How value-based care impacts Family Medicine Billing is a question that hits hard the moment you walk into a clinic today. You feel it in the patient chart that stretches back ten years. The change did not arrive loudly. It slipped into clinics with quiet steps. A new alert in the EHR. A strange shift in a risk score. A claim that felt different than the ones before it. Then the change grew stronger. It pressed into documentation, coding, and follow-up work until everyone felt its weight.
Family medicine stands closest to long-term patient journeys. When value-based care rose into focus, it struck this specialty with more force than any other. A missed diagnosis suddenly mattered far more. A chronic condition coded poorly could weaken a full year of revenue. CMS and AMA guard the rules, and the expectations set by those groups shape every chart and every note. Outcomes matter. Prevention matters. Consistent detail matters. And the billing world breathes differently because of it.
Why Does Value-Based Care Feel Different in Family Medicine?
You can feel the difference when you step into primary care. Family medicine used to move on simple terms. A visit. A code. A claim. A payment. Now the model asks for proof of impact and proof of change that lasts. This is why how value-based care impacts Family Medicine Billing feels so heavy for family doctors.
You know the patient across years. You see them through calm seasons and storms. You manage their chronic issues and prevent their crises. And now the system watches every detail of that work. It measures how well chronic conditions stay stable. It watches whether preventive screens arrive on time. It studies how quickly patients return after hospital discharge.
Doctors now ask questions they never had to ask before. What is the best way to bill for care that avoids a crisis? How did a missing hypertension code shrink the clinic’s revenue? Why does documentation feel like the heartbeat of the entire payment model? The answers point back to risk scores, coding accuracy, and decision-making that now carry financial weight equal to clinical weight.
What Does Value-Based Care Look Like in Family Medicine in 2025?
To understand how value-based care impacts Family Medicine Billing, you need to see the new payment structure. In 2025, value-based care blends old fee-for-service methods with performance and risk models. It rewards steady care, clean documentation, and strong outcomes.
| Payment Focus | Billing Role | Clinic Impact | Outcomes |
|---|---|---|---|
| Quality and Risk Data | Payment tied to results | Prevention | Screens and gap closure |
| Constant Tracking | Chronic Care | Updated diagnoses | Higher coding precision |
HCC Coding for Family Medicine becomes essential. Value-Based Care Documentation becomes the backbone of every chart review. Risk scores rise when chronic issues are documented well. They fall when notes stay thin.
Why Does Family Medicine Feel the Impact First?
Family medicine feels the pressure first because it holds more responsibility than most specialties. That is why how value-based care impacts Family Medicine Billing often becomes a daily struggle for clinics.
Chronic Conditions Carry Economic Weight
Chronic disease shapes Risk Adjustment in Primary Care. Diabetes. Hypertension. Heart disease. Depression. These conditions define patient risk levels. When coded well, the clinic’s revenue reflects true patient needs. When coded poorly, the loss lasts all year.
High Visit Volume
Family medicine sees more patients than any other specialty. Even small documentation issues repeat themselves. A single missed diagnosis can appear again and again, shaping the entire practice revenue.
Prevention at the Core
How Does Value-Based Care Change the Billing Workflow?
The workflow no longer moves in a straight line. To truly understand how value-cased Care impacts Family Medicine Billing, imagine the process as a circle where coding, documentation, risk scoring, and outcomes feed each other.
Coding
Coding becomes precise and strategic. Each chronic issue must appear clearly and must be supported in the note. The AMA defines the coding rules. CMS defines how risk scores respond. The clinic must satisfy both.
Documentation
Notes gain new depth. They must show complexity, patient needs, medication decisions, and social barriers. Brief notes cause problems. Vague wording leads to poor risk scores.
Claim Submission
Claims still matter, but performance-based services matter as well. Chronic Care Management, Remote Patient Monitoring, Transitional Care Management, and Care Coordination Billing connect the patient to the clinic between visits.
Quality Reporting
MIPS scores, HEDIS data, care gap closure, and patient experience shape bonuses and penalties. Quality metrics become part of the clinic’s financial pulse.
How Does Value-Based Care Transform Clinic Payments?
The clearest view of how value-based care impacts Family Medicine Billing appears in the new payment structure. Payment rises and falls with outcomes.
| Model | Meaning | Impact |
|---|---|---|
| Capitation | Paid each month per patient | Steady revenue |
| Shared Savings | Reward for lowering total costs | Depends on accurate coding |
| Pay-for-Performance | Metrics drive bonuses | Lives on care quality |
Now it is not the number of visits that matters. It is the number of outcomes achieved. Blood pressure control. A1C trends. Cancer screening completion. Follow-up after discharge. These measures now carry financial weight.
How Does Value-Based Care Shape Denials?
Denials change shape under this model. They come not only from billing errors but also from weak documentation. This is one of the most revealing aspects of how value-based care impacts Family Medicine Billing.
