What Is Iron Deficiency Anemia?
Iron deficiency anemia is a condition where the body lacks enough iron to make adequate hemoglobin, limiting the blood’s ability to carry oxygen. This causes common symptoms such as fatigue, weakness, and trouble concentrating.
What Is the ICD 10 Code for Iron Deficiency Anemia?
The ICD 10 code for Iron Deficiency Anemia is D50.9, which is used to document and bill anemia caused by iron deficiency. This code identifies iron deficiency as the underlying cause of anemia so payers can evaluate medical necessity, clinical accuracy, and reimbursement eligibility.
Iron deficiency anemia is very common in the United States. This diagnosis matters because billing depends on it. The ICD 10 Code for Iron Deficiency Anemia decides if a claim gets paid or denied.
When teams use the wrong ICD 10 Code for Iron Deficiency Anemia, claims fail. Payments slow. Stress grows for providers and patients.
Low iron in food, long-term blood loss, pregnancy, and health problems often cause iron deficiency anemia. Without iron, the body cannot make healthy red blood cells.
Patients feel tired. They feel weak. They lose focus. Billing must show this clearly using the right ICD 10 Code for Iron Deficiency Anemia.
When anemia lasts over time, providers may use chronic anemia ICD 10 to show the full condition. Clear notes help coders choose the correct ICD 10 Code.
When details go missing, claims do not match the visit. Payers deny them. This guide explains iron deficiency anemia, coding rules, and how to avoid billing mistakes.
What Is the ICD 10 Code for Iron Deficiency Anemia ?
The ICD 10 code for Iron Deficiency Anemia is reported under the ICD-10-CM category D50.
The most commonly used diagnosis codes include:
- D50.0 – Iron deficiency anemia due to chronic blood loss
- D50.8 – Other iron deficiency anemias
- D50.9 – Iron deficiency anemia, unspecified
For 2026, CMS has not introduced new D50 codes, but payer scrutiny remains high. Claims billed with D50.9 are closely reviewed when clinical notes or laboratory results support a specific cause, such as blood loss, pregnancy, or malabsorption.
Providers and coders are expected to assign the most specific D50 code supported by documentation and lab evidence to reduce denials, audits, and reimbursement delays.
What Symptoms Support the ICD 10 Code for Iron Deficiency Anemia?
- Fatigue and weakness
- Shortness of breath
- Dizziness
- Pale skin
- Cold hands and feet
- Chest pain in life-threatening cases
What Is the Correct ICD 10 Code for Iron Deficiency Anemia in 2025?
What ICD-10 Code Applies Most Often? The main code is D50.9 – Iron deficiency anemia, unspecified.
When should coders use it? Use it only when records confirm iron deficiency anemia but do not name the cause. Should teams rely on it often? No. Payers expect details when notes allow.
Why does this matter? Different medical conditions, autoimmune diseases, or a chronic condition can cause anemia. Low hemoglobin levels affect how blood cells carry oxygen and lead to symptoms of anemia and other side effects. Coders must also avoid D64.9, which reflects anemia of chronic disease, not iron deficiency.
Which Specific ICD 10 Codes Apply to Iron Deficiency Anemia?
Why does code choice matter? Specific codes lower denial risk and support medical necessity, especially when anemia develops due to a known cause.
Why avoid overusing D50.9? Payers often review unspecified codes. Clear notes allow coders to choose better options, especially when anemia appears due to Chronic Kidney Conditions or GI bleeding.
The ICD 10 Code for Iron Deficiency Anemia has more than one code. Each code is used for a different reason. Using the right code helps avoid billing problems. The table below shows the main codes and when to use them.
| ICD-10 Code | Description | When to Use |
|---|---|---|
| D50.0 | Iron deficiency anemia secondary to blood loss (chronic) | When anemia results from long-term blood loss (e.g., GI bleeding, heavy menstrual cycles). |
| D50.1 | Sideropenic dysphagia | For Plummer-Vinson syndrome: iron deficiency anemia with difficulty swallowing. |
| D50.8 | Other iron deficiency anemias | For documented iron deficiency anemia not fitting into D50.0 or D50.1 categories. |
| D50.9 | Iron deficiency anemia, unspecified | Use only when the cause is not documented. Avoid frequent use to reduce denials. |
Common Coding Mistakes With ICD 10 Code for Iron Deficiency Anemia
You already know what iron deficiency anemia is. You also know the ICD-10 codes used for it. Now you need to see where coding goes wrong and why the payment stops.
