What Is Acute Kidney Injury (AKI)?
Acute Kidney Injury (AKI) is a sudden and potentially reversible decline in renal function that can lead to severe electrolyte imbalance, fluid retention, and increased mortality if untreated. It often develops in hospitalized or critically ill patients and may result from sepsis, nephrotoxic medications, trauma, or obstructive uropathy.
ICD-10 Code for Acute Kidney Injury (N17.9), Unspecified
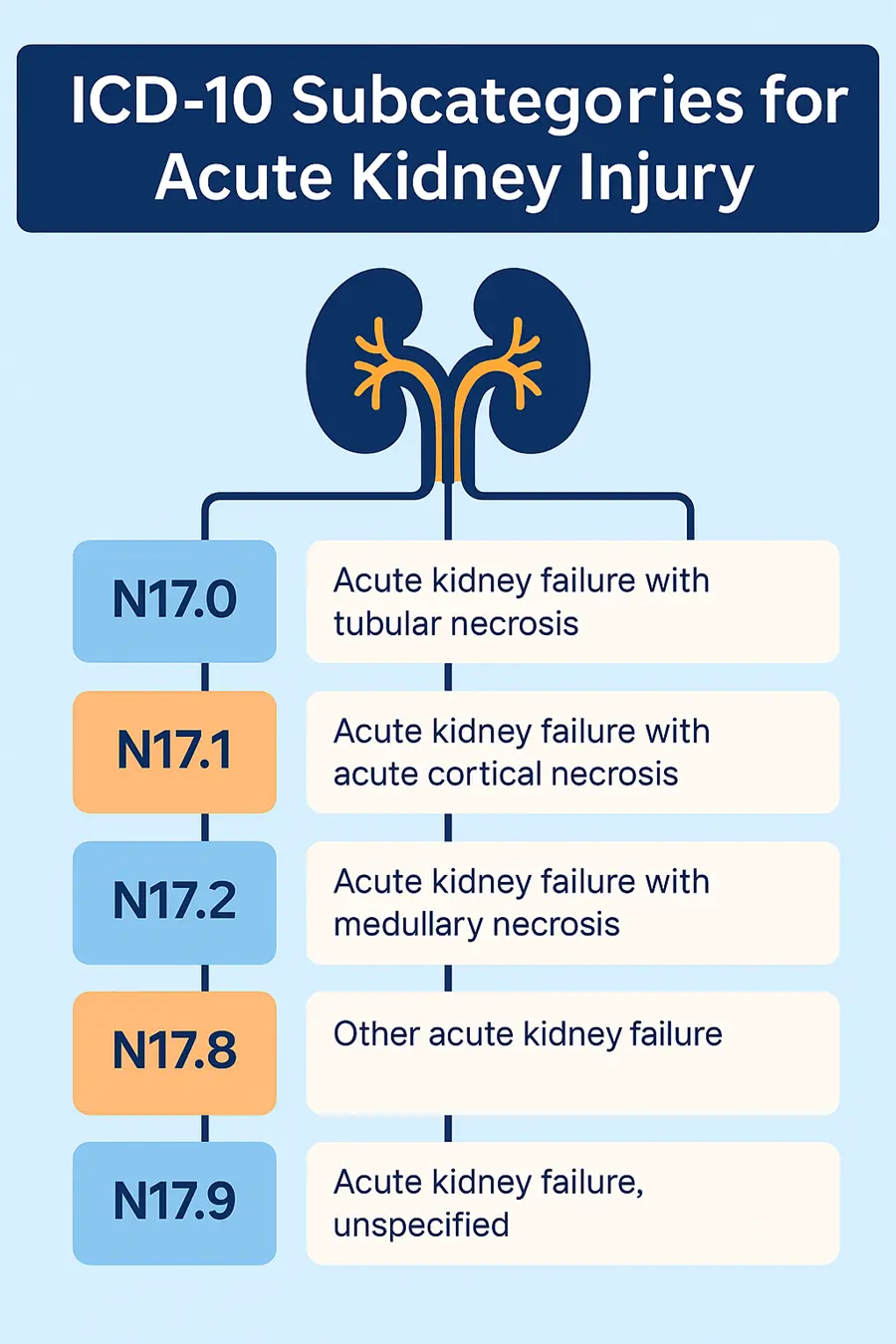
ICD-10 Code for Acute Kidney Injury (N17.9) is used to classify a diagnosis of acute kidney failure (AKF) or acute kidney injury (AKI) when the provider has not documented a specific cause, mechanism, or site of the renal injury. The term “unspecified” indicates that the clinical notes confirm AKI but do not provide further detail required to use a more specific subcategory code (N17.0–N17.8).