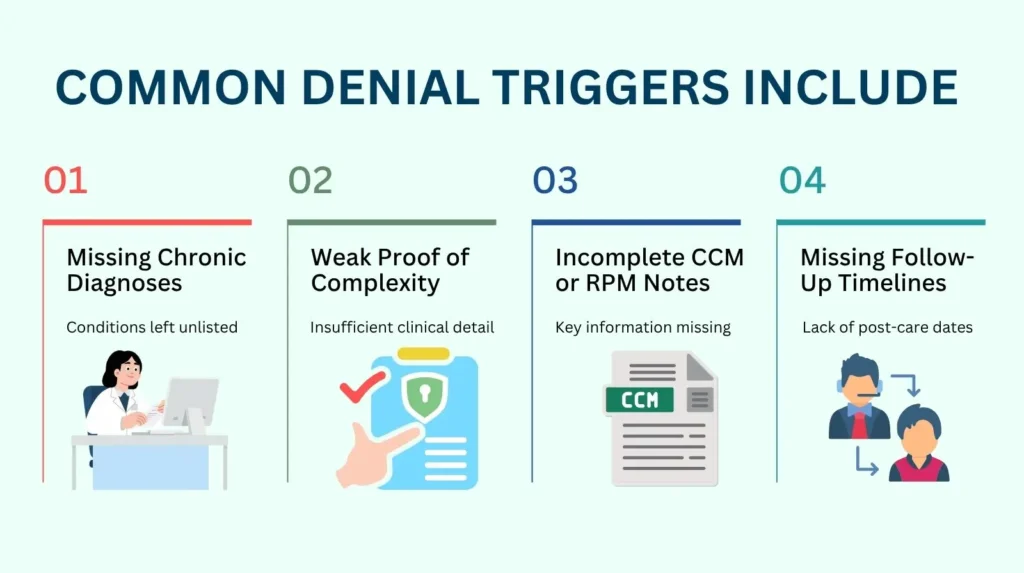
Common denial triggers include:
- Missing chronic diagnoses
- Weak proof of complexity
- Incomplete CCM or RPM notes
- Missing follow-up timelines
- Missing preventive care documentation
Denials do not fall at random. They come from the places you ignored. A missing word. A thin note. A chronic condition left unnamed. Each one leaves a mark. Each one grows into a pattern. They move with purpose. They wait in the silence of your charts. Then they strike, clean and precise, the moment your documentation shows a crack.
New Billing Opportunities Under Value-Based Care
Value-based care also opens doors. Many clinics do not realize how many new billing paths now exist. Understanding these paths is a key part of how value-based care impacts Family Medicine Billing.
Chronic Care Management: Steady care between visits becomes a lifeline for patients with chronic disease. CCM keeps their story from slipping into chaos and brings predictable revenue to the clinic.
Complex CCM: Some patients carry heavier burdens and need deeper monitoring. Complex CCM captures that weight and ensures the work behind it never goes unseen or unpaid.
Transitional Care Management: The days after a hospital discharge are fragile. TCM guides patients across that narrow bridge so they do not fall back into crisis and the clinic earns for guiding them safely home.
Remote Patient Monitoring: RPM keeps the clinic’s eyes open when the patient is far away. It turns daily readings into insight and transforms quiet risks into early action.
Annual Wellness Visits: These visits map the road ahead for the year. They reveal gaps, guide prevention, and help the clinic anchor value-based performance before trouble grows.
Behavioral Health Integration: Many patients carry wounds that do not appear on lab results. BHI brings mental health into the center of care so the clinic treats the whole person, not the symptom alone.
Care Coordination Billing: When teams move together, patients stay steady. Care coordination billing rewards clinics for weaving specialists, follow-ups, and plans into one clear path.
Hybrid Payment Models in Primary Care: Some clinics walk between two worlds: fee-for-service and value-based care. Hybrid models let them adapt with balance so revenue stays steady while outcomes rise.
These services support long-term care and connect patients to the clinic between visits. They reflect priorities defined by CMS.
What Clinics Must Change to Stay Ahead?
To survive the shift, clinics must change the way they move. Not tomorrow. Now. The system grows sharper each month, and it watches every choice. If a clinic wants to stand firm, it must strengthen the foundation first. And that starts with the work done behind every chart.
Clinics need:
Consistent updates to chronic condition lists: These lists cannot grow stale. Each missed diagnosis weakens the year ahead.
Care coordinators who track care gaps: Someone must guard the spaces where trouble hides.
Preventive care dashboards: Prevention fails when it is forgotten. Dashboards keep it in sight.
Risk score monitoring: Risk shifts like weather. Someone must watch the sky.
AI-supported documentation checks: Even the best notes miss things. AI sees what long days make easy to overlook.
Clear VBC Billing Workflows: Without structure, the system fractures.
