Quick Summary: Peripheral Artery Disease ICD 10 Coding
Peripheral artery disease ICD 10 coding requires high specificity to support medical necessity and avoid denials. The correct ICD 10 code for peripheral arterial disease must reflect severity, obstruction, and associated complications. When arterial blockage is documented, an ICD 10 code for peripheral arterial occlusive disease may be more appropriate than an unspecified ICD 10 peripheral artery disease code. CMS frequently audits PAD claims due to high procedural costs, making accurate ICD-10 and CPT linkage essential for compliant reimbursement.
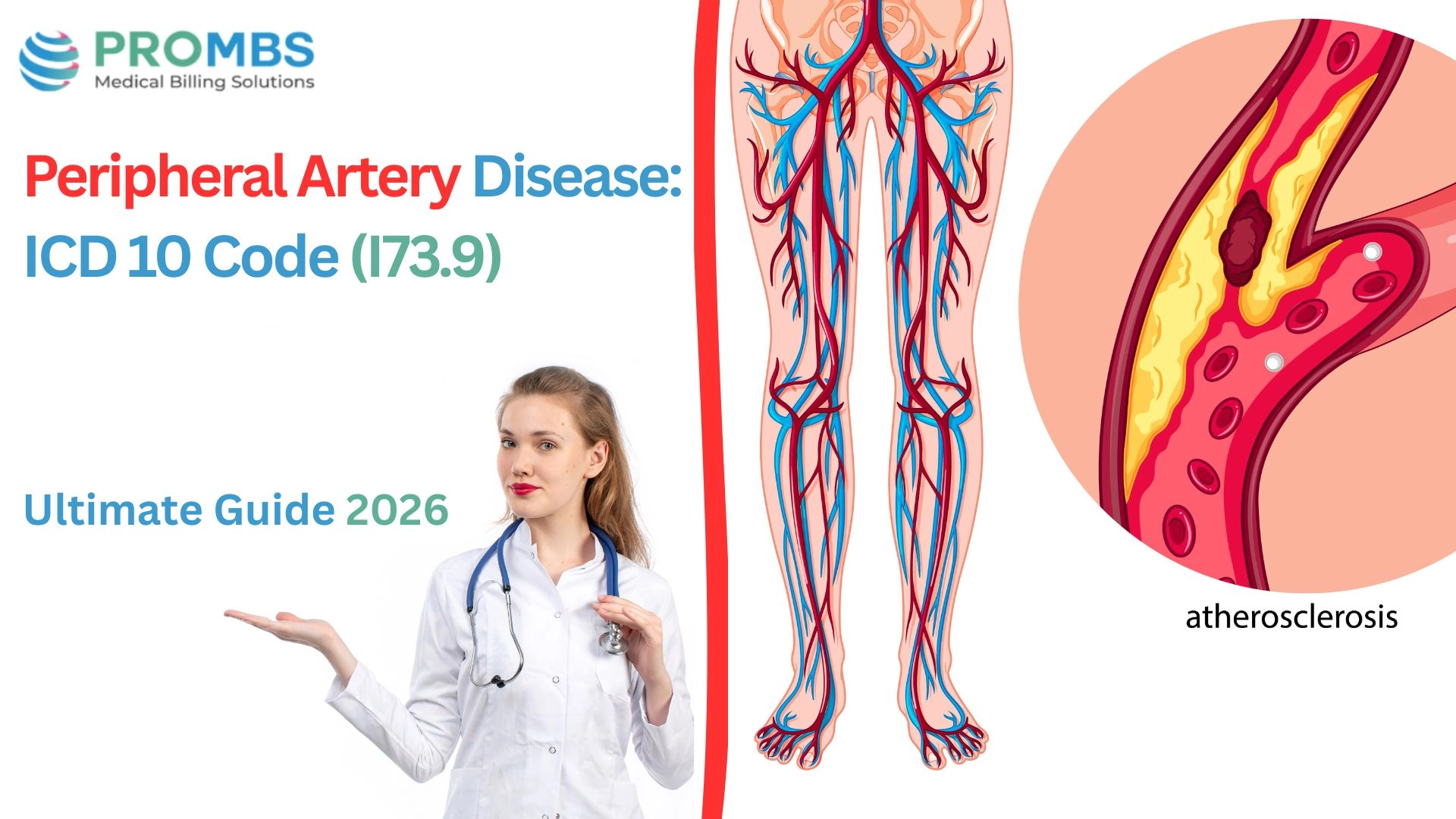
Peripheral arterial disease (PAD), also known as peripheral vascular disease, is a chronic circulatory condition caused by narrowed arteries that reduce blood flow to the extremities.
