Congestive Heart Failure (CHF) is more than just a frequent clinical diagnosis; it is a high-stakes focal point for Medicare reimbursement and payer audits. With millions of annual hospitalizations and billions in healthcare spending, the pressure to assign the correct ICD 10 code for Congestive Heart Failure has never been higher.
For providers, the challenge lies in the details. A generic diagnosis is no longer enough. To ensure clean claims and accurate risk adjustment, documentation must distinguish between specific manifestations, such as Diastolic CHF ICD 10 codes versus systolic or combined failure.
Inaccurate Congestive Heart Failure ICD 10 reporting doesn’t just skew quality data - it triggers claim denials, invites compliance scrutiny, and results in significant financial leakage. This guide bridges the gap between clinical documentation and technical coding, providing the clarity needed to optimize your revenue cycle and stay compliant in an increasingly audited landscape.
What is Congestive Heart Failure (CHF) and What Are Its Symptoms?
Congestive Heart Failure (CHF) is a chronic, progressive condition where the heart’s pumping efficiency is compromised, leading to fluid buildup (congestion) in the lungs and peripheral tissues. From a billing perspective, identifying the clinical indicators is the first step in selecting the correct ICD 10 code for Congestive Heart Failure.
Common symptoms include:
Because Congestive Heart Failure ICD 10 codes are often tied to the severity of the patient's presentation, documentation must reflect these common symptoms:
- Shortness of breath (dyspnea), especially on exertion or lying flat
- Fatigue and reduced exercise tolerance
- Swelling (edema) in the legs, ankles, and feet
- Rapid or irregular heartbeat
- Persistent cough or wheezing due to pulmonary congestion
The Documentation Gap: Why Specificity Matters
For coders and auditors, the term "CHF" used in isolation is often viewed as an unspecified diagnosis. To capture the highest level of specificity - such as a Diastolic CHF ICD 10 code versus a systolic or combined failure - the provider must document the acuity (acute, chronic, or acute-on-chronic) and the type of heart failure.
What is the ICD 10 Code for Congestive Heart Failure?
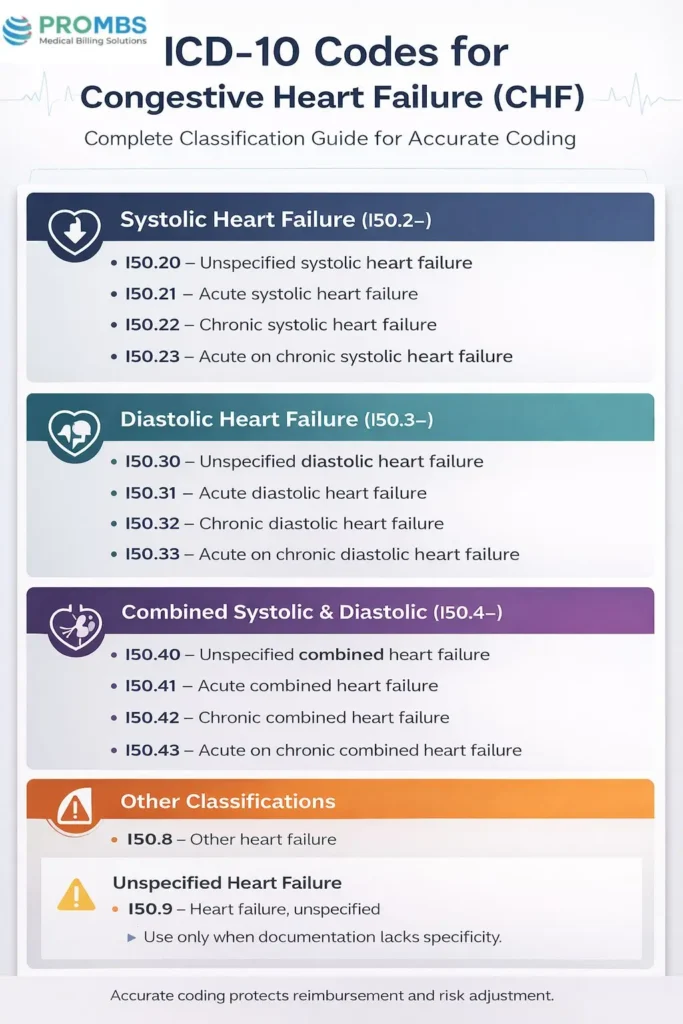
The primary ICD 10 code for Congestive Heart Failure is I50.9 - Heart failure, unspecified. However, ICD-10-CM requires more precise documentation when available. Congestive Heart Failure is broken down into multiple categories:
ICD 10 Codes for Congestive Heart Failure (CHF)
| Category | ICD-10 Code | Description |
|---|---|---|
| Systolic Heart Failure (I50.2–) | I50.20 | Unspecified systolic heart failure |
| I50.21 | Acute systolic heart failure | |
| I50.22 | Chronic systolic heart failure | |
| I50.23 | Acute on chronic systolic heart failure | |
| Diastolic Heart Failure (I50.3–) | I50.30 | Unspecified diastolic heart failure |
| I50.31 | Acute diastolic heart failure | |
| I50.32 | Chronic diastolic heart failure | |
| I50.33 | Acute on chronic diastolic heart failure | |
| Combined Systolic & Diastolic (I50.4–) | I50.40 | Unspecified combined heart failure |
| I50.41 | Acute combined heart failure | |
| I50.42 | Chronic combined heart failure | |
| I50.43 | Acute on chronic combined heart failure | |
| Other Heart Failure | I50.8 | Other heart failure |
| Unspecified Heart Failure | I50.9 | Heart failure, unspecified |
Which ICD 10 Chapter Covers CHF Coding?