This code should not be used when the provider documents a specific cause or stage of AKI, such as acute tubular necrosis (ATN), cortical necrosis, medullary necrosis, or post-renal obstruction. In those cases, the more specific ICD-10 subcategory must be assigned to ensure coding accuracy, maintain medical necessity, and reduce denial risk.
Clinical Use Case:
ICD-10 Code for Acute Kidney Injury (N17.9) should be used only when:
- The provider confirms AKI, but
- There is no mention of underlying pathology (e.g., tubular necrosis), anatomical site (e.g., cortical, medullary), or known cause (e.g., sepsis, dehydration, nephrotoxic agents)
- Clinical descriptors required for N17.0–N17.8 (such as ischemic origin or anatomical detail) are absent in documentation
ICD-10 Subcategories for Specific AKI Types
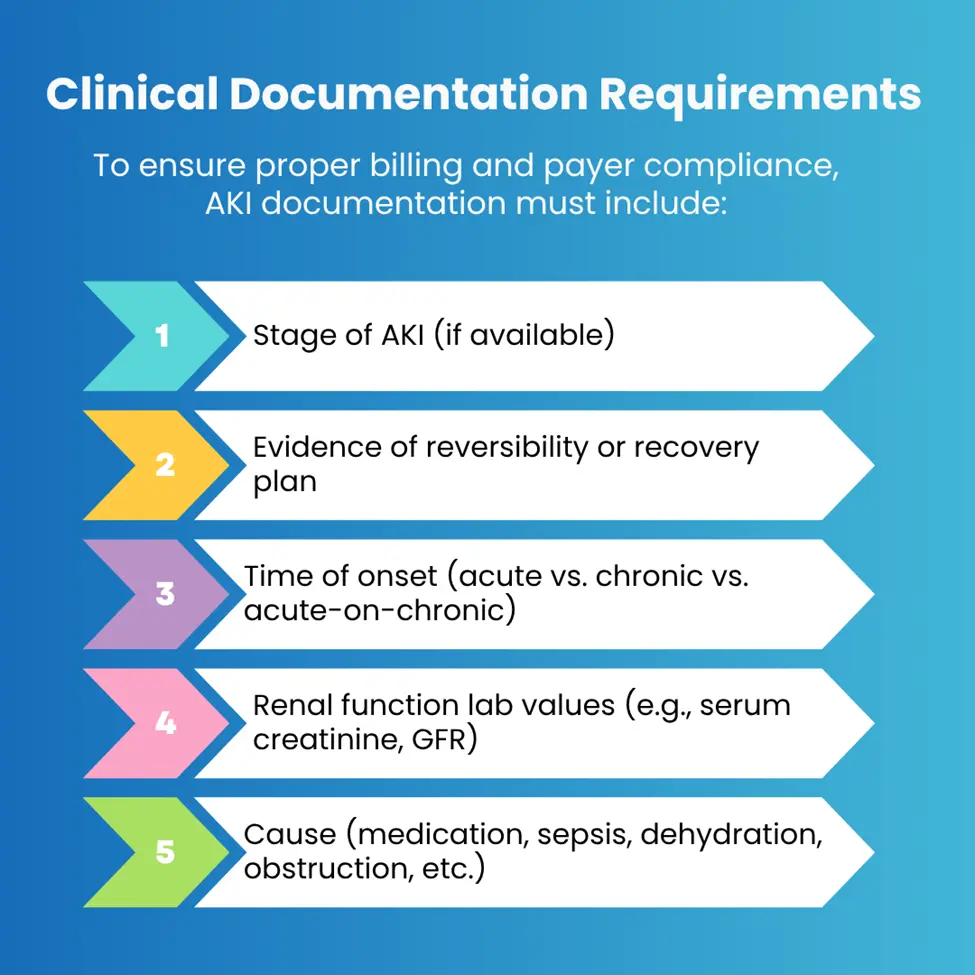
Clinical Documentation Requirements
Common Coding Errors and Denials in AKI Billing
When billing for ICD-10 Code for Acute Kidney Injury (N17.9), accurate coding and supporting documentation are essential to avoid denials. Payers often reject claims due to the following common issues:
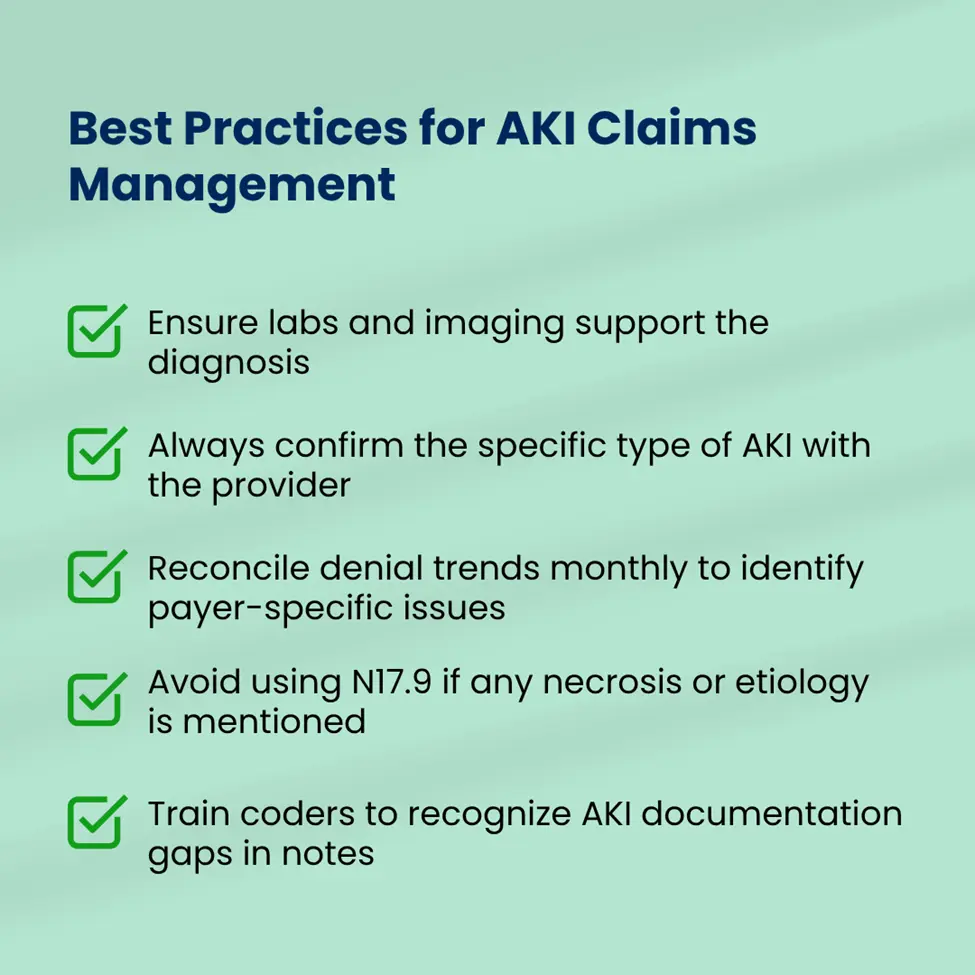
Use of Unspecified Code (N17.9) When Specificity Is Available
Many coders default to N17.9 – Acute kidney failure, unspecified even when clinical documentation provides enough detail for a more specific code (e.g., N17.0 for tubular necrosis). Unspecified codes raise red flags with payers and may result in down coded or denied claims.
Missing Medical Necessity in Provider Notes
Even with the correct ICD-10 code, claims may be denied if the clinical rationale for the diagnosis is not clearly documented. This includes lab results, creatinine trends, or clinical findings supporting AKI onset.
AKI Listed as a Secondary Diagnosis Without Correlation to Treatment
Confusion with Chronic Kidney Disease (CKD) Codes (N18.X)
