Discover the fascinating 350-year history of medical billing and coding, from plague-ravaged London to today's digital healthcare systems. This comprehensive exploration reveals how a simple need to track mortality evolved into the complex coding systems that power modern healthcare.
350 Years of Medical Coding: Key Milestones
| Year | Milestone |
|---|---|
| 1662 | John Graunt publishes analysis of Bills of Mortality |
| 1830s | Dr. William Farr proposes standardized cause-of-death classification |
| 1893 | Jacques Bertillon creates the first international mortality classification |
| 1948 | WHO adopts ICD-6 as the first global disease classification |
| 1966 | AMA introduces the CPT system |
| 1977 | ICD-9 is released, adding morbidity codes |
| 1990s | CPT expands to include E/M, radiology, and lab codes |
| 2015 | ICD-10 implemented in the US (after delays) |
| 2020s | AI and NLP technologies transform coding practices |
Early Beginnings: 17th Century England and the Bills of Mortality
The remarkable story of medical coding begins in the darkest chapter of London's history. During the devastating Great Plague of 1665-1666, which claimed approximately 100,000 lives—nearly a quarter of London's population—an urgent need arose to systematically track and understand the causes of death sweeping through the city.
John Graunt, a haberdasher turned statistician, became the unlikely pioneer of medical data classification. Working with the London Bills of Mortality, he developed the first systematic approach to categorizing causes of death using numerical codes. These bills, originally created by parish clerks who recorded deaths in their districts, were transformed by Graunt into a powerful tool for understanding disease patterns.
What made Graunt's work revolutionary wasn't just the numerical coding system itself, but his analytical approach to the data. He identified patterns in mortality, seasonal variations in disease, and even demographic trends that would later form the foundation of epidemiology. His 1662 publication "Natural and Political Observations Made upon the Bills of Mortality" established the principle that health data, when properly coded and analyzed, could reveal crucial insights about public health.
This early coding system, though rudimentary by today's standards, established several key principles that remain central to medical coding: the need for standardized categories, the importance of accurate data collection, and the power of systematic classification to reveal health patterns. The Bills of Mortality represented humanity's first serious attempt to quantify and understand disease through coded data.
19th Century Advances: Standardizing Cause of Death Classification
The 19th century brought unprecedented advances in medical understanding and the urgent need for international standardization. Dr. William Farr, England's first medical statistician, recognized that inconsistent classification systems across different regions made it impossible to compare health data meaningfully. In the 1830s, he proposed the revolutionary concept of uniform classification that could be applied globally.
Farr's vision extended beyond simple death recording to encompass a comprehensive understanding of disease patterns. He advocated for classifications based on anatomical site, general disease type, and specific conditions—a framework that would influence medical coding for centuries to come. His work demonstrated that standardized coding wasn't merely administrative convenience but a crucial tool for advancing medical science and public health policy.
The breakthrough came in 1893 when Jacques Bertillon, Chief of Statistical Services in Paris, introduced the Bertillon Classification of Causes of Death. This system, adopted by the International Statistical Institute, became the first truly international health classification standard. The Bertillon Classification featured 161 categories organized into groups, providing unprecedented detail and consistency in mortality data collection.
This system's adoption marked a pivotal moment in medical history. Countries across Europe and North America began implementing the Bertillon Classification, creating the first global database of comparable health information. The system underwent revisions every decade, reflecting advances in medical knowledge and the growing sophistication of disease classification. By the early 20th century, the foundation was laid for modern epidemiology and evidence-based medicine, all built upon the principle of systematic, coded health data.
The International Classification of Diseases (ICD) Emerges
Global Standardization
The World Health Organization's formalization of the International Classification of Diseases in 1948 marked the beginning of truly global health data standardization. This momentous development transformed medical coding from a collection of regional systems into a unified international language of health.
ICD Version History Overview
| ICD Version | Year Introduced | Notable Feature |
|---|---|---|
| ICD-1 | 1900 | First international mortality classification |
| ICD-6 | 1948 | WHO’s first version, included morbidity |
| ICD-9 | 1977 | Diagnostic and injury coding |
| ICD-10 | 1990 (Global), 2015 (US) | Expanded specificity and code structure |
| ICD-11 | 2022 (Global) | Digital-first, AI-ready, genomic coding |
The evolution from ICD-9 to modern systems represents one of healthcare's most significant technological advancements. ICD-9, introduced in 1977, expanded beyond mortality to encompass clinical diagnoses and injuries, featuring approximately 13,000 codes. This expansion reflected the growing complexity of medicine and the need for more detailed clinical documentation.
