection from audits with proactive compliance checks
- Education and guidance for providers and billing staff
Whether you manage a solo therapy practice or a multi-provider clinic, our team ensures your mental health billing is accurate, efficient, and compliant.