Congestive Heart Failure falls under:
- ICD-10-CM Chapter IX: Diseases of the Circulatory System (I00–I99)
- Subcategory I50 - Heart failure
This chapter also includes related conditions such as ischemic heart disease, arrhythmias, and hypertensive heart disease. Coders should carefully review whether CHF is documented as a consequence of hypertension (e.g., I11.0 - Hypertensive heart disease with heart failure). In such cases, sequencing rules apply, and both hypertension and CHF codes may be required.
What CPT Codes Are Used for CHF Management?
While ICD-10 codes capture the diagnosis, CPT codes describe the services rendered for Congestive Heart Failure management.
CPT Codes for CHF Management:
| CPT Code | Description |
|---|---|
| 99221–99223 | Initial hospital care for CHF admissions |
| 99231–99233 | Subsequent hospital visits during CHF management |
| 93306 | Echocardiography, complete, often performed to assess CHF severity |
| 36415 | Collection of venous blood for laboratory testing (BNP/NT-proBNP) |
| G2211 | Medicare add-on code for complex chronic care management (frequently applicable in CHF cases) |
What Are the Treatment Options for CHF Patients?
The management of Congestive Heart Failure (CHF) requires a multi-faceted approach combining pharmacologic therapy, device-based interventions, and lifestyle modifications. From a revenue cycle perspective, every treatment must be documented and linked correctly to the specific ICD 10 code for Congestive Heart Failure to establish medical necessity and prevent payer denials.
Pharmacologic Management
Medication is the cornerstone of CHF care. For accurate billing, the documentation must reflect the patient's response to these drugs, especially during acute exacerbations.
- Diuretics (e.g., Furosemide): Used to manage fluid overload.
- ACE Inhibitors/ARBs: Essential for improving cardiac output.
- Beta-Blockers: Critical for reducing mortality in Congestive Heart Failure ICD 10 cases.
- Aldosterone Antagonists: Often used when there is a reduced ejection fraction.
Billing Tip:
When administering IV diuretics (like Lasix) during an admission, ensure the J1940 code is linked to the specific CHF diagnosis. Use CPT codes 96365-96366 for infusion services to ensure full reimbursement for the resources consumed during treatment.
Surgical Procedures and Device Therapy
Advanced cases, particularly those involving Diastolic CHF ICD 10 or systolic dysfunction with low ejection fractions, may require surgical intervention.
- Implantable Cardioverter-Defibrillators (ICDs): CPT 33249 is frequently used for insertion to prevent sudden cardiac death.
- Pacemakers: To regulate arrhythmias associated with heart failure.
- Ventricular Assist Devices (VADs): Mechanical pumps used as a "bridge to transplant" or destination therapy.
Compliance Note:
These high-value procedures face heavy payer scrutiny. Documentation must clearly state the ejection fraction (EF) and NYHA functional class to justify the procedure under the primary Congestive Heart Failure ICD 10 diagnosis.
Lifestyle Modification and Chronic Care Management
Non-pharmacologic strategies are vital for long-term stability and offer additional billing opportunities through specialized CPT codes.
- Sodium & Fluid Restriction: To prevent rapid decompensation.
- Daily Weight Monitoring: A key clinical indicator used to justify "Acute-on-Chronic" status if a sudden weight gain occurs.
- Chronic Care Management (CCM): Providers can often bill CPT 99490 (20 minutes of non-face-to-face care per month) for patients with CHF, provided the care plan is tied to the appropriate ICD 10 codes.
What Documentation is Required for Accurate CHF Coding?
Accurate assignment of the ICD 10 code for Congestive Heart Failure depends entirely on the specificity of the provider’s clinical notes. Coders are prohibited from "assuming" a diagnosis based on lab results alone; the documentation must explicitly state the type and acuity to avoid the dreaded "unspecified" code (I50.9), which frequently triggers payer audits and medical necessity denials.
The "Specificity Triple Threat"
To capture the most accurate Congestive Heart Failure ICD 10 code, documentation must address these three pillars:
- Type (The "What"): Is it Systolic (HFrEF), Diastolic (HFpEF), or Combined heart failure?
- Acuity (The "When"): Is the condition Acute, Chronic, or Acute-on-Chronic (Exacerbated)?
- Cause (The "Why"): Is the failure due to hypertension, ischemic cardiomyopathy, or valvular disease?