According to the Centers for Disease Control and Prevention (CDC), PAD affects more than 6.5 million adults in the United States over age 40, making it a significant public health concern. From a coding perspective, understanding the Peripheral Artery Disease ICD 10 classification framework is essential for accurate reporting and appropriate risk adjustment.
From a reimbursement and compliance standpoint, PAD is one of the most scrutinized vascular diagnoses. The Centers for Medicare & Medicaid Services (CMS) frequently audits vascular claims because of the high costs associated with diagnostic imaging, endovascular procedures, and long-term management.
Selecting the correct peripheral arterial disease ICD 10 code, or when clinically supported, a specific ICD 10 code for peripheral arterial occlusive disease, directly impacts claim approval and medical necessity validation. Using a nonspecific ICD 10 peripheral artery disease designation can increase denial exposure, especially when procedural CPT codes require clear diagnostic linkage.
Did You Know?
The American Heart Association (AHA) reports that individuals with PAD face a six- to seven-fold higher risk of major cardiovascular events. This elevated risk profile highlights the importance of a precise ICD 10 code for peripheral arterial disease selection, particularly when documenting atherosclerosis, limb ischemia, or related vascular complications.
Accurate ICD-10 and CPT alignment strengthens payer confidence and supports approval for advanced diagnostics and revascularization services.
What Is Peripheral Artery Disease ICD 10 and What Symptoms Should Be Documented?
Peripheral arterial disease is not a uniform diagnosis. For payers, specificity in documentation determines whether ICD-10 coding aligns with CPT services and supports medical necessity.
If documentation lacks detail, coders may be limited to a broad peripheral artery disease ICD 10 classification, often defaulting to I73.9. This unspecified option under the broader ICD 10 peripheral artery disease category increases denial exposure and weakens audit defensibility.
The Centers for Medicare & Medicaid Services (CMS) consistently emphasizes that vague PAD documentation leads to improper payments and recoupments.
Accurate selection within the peripheral arterial disease ICD 10 hierarchy depends entirely on the level of clinical detail provided. Below is how each documentation component affects billing accuracy and risk.
| Element | Clinical Explanation | ICD-10 & Billing Impact | Denial Risk if Missing |
|---|---|---|---|
| Type of PAD (atherosclerosis of extremities, intermittent claudication, critical ischemia) | PAD ranges from mild narrowing with exertional pain (claudication) to life-threatening ischemia with ulcers or gangrene. | Type determines whether coders assign I70.2xx (with claudication), I70.23x (with ulceration), or I70.26x (with gangrene). | Claim defaults to I73.9 unspecified, which payers may deny as “non-specific.” |
| Location of Disease (femoral, popliteal, iliac, multiple sites) | PAD may affect one vessel (femoral) or multiple segments. Laterality (right, left, bilateral) also matters. | Specificity enables CPT linkage for angioplasty (37225 femoral, 37226 iliac). | Procedures like stenting can be denied if the operative site isn’t documented. |
| Severity of Symptoms (mild claudication vs gangrene) | Severity ranges from pain with walking → rest pain → tissue loss or gangrene. | Severity level impacts both ICD-10 coding and medical necessity for invasive interventions. | Angioplasty or bypass may be denied without clear symptom severity progression. |
| Associated Risk Factors (diabetes, smoking, hyperlipidemia, hypertension) | PAD rarely exists alone; comorbidities drive progression and justify aggressive management. | Documenting risk factors supports chronic care management CPT 99490 and strengthens inpatient justification. | Without risk factors, claims may be denied for “lack of medical necessity” for imaging or revascularization. |
Did You Know?