Accurate SDOH entries: Social needs shape risk. Risk shapes payment.
Reliable follow-up systems: Patients fall through cracks when no one guards the gap.
These changes are not optional. They shield the clinic, sharpen its work, and keep its revenue from slipping away. And when they come together, they reveal the true path through the world shaped by how value-based care impacts Family Medicine Billing.
How Does AI Strengthen Value-Based Care Documentation?
AI becomes a powerful tool in this world. It identifies missing diagnoses, scans notes for risk issues, predicts documentation gaps, and warns against errors that could trigger audits. It helps clinicians stay aligned with CMS expectations. This is another crucial layer in How Value-Based Care Impacts Family Medicine Billing. AI does not replace clinical skill. It strengthens it by seeing what busy teams often overlook.
The Cultural Shift Beneath It All
The deepest truth about how value-based care impacts Family Medicine Billing is cultural. Billing can no longer sit quietly in the back office. It becomes the responsibility of the entire care team.
- A missed screen changes revenue.
- A missed diagnosis changes a risk score.
- A missing detail changes a year.
Clinics that move together stay strong. They share the weight. They guard each other’s blind spots. No task drifts. No detail slips. The work holds steady because every hand is raised, every voice aligned. Clinics that work in silos fall. They fall slowly at first. A missed note. A forgotten call. A code left unsaid. Then the cracks spread. The gaps widen. And the whole system breaks under the pressure no one faced together.
Can Pro-MBS Change the Future of How Value-Based Care Impacts Family Medicine Billing?
The pain shows itself quietly at first. A risk score that slips lower than expected. A chronic condition that never made its way into the note. A missed screen that turns into a lost bonus. Then it grows. CMS requirements tighten. AMA coding rules sharpen. Documentation spreads like a forest of tangled branches. And the clinic feels the weight of it all. This is exactly where how value-Based care impacts Family Medicine Billing hits hardest. Not with noise, but with slow, steady pressure that wears a practice down over time.
This is where Pro-MBS becomes the guide you wish you had from the start. Our teams step in like steady hands in a storm. We tighten risk adjustment accuracy so scores stop slipping through cracks. We clean documentation that once felt impossible to control. We build workflows that turn frantic value-based tasks into calm, predictable systems. Chronic care management becomes structured. Coding grows sharper. Care gaps close before they cost you.
With Pro-MBS at your side, the path through How Value-Based Care Impacts Family Medicine Billing becomes less a burden and more a strategy. The question remains, as all important questions do. What will your clinic choose to become now that the path ahead is clear?
Frequently Asked Questions
How does Value-Based Care change Family Medicine Billing?
Value-based care shifts the ground beneath every clinic. Payment no longer follows visits. It follows outcomes, risk scores, and the truth written in the chart. That is why Family Medicine Billing now depends on accuracy, not speed. Missed diagnoses drain revenue. Thin notes weaken risk. Every gap becomes a cost. Pro-MBS can steady your billing workflow before those cracks spread.
Why is Risk Adjustment so important in Primary Care?
Risk adjustment is the center of the value-based model. When chronic conditions are captured cleanly, the system sees the real weight of patient needs. When they are missed, the score collapses. That is why Risk Adjustment In Primary Care demands discipline, precision, and steady updates. Clinics that ignore it lose more than they realize. Let Pro-MBS guard your risk scores before they fall again.
How does HCC Coding affect revenue in Family Medicine?
HCC codes carve the path for the entire year’s payment. When HCC Coding For Family Medicine is sharp, risk aligns with patient need. When coding weakens, revenue drops even if care stays strong. Every diagnosis must be supported, updated, and captured with clarity. With Pro-MBS, your HCC accuracy becomes a weapon, not a weakness.
What Quality Measures matter most in Family Medicine?
The system watches every step. A1C levels. Blood pressure control. Cancer screens. Follow-up timelines. These Quality Measures In Family Medicine shape bonuses, penalties, and performance scores. Missed screens cost money. Missed follow-ups cost trust. Only consistent detail survives the pressure. Pro-MBS can build the workflows that keep every measure in sight.
How do Care Management services support Value-Based Reimbursement?
Care no longer ends when the visit does. Chronic Care Management Billing, Care Coordination Billing, and Remote Patient Monitoring guide patients through the quiet days when risk grows unseen. These services anchor Value-Based Reimbursement and stabilize outcomes. When used well, they turn uncertainty into control. Pro-MBS can manage these programs so your clinic earns for the care it already delivers.
What should clinics change to thrive in Value-Based Care?
Clinics must move as one. They need clean codes, strong notes, and risk scores watched like weather. They need clear dashboards and VBC Billing Workflows that hold firm under pressure. The clinics that adapt rise. The ones that resist break beneath the weight. Stand with Pro-MBS and build the structure your clinic needs to thrive.