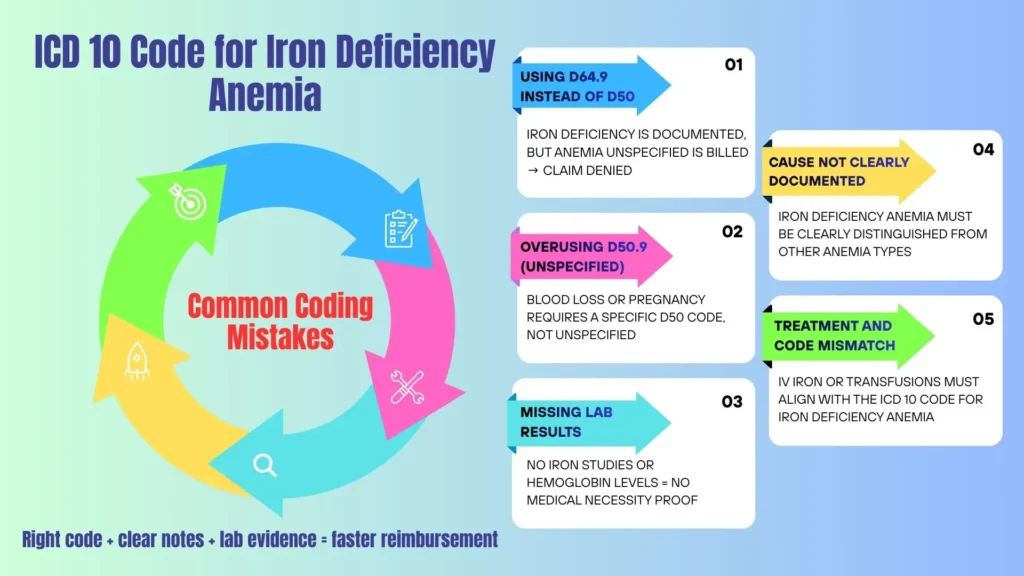
Common mistakes include:
- Using D64.9 instead of D50
Coders pick anemia unspecified when iron deficiency is clear. Payers reject these claims under the 2026 ICD-10-CM diagnosis code rules. - Using D50.9 too often
When notes show blood loss or pregnancy, coders must use a specific D50 code. Coding guidelines expect clear details. - Missing lab results
Claims fail when iron tests or hemoglobin results are missing. Labs prove the problem is real. - Not naming the cause
Notes must show what caused the anemia. Iron deficiency is not the same as hemolytic anemia or sickle cell. Each uses a different code. - Wrong match between care and code
IV iron or transfusions must match the ICD 10 code for iron deficiency anemia. When they do not, payers deny the claim.
These mistakes slow payment. They raise stress. Clear notes, correct codes, and lab proof keep claims moving and revenue steady.
Which ICD 10 Chapter Covers Iron Deficiency Anemia Codes?
Where does iron deficiency anemia appear in ICD-10-CM? It falls under Chapter 3: Diseases of the blood and blood-forming organs (D50–D89).
Why does this matter? Chapter rules guide code order when anemia appears with other conditions, such as kidney disease, cancer, or chronic kidney disease CKD, where anemia may appear alongside erythropoietin resistant anemia EPO.
Does ICD 10 Code for Iron Deficiency Anemia Affect Risk Adjustment?
Risk Adjustment and HCC Coding
Does iron deficiency anemia raise HCC scores? No. D50.x codes do not map directly to CMS-HCC categories.
Does documentation still matter? Yes. Clear records help explain treatment decisions and support audit defense. Lab proof and provider notes show why care occurred, especially when anemia develops alongside chronic kidney disease CKD.
Which CPT and HCPCS Codes Link to the ICD 10 Code for Iron Deficiency Anemia?
What do CPT and HCPCS codes show? They describe tests and treatments linked to the diagnosis. Why must codes match? Payers require a clear link between the diagnosis and services for reimbursement purposes.
CPT Billing Notes
Why do infusion claims deny? Coders often misuse modifiers. Claims must support modifier use when billing iv infusion or other intravenous infusion services with E/M visits.
How Is the ICD 10 Code for Iron Deficiency Anemia Treated?
How do providers choose treatment? Severity, cause, and patient tolerance guide care.
Oral Iron Supplementation
Providers often start with iron supplements. Why? Oral therapy works for mild cases and supports long-term recovery when tolerated.
Dietary Modification
Why change diet? Proper iron intakes from food support recovery and help restore iron levels over time.
Intravenous (IV) Iron Therapy
When oral treatment does not work, providers use IV iron. Iron sucrose goes straight into the blood. It raises iron levels faster. This helps patients with long-term illness who need repeat IV infusions.
Blood Transfusion
When does transfusion apply? Providers use blood transfusion only for severe anemia. They use it when symptoms get worse fast or become life-threatening.