The American Heart Association reports that one in three adults over age 50 with diabetes has PAD. This underscores the importance of pairing an accurate peripheral artery disease ICD 10 classification with properly documented comorbid conditions to ensure compliant and defensible reimbursement.
What Does the ICD 10 Code for Peripheral Arterial Disease Mean?
The most commonly reported peripheral artery disease ICD 10 code is I73.9 Peripheral vascular disease, unspecified. This code is typically assigned when a provider documents “PAD” or “peripheral vascular disease” without identifying severity, anatomical location, laterality, or associated complications. While technically valid, I73.9 falls under the broader ICD 10 peripheral artery disease category and is considered non-specific. It is also one of the leading causes of vascular claim denials.
The World Health Organization ICD-10 classification guidance indicates that I73.9 should only be used when no additional clinical detail is available. In most clinical settings, more specificity exists but is not properly documented. When that happens, coders are prevented from selecting a more accurate ICD 10 code for peripheral arterial disease, increasing denial exposure.
In practice, payers and auditors expect assignment from the I70.x series, which reflects atherosclerosis of arteries of the extremities. These codes provide clinical detail regarding:
- Presence of intermittent claudication
- Ulceration or tissue loss
- Gangrene
- Laterality such as right, left, or bilateral
- Anatomical location including femoral, popliteal, or iliac arteries
When obstruction is clearly documented, coding may align more closely with classifications that support an ICD 10 code for peripheral arterial occlusive disease, rather than relying on a vague unspecified diagnosis.
The Centers for Medicare & Medicaid Services (CMS) consistently warns that unspecified circulatory system codes, such as I73.9 can trigger medical necessity denials for high-cost services including angioplasty, duplex ultrasound, atherectomy, and bypass surgery. Proper selection within the peripheral arterial disease ICD 10 framework ensures appropriate linkage between diagnosis and CPT procedures.
| ICD-10 Code | Description | When to Use | Compliance Impact |
|---|---|---|---|
| I73.9 | Peripheral vascular disease, unspecified | When provider only documents “PAD” without detail. | High denial risk. Payers may reject claims for imaging or revascularization. |
| I70.211 | Atherosclerosis of native arteries of extremities with intermittent claudication, right leg | For PAD patients with exertional leg pain (claudication). | Supports E/M visits, exercise therapy, and medication management. |
| I70.233 | Atherosclerosis of native arteries of extremities with ulceration, left leg | For PAD with non-healing wounds or ulcers. | Justifies wound care CPT 11042, 11043 and vascular procedures. |
| I70.261 | Atherosclerosis of native arteries of extremities with gangrene, right leg | For PAD with critical ischemia and tissue loss. | Supports bypass or amputation; strong medical necessity. |
| I70.8xx | Atherosclerosis of extremities with other complications | For less common but severe PAD complications. | Reinforces medical necessity for advanced imaging and interventions. |
Did You Know?
The Healthcare Financial Management Association (HFMA) reports that vascular claims coded with I73.9 have a 40% higher denial rate than those coded with I70.x series, due to “lack of specificity.”
Which ICD-10 Chapter Covers Peripheral Artery Disease ICD 10 Classifications?
PAD codes are located in Chapter 9: Diseases of the Circulatory System (I00-I99). This classification matters because payers use chapter-based coverage rules to decide whether vascular imaging and revascularization procedures are reimbursable.