The ICD system's global adoption created remarkable consistency in health data collection. Hospitals in Manchester could now meaningfully compare their outcomes with facilities in Mumbai or Montreal. This standardization enabled large-scale epidemiological studies, international disease surveillance, and evidence-based treatment protocols that transcended national boundaries.
Perhaps most significantly, the ICD system established the principle that accurate coding was essential for quality healthcare delivery. The detailed classification requirements forced healthcare providers to document more precisely, leading to improved patient care, better resource allocation, and more effective public health interventions. The ICD's influence extended far beyond coding, fundamentally changing how medicine approached documentation, research, and quality improvement.
Development of Procedural Coding: The CPT System
The American Medical Association's development of Current Procedural Terminology (CPT) in 1966 addressed a critical gap in medical coding. While diagnostic codes captured what was wrong with patients, there was no standardized system for describing what healthcare providers actually did to help them. The CPT system emerged from the practical need to document medical services accurately and consistently.
Initially focused on surgical procedures, CPT codes provided a standardized vocabulary for describing medical interventions. The system's genius lay in its systematic approach: each code represented a specific service, with detailed descriptions that eliminated ambiguity about what was performed. This precision was crucial not only for billing purposes but also for medical research, quality assurance, and healthcare planning.
The CPT system's evolution reflected the rapid expansion of medical capabilities throughout the latter half of the 20th century. As new procedures were developed—from minimally invasive surgeries to advanced diagnostic techniques— new codes were added to capture these innovations. The system grew from a simple procedural reference to a comprehensive catalogue of medical services, including evaluation and management codes, radiology procedures, laboratory tests, and emerging technologies.
Perhaps most importantly, CPT codes established the direct link between medical coding and healthcare economics. By providing precise descriptions of services rendered, the system enabled accurate billing, appropriate reimbursement, and meaningful cost analysis. This connection between coding accuracy and financial sustainability made medical coding an integral part of healthcare administration, transforming it from a purely clinical documentation tool into a crucial business function that would shape the entire healthcare industry.
Technological Evolution: From Paper to Digital Systems
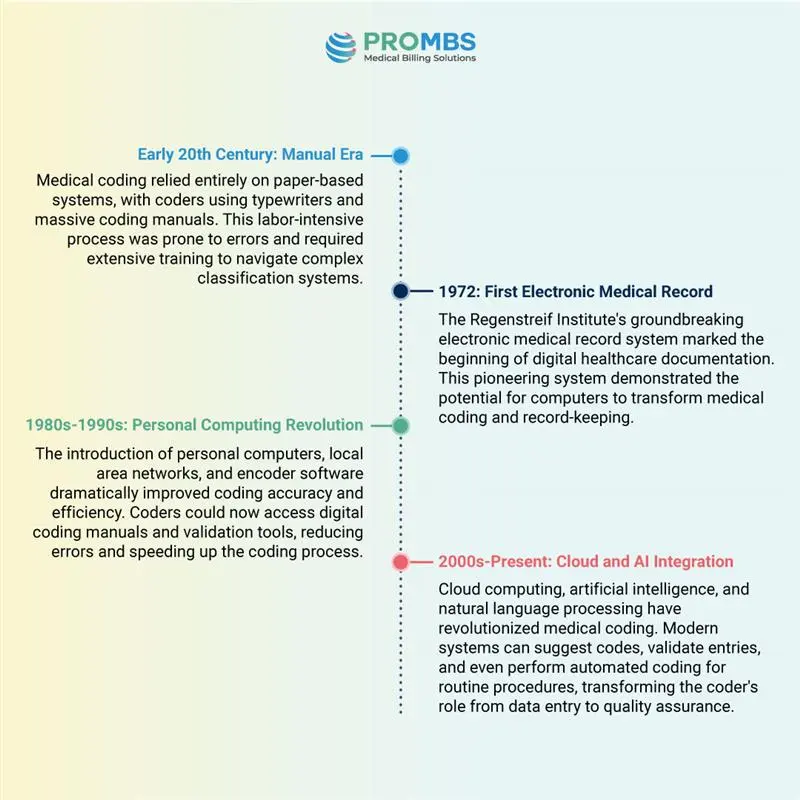
Cloud computing, artificial intelligence, and natural language processing have revolutionized medical coding. Modern systems can suggest codes, validate entries, and even perform automated coding for routine procedures, transforming the coder's role from data entry to quality assurance.