Documentation Checklist for Providers
To ensure clean claims and high-fidelity risk adjustment, clinical notes should include:
- Ejection Fraction (EF) Percentage: Essential for distinguishing between systolic and Diastolic CHF ICD 10 codes.
- Acuity Indicators: Terms like "decompensated," "exacerbation," or "fluid overload" support acute status codes.
- Clinical Validity Evidence: Reference BNP levels, chest X-ray findings (e.g., cephalization, Kerley B lines), and echocardiogram results to strengthen the diagnosis against payer "clinical validation" audits.
- Linkage of Comorbidities: Clearly link CHF to the underlying causes. For example, documenting "Hypertensive Heart Disease with Heart Failure" changes the coding sequence to the I11.0 series.
Coder's Note:
If a provider documents "CHF" but the echo shows a preserved ejection fraction of 60%, the coder should query the provider to confirm if a Diastolic CHF ICD 10 code (I50.3-) is appropriate, rather than billing an unspecified code.
How Can Providers Avoid Claim Denials When Billing ICD 10 Code for Congestive Heart Failure?
Denials in Congestive Heart Failure coding often stem from insufficient documentation or ICD-10/CPT mismatches.
Common payer rejection reasons include:
- Unspecified coding - Using I50.9 when documentation supports a more specific diagnosis.
- Sequencing errors - Not sequencing hypertension before CHF when both are present.
- Medical necessity issues - Procedures like echocardiography are billed without supporting CHF diagnosis codes.
- Incomplete linkage - Failure to connect CHF ICD-10 codes with appropriate CPT codes.
- Risk Adjustment Validation - Medicare Advantage and other risk-adjusted payers often deny if documentation does not support the Hierarchical Condition Category (HCC 85: Congestive Heart Failure). Lack of specificity can result in loss of HCC credit, lower risk scores, and denied claims.
Denial Prevention Strategies:
- Always code to the highest specificity.
- Query providers if documentation is unclear.
- Apply payer-specific CHF coding guidelines.
- Regularly audit CHF claims for accuracy and compliance.
How Pro-MBS Optimizes Your Revenue Cycle for CHF
Navigating the complexities of the ICD 10 code for Congestive Heart Failure requires more than just software; it requires specialized Cardiovascular Coding expertise. Pro-MBS provides a dedicated team of certified coders who understand the clinical nuances between systolic dysfunction and a specific Diastolic CHF ICD 10 diagnosis.
Why Leading Practices Partner with Pro-MBS:
- Precision in Code Assignment: We apply rigorous payer-specific edits to ensure every Congestive Heart Failure ICD 10 code is sequenced correctly with comorbidities like hypertension (I11.0) or chronic kidney disease (I13.x).
- Audit-Ready Documentation: Our team identifies gaps where "unspecified" codes are being overused and works with your providers to capture the clinical specificity (Acute vs. Chronic) that payers demand.
- Seamless RCM Integration: We integrate directly with your EHR and RCM platforms to accelerate claim scrubbing and maintain a high first-pass acceptance rate.
- Proactive Denial Management: By managing the technical triggers for RAC and payer audits, we stop denials before they happen, safeguarding your revenue integrity.
By outsourcing the technical burden of the ICD 10 code for Congestive Heart Failure to Pro-MBS, your clinical team can refocus on patient outcomes while our experts ensure you are fully and fairly reimbursed for the complex care you provide.
Frequently Asked Questions
Why should you avoid using I50.9 as the primary ICD 10 code for Congestive Heart Failure?
Using I50.9 signals a lack of clinical detail, which often triggers claim denials or audits. Specific codes like chronic systolic failure satisfy compliance, support risk adjustment, and ensure full reimbursement for the complex care your practice provides to patients.
How does documenting ejection fraction impact Diastolic CHF ICD 10 code selection?
Ejection fraction (EF) is the clinical bridge to the correct code. A preserved EF supports a Diastolic CHF ICD 10 diagnosis, while a reduced EF indicates systolic failure. Precise EF documentation prevents coding queries and validates medical necessity during payer reviews.
What are the sequencing rules for the ICD 10 code for Congestive Heart Failure and hypertension?
ICD-10-CM guidelines presume a causal link between hypertension and heart failure. You must sequence the hypertensive heart disease code (I11.0) first, followed by the specific Congestive Heart Failure ICD 10 code. Incorrect sequencing leads to automated claim rejections and denials.
How does the acuity of heart failure affect the final ICD 10 code for Congestive Heart Failure?
Acuity determines the final digit of the ICD 10 code for Congestive Heart Failure. Acute-on-chronic exacerbations often qualify as Major Comorbidities (MCCs), which increase DRG weights and payment. Identifying the correct temporal status is vital for accurate inpatient reimbursement.
Which CPT codes should you link to the ICD 10 code for Congestive Heart Failure to ensure payment?
Link CPT codes like 93306 or 99490 directly to specific heart failure diagnoses. For acute care, pair HCPCS J1940 with an acute Congestive Heart Failure ICD 10 code. Proper linkage demonstrates that treatments were a direct response to the patient's condition.