According to CMS’s Medicare Coverage Database, vascular procedures such as angioplasty or bypass require precise I70.x codes, not I73.9 unspecified. Misclassification under “unspecified circulatory disorders” is a common denial trigger.
| CPT Code | Service Description | When Used in PAD Billing | Compliance Notes (with Sources) |
|---|---|---|---|
| 99213 / 99214 | Outpatient E/M visits | For evaluation of PAD symptoms, medication management, risk factor counseling. | Documentation must include claudication, rest pain, or wounds linked to I70.x or I73.9, according to CMS E/M Guidelines. |
| 93925 / 93926 | Duplex scan of lower extremity arteries | Ordered for diagnosis or monitoring PAD progression. | Medical necessity must reflect claudication or suspected ischemia, as noted by the American College of Radiology (ACR). |
| 37225 | Angioplasty, femoral/popliteal artery | Used in revascularization for symptomatic PAD. | Documentation must prove failure of medical therapy and imaging confirmation, consistent with CMS LCD for Lower Extremity Revascularization. |
| 35371 | Femoral-popliteal bypass graft | For severe occlusive disease or limb-threatening ischemia. | Must justify with documented ischemia, ulcers, or gangrene, consistent with Medicare LCD criteria. |
| 11042 / 11043 | Wound debridement | For PAD-related non-healing ulcers. | Ulcer diagnosis must be linked directly to a PAD ICD-10 code, as emphasized in AMA CPT guidance. |
Did You Know?
The American College of Cardiology (ACC) stresses that PAD is underdiagnosed and undertreated, and improper coding contributes to gaps in reimbursement for vascular procedures.
What Treatments Affect Billing Under Peripheral Artery Disease ICD 10 Guidelines?
Treatment for PAD ranges from lifestyle changes and medications to invasive revascularization. The National Heart, Lung, and Blood Institute (NHLBI) outlines therapy based on severity.
| Treatment Type | When Used | Billing Impact | Documentation Needed |
|---|---|---|---|
| Lifestyle & Medical Management | Early PAD, risk factor control (smoking cessation, statins, antihypertensives). | Outpatient visits (99213/99214) + medication management. | Must link PAD diagnosis to risk factor counseling. |
| Exercise Therapy | Supervised exercise for intermittent claudication. | CPT 93668 (cardiac rehab-like services in some payers). | Document exercise protocol and PAD symptoms. |
| Medications | Antiplatelets, statins, vasodilators. | Billed under E/M visits, some require prior authorization. | Document necessity (claudication, risk of CV events). |
| Angioplasty / Stenting | For severe occlusion in femoral/popliteal arteries. | CPT 37225, 37226, etc. | Must prove failure of conservative therapy and imaging findings. |
| Bypass Surgery | For critical limb ischemia, gangrene, non-healing ulcers. | CPT 35371 (fem-pop bypass). | Documentation of ulcer/gangrene required. |
| Wound Care / Debridement | For PAD-related ulcers. | CPT 11042, 11043. | Must link ulcers directly to PAD ICD-10 code. |
How Should Peripheral Artery Disease ICD 10 Documentation Be Structured to Avoid Denials?
Peripheral arterial disease generates significant payer scrutiny because it often leads to high-cost diagnostics and invasive interventions. Accurate selection of a peripheral artery disease ICD 10 classification alone does not guarantee payment.
Even when providers assign the correct ICD 10 code for peripheral arterial disease, whether I73.9 or a more specific I70.x code, claims may be denied if the documentation does not clearly establish severity, obstruction, and medical necessity.
The Centers for Medicare & Medicaid Services requires that PAD-related procedures, including duplex ultrasound 93925, angioplasty 37225, and bypass surgery 35371, be supported by detailed clinical documentation. When location, laterality, or complication status is missing, coding often defaults to an unspecified ICD 10 peripheral artery disease designation such as I73.9. This unspecified classification remains one of the most common vascular denial triggers.
The Office of Inspector General has also identified incomplete vascular documentation as a source of Medicare overpayments. Proper structure within the peripheral arterial disease ICD 10 framework is therefore critical for compliance and audit protection.
Below is a structured documentation model that reduces denial risk:
| Step | Action | Denial Risk if Skipped |
|---|---|---|
| Identify Type of PAD | Document atherosclerosis, claudication, ischemia. | Defaults to I73.9 unspecified. |
| Record Laterality & Location | Right vs left femoral, popliteal, or iliac artery. | Imaging or procedure denied. |
| Link to CPT Services | Pair I70.x/I73.9 with duplex scans, angioplasty, or wound care. | Claim denied for “not medically necessary.” |
| Prove Medical Necessity | Show failed conservative therapy before revascularization. | Angioplasty or bypass denied. |
| Capture Complications | Ulcers, gangrene, rest pain. | Wound care or bypass not reimbursed. |
| Submit with Supporting Evidence | Include imaging reports, wound photos, progress notes. | Delayed payment or audit recoupment. |
What Are the Compliance Risks When Using PAD ICD 10 Codes?