The technological transformation of medical coding represents one of healthcare's most dramatic efficiency improvements. What once required hours of manual searching through thick coding manuals can now be accomplished in minutes with sophisticated software tools. This evolution has not only improved accuracy but has also made medical coding more accessible to new practitioners and enabled the rapid expansion of healthcare services.
Modern coding systems integrate seamlessly with electronic health records, automatically populating relevant clinical data and suggesting appropriate codes based on physician documentation. This integration has created a more holistic approach to healthcare documentation, where coding becomes part of the clinical workflow rather than a separate administrative task.
Transition from ICD-9 to ICD-10: Necessity and Impact
The transition from ICD-9 to ICD-10 represented one of the most significant upheavals in medical coding history. By the early 2000s, ICD- 9's limitations had become critical barriers to effective healthcare delivery. The system's antiquated structure, with only 13,000 codes, simply couldn't accommodate the complexity of modern medicine. High claim denial rates, coding ambiguities, and insufficient clinical detail were creating substantial financial and operational challenges for healthcare providers.
ICD-9 vs ICD-10: Key Differences
| Feature | ICD-9 | ICD-10 |
|---|---|---|
| Code Format | Numeric | Alphanumeric |
| Total Codes | ~13,000 | ~68,000+ |
| Code Length | 3–5 digits | Up to 7 characters |
| Laterality | Not supported | Supported |
| Combination Codes | Limited | Common |
| Specificity | Low | High |
| US Implementation | 1979 | 2015 |
ICD-10's introduction brought revolutionary changes to medical coding. The new system's alphanumeric structure expanded coding capacity exponentially, with seven-character codes providing unprecedented specificity. Combination codes allowed coders to capture multiple conditions and their relationships in a single code, while laterality indicators specified which side of the body was affected. These improvements dramatically reduced ambiguity and enhanced clinical documentation quality.
The impact of this transition extended far beyond coding departments. Healthcare providers discovered that ICD-10's enhanced specificity led to more accurate reimbursement, reduced claim denials, and improved quality reporting. The system's detailed clinical information enabled better population health management, more precise epidemiological studies, and enhanced patient safety initiatives.
Implementation challenges were significant, requiring extensive staff training, system upgrades, and workflow modifications. However, the benefits quickly became apparent. Healthcare organizations reported improved revenue cycle management, enhanced clinical decision- making support, and better compliance with regulatory requirements. The transition demonstrated that investing in advanced coding systems could yield substantial returns in healthcare quality and efficiency.
Modern Medical Billing & Coding: Roles and Responsibilities
Clinical Analysis
Modern medical coders serve as clinical data analysts, meticulously reviewing patient records to extract relevant diagnoses, procedures, and treatments. This requires deep understanding of medical terminology, anatomy, and disease processes.
Compliance Assurance
Coders ensure adherence to complex regulatory requirements, including HIPAA privacy rules, Medicare guidelines, and insurance protocols. They serve as guardians of healthcare data integrity and legal compliance.
Revenue Optimization
Accurate coding directly impacts healthcare revenue through proper reimbursement claims. Coders work closely with billing departments to maximise appropriate revenue while maintaining ethical standards.
Quality Improvement
Coded data drives quality metrics, patient safety initiatives, and clinical outcome studies. Coders contribute to continuous improvement efforts across healthcare organizations.
The specialization within medical coding has reached unprecedented levels. Coders now focus on specific medical specialties such as orthopedics, neurology, cardiology, and ambulatory surgery, developing deep expertise in complex procedural coding and specialty-specific documentation requirements. This specialization ensures accuracy in increasingly complex medical procedures and emerging treatment modalities.
Integration with electronic health records has transformed the coder's workflow. Modern coders work within sophisticated EHR systems that provide real-time access to clinical documentation, laboratory results, and imaging studies. This integration enables more accurate code assignment and facilitates communication between coding staff and clinical providers when documentation clarification is needed.
The modern medical coder's role extends beyond traditional coding to encompass revenue cycle management, denial management, and audit preparation. As healthcare organizations face increasing financial pressures, coders have become strategic partners in maintaining financial stability while ensuring compliance with ever-evolving regulatory requirements.