Coders sometimes confuse AKI (N17.X) with CKD (N18.X), especially when a patient has a complex renal history. Billing both without documentation confirming acute-on-chronic kidney injury can trigger rejections or audits.
Relevant CPT Codes Used in AKI Billing
| Feature | Offset | Refund/Recoupment |
|---|---|---|
| Initiated By | Payer | Payer or Provider |
| Processing Method | Deducted from current or future payments | Separate refund issued or requested |
| Notification Format | ERA line item or RARC/CARC codes | Letter of overpayment |
| Impact on Workflow | Inflates open AR until manually cleared | Less disruptive if proactively handled |
Payer Policy Insights and Reimbursement Considerations
Most commercial and Medicare Advantage plans follow NCD 220.1 and LCD-specific policies related to acute renal failure management. Key considerations include:
- AKI must be supported by labs (BUN, Creatinine, eGFR)
- Claims may require chart notes during pre-payment review
- Dialysis services may trigger separate audit requests
- Modifier usage for same-day visits and labs must be accurate
Best Practices for AKI Claims Management
How Pro-MBS Helps with AKI Coding and Billing
Pro-MBS ensures acute kidney injury (AKI) claims are coded with maximum specificity and compliance. Our certified coders review documentation for accuracy, verify lab correlations (e.g., creatinine, BUN, eGFR), and flag misuse of unspecified codes like N17.9 when detailed subcodes apply. We help providers align diagnosis codes with CPT services and meet payer documentation standards to prevent denials and audits.
We also assist in identifying recurring denial patterns, managing payer-specific billing edits, and maintaining clean claims through proactive credentialing, modifier accuracy, and proper code linkage. Whether inpatient or outpatient, our team safeguards your AKI revenue cycle from front-end intake to backend reimbursement.