Peripheral arterial disease is one of the most heavily audited vascular conditions in the reimbursement landscape. Because PAD frequently results in high-cost diagnostics and invasive procedures, payers closely evaluate whether the selected PAD ICD 10 classification is clinically supported.
Overreliance on unspecified coding within the broader ICD 10 peripheral artery disease category creates both reimbursement instability and compliance exposure.
The Centers for Medicare & Medicaid Services identifies vascular disease among the top diagnoses flagged in audits due to improper coding and insufficient medical necessity documentation. The Office of Inspector General has similarly reported that Medicare overpayments are often tied to non-specific ICD-10 selections, incomplete complication reporting, or weak linkage between the ICD 10 code for PAD and corresponding CPT procedures.
Industry data cited by the Healthcare Financial Management Association indicates that vascular claims submitted with unspecified peripheral artery disease ICD 10 coding, such as I73.9, experience denial rates significantly higher than claims supported by specific I70.x atherosclerosis codes. These denials delay reimbursement and increase post-payment review risk.
Below is a compliance-focused breakdown of common PAD coding risks:
| Compliance Risk | Impact on Billing & Compliance | Real-World Example | Prevention Strategy |
|---|---|---|---|
| Overuse of I73.9 (unspecified PAD) | Triggers denials and payer audits. | Duplex scan billed with I73.9 denied as “non-specific.” | Use I70.x codes with claudication, ulceration, or gangrene whenever documented. |
| Failure to Document Laterality & Location | Imaging/procedure claims denied due to incomplete detail. | Angioplasty billed without noting right vs left leg. | Always capture vessel (femoral, iliac, popliteal) + laterality in notes. |
| Missing Complications (ulcer, gangrene) | Leads to underpayment or claim rejection. | Wound care billed without linking ulcer to PAD. | Add complication codes (I70.23x, I70.26x) when documented. |
| Incorrect ICD-10/CPT Linkage | Claim denied as “not medically necessary.” | Angioplasty CPT 37225 paired with I73.9 unspecified. | Link specific I70.x code with procedure to show necessity. |
| Weak Documentation of Medical Necessity | High-cost procedures flagged as routine. | Bypass surgery denied because no failed conservative therapy documented. | Document failed medication/exercise therapy before invasive procedures. |
| Ignoring Local Coverage Determinations (LCDs/NCDs) | Denial despite correct coding. | Medicare denies imaging billed without LCD-supported diagnosis. | Cross-check payer LCD/NCD before claim submission. |
Did You Know?
The American Heart Association (AHA) estimates that PAD patients cost the U.S. healthcare system $21 billion annually, making vascular claims a major target for payer scrutiny. Unspecified coding not only risks denials but also flags practices for utilization review and audits.
Why Should Providers Partner With ProMBS for Peripheral Artery Disease ICD 10 Billing?
Peripheral artery disease ICD 10 billing requires more than basic code selection. It demands precise diagnosis specificity, accurate CPT pairing, and airtight medical necessity documentation.
A minor mismatch between the ICD 10 code for peripheral arterial disease and procedures like angioplasty, duplex imaging, or wound care can trigger denials or audits.
At ProMBS, we strengthen your PAD ICD 10 billing through:
- Precise selection of the correct ICD 10 code for PAD based on severity, ischemia, ulceration, or gangrene
- Accurate ICD-10 and CPT linkage for imaging, revascularization, bypass, and wound care
- LCD and NCD verification before submission
- Proactive denial prevention and audit-ready documentation review
We do not simply submit claims. We position your peripheral artery disease ICD 10 claims to withstand payer scrutiny, reduce denials, and accelerate reimbursement.