Blood Transfusion Billing Notes: Coders often report CPT 36430. Why does detail matter? Payers require proof of severity, lab values, and the amount of blood given.
Coverage and Documentation Considerations
What do payers require before approval? Most want lab results such as hemoglobin, ferritin, and total iron binding capacity.
Claims deny when blood test results are missing. Payers cannot see the need for care. IV therapy often needs approval. This is common for patients with chronic kidney disease.
What Documentation Is Required for ICD 10 Code for Iron Deficiency Anemia?
Clear notes matter first. Why? They decide if the claim gets paid. Providers must clearly name iron deficiency anemia and list the cause when they know it.
Why avoid vague terms like “anemia NOS”? These words raise denial risk and block use of a billable specific code.
What should the chart include? Providers should add blood test results like a complete blood count and iron tests. They should also note how severe the anemia is.
Is there chronic blood loss? Is this anemia in pregnancy? Do chronic diseases play a role, such as anemia in chronic kidney disease? Clear answers guide clean billing.
Why list related conditions? Kidney disease, long-term illness, and blood loss explain the anemia. These details place the diagnosis under diseases of the blood and blood forming organs and certain disorders involving the immune mechanism. Clear notes protect payment.
Strong records support correct coding from 2016 through 2026.
How Can Coders Avoid Denials With ICD 10 Code for Iron Deficiency Anemia?
Why do denials happen? Coders use unclear codes. Labs stay missing. Simple errors slip through. These issues block payment.
What should coders do first? Read the note closely. Does it show chronic blood loss? Does it link to chronic diseases or anemia in pregnancy?
If yes, coders should choose a billable specific code instead of a general one.
Why do labs matter so much? Labs prove the diagnosis. Without them, claims fail. Infusion claims also fail when the modifier details stay wrong. Simple checks prevent delays.
How do teams protect revenue long-term? They run regular audits. They review notes often. These steps reduce risk every year from 2016 2017 2018 2019 2020 2021 2022 2023 2024 2025 2026 billable specific codes.
Clear notes and careful coding keep claims clean and payments steady.
Why Choose Pro-MBS for Iron Deficiency Anemia Coding Support
Why choose Pro-MBS? Our teams specialize in anemia and infusion billing. We apply accurate ICD 10 Code for Iron Deficiency Anemia, match CPT and HCPCS code rules, and maintain a 98% clean claim rate.
We handle authorizations. We manage infusion billing. We fix denials. We track A/R. We follow rules from Medicare and private payers.
Providers focus on care. We protect payment accuracy.
Frequently Asked Questions
What is the most specific ICD 10 Code for Iron Deficiency Anemia?
The most specific ICD 10 code depends on the underlying cause documented in the medical record. While D50.9 (Iron deficiency anemia, unspecified) is frequently used, it is often flagged by payers for lack of detail. For higher reimbursement accuracy, providers should use D50.0 for anemia due to chronic blood loss or D50.8 for other specified iron deficiency anemias (such as those related to diet or malabsorption).
Can I use D50.9 for iron deficiency anemia in 2026?
Yes, D50.9 remains a valid, billable ICD-10 code in 2026, but its use should be limited. Medical billers and coders should only assign D50.9 when the clinical documentation confirms an iron deficiency but fails to identify a specific cause. Overusing unspecified codes can lead to increased claim denials and medical necessity audits from insurance payers.
How do you code iron deficiency anemia caused by chronic blood loss?
To code iron deficiency anemia resulting from chronic blood loss (such as GI bleeds or heavy menstruation), you must use ICD-10 code D50.0. It is important to distinguish this from D62 (Acute posthemorrhagic anemia), which is used for sudden, massive blood loss. Accurate documentation of the "chronic" nature of the blood loss is required to support the D50.0 diagnosis.
What is the difference between ICD-10 codes D50.9 and D64.9?
The primary difference is the cause of the anemia. D50.9 is strictly for anemia caused by a lack of iron. D64.9 is a more general code for "Anemia, unspecified" and is used when the type of anemia (iron deficiency, hemolytic, vitamin B12 deficiency, etc.) is not documented. Coding D64.9 when lab results specifically show low ferritin or iron levels is considered a coding error and may result in claim rejection.
Does ICD 10 Code for Iron Deficiency Anemia (D50.9) map to an HCC code for risk adjustment?
No, The ICD 10 Code for Iron Deficiency Anemia codes under the D50 category, which do not currently map to CMS-HCC (Hierarchical Condition Category) models. While these codes do not directly increase risk adjustment scores, accurate coding is still vital. Proper documentation of D50 codes supports the medical necessity of expensive treatments like IV iron infusions (CPT 96365) and frequent laboratory monitoring.