The Future: AI, Automation, and Expanding Opportunities
Artificial Intelligence Integration
AI-assisted coding tools are revolutionizing the profession, reducing manual errors and dramatically accelerating coding processes. Natural language processing algorithms can analyses physician documentation and suggest appropriate codes, while machine learning systems continuously improve their accuracy based on coder feedback and validation.
The integration of AI doesn't eliminate the need for human coders but rather elevates their role. Coders are transitioning from routine data entry to sophisticated quality assurance, audit management, and denial resolution. This evolution requires new skills in AI system management, data analysis, and complex problem-solving.
Expanding opportunities in medical coding reflect the growing complexity of healthcare delivery. Remote coding positions have become increasingly common, offering flexibility and access to specialized roles regardless of geographic location. The demand for certified coders continues to grow, driven by aging populations, expanding healthcare services, and increasing regulatory requirements.
Emerging technologies are creating new coding challenges and opportunities. Telemedicine, robotic surgery, precision medicine, and genomic therapies require new coding approaches and specialized expertise. The profession is adapting to capture the nuances of these advanced medical interventions while maintaining the accuracy and specificity that modern healthcare demands.
Professional development in medical coding now emphasizes continuous learning and adaptation. Coders must stay current with evolving coding guidelines, new medical procedures, and advancing technology platforms. This dynamic environment offers exciting career progression opportunities for those willing to embrace change and continue developing their expertise.
Summary: The Enduring Importance of Medical Billing & Coding
Historical Foundation
From 17th century plague records to global health standards, medical coding has evolved through centuries of innovation and international collaboration, establishing the critical infrastructure for modern healthcare data management.
Clinical Excellence
Accurate coding ensures precise healthcare delivery, appropriate reimbursement, and meaningful clinical research, serving as the backbone of evidence-based medicine and quality patient care.
Future Innovation
As healthcare continues evolving with AI, telemedicine, and precision medicine, medical coding adapts to capture new complexities whilst maintaining the accuracy and integrity essential for optimal patient outcomes.
The remarkable journey of medical billing and coding spans over three and a half centuries, from John Graunt's pioneering work during London's Great Plague to today's sophisticated AI- assisted coding systems. This evolution reflects humanity's persistent drive to understand, categories, and improve healthcare through systematic data collection and analysis.
Medical Coding Then vs Now
| Element | Historical Era | Modern Era |
|---|---|---|
| Tools Used | Handwritten logs, mortality bills | EHRs, cloud-based encoders, AI platforms |
| Primary Purpose | Track death counts | Clinical accuracy, billing, compliance |
| Code Volume | < 200 (Graunt/Bertillon) | 70,000+ (ICD-10-CM, CPT, HCPCS) |
| Coding Role | Clerical or statistical | Clinical analyst, auditor, revenue agent |
| Coding Format | Free text or numeric categories | Structured, alphanumeric, laterality |
| Workflow | Manual post-care documentation | Real-time integrated with EHRs |
What began as a desperate attempt to comprehend mortality patterns during a devastating plague has transformed into a sophisticated global system that enables precise healthcare delivery, accurate billing, and meaningful clinical research. The progression from simple numerical death codes to today's complex alphanumeric systems demonstrates how medical coding has consistently adapted to meet the growing demands of advancing medical science.
The field's resilience and adaptability are perhaps its most remarkable characteristics. Through wars, pandemics, technological revolutions, and shifting healthcare paradigms, medical coding has continuously evolved whilst maintaining its core mission: providing accurate, standardized documentation that supports quality patient care and effective healthcare management.
Today's medical coding professionals stand at the intersection of clinical expertise, technological innovation, and regulatory compliance. They serve as guardians of healthcare data integrity, ensuring that the rich clinical information generated by modern medicine is accurately captured, appropriately coded, and effectively utilized for patient care, research, and public health initiatives.
Looking forward, medical coding will undoubtedly continue evolving to meet future healthcare challenges. Whether addressing emerging diseases, new treatment modalities, or revolutionary technologies, the profession's fundamental purpose remains constant: transforming complex clinical information into standardized, actionable data that drives better health outcomes for individuals and populations worldwide. The deep origins of medical billing and coding have created an enduring legacy that will continue shaping healthcare for generations to come.