Vomiting appears in medical records every day. Nausea appears just as often. They look simple. They are not.
In ICD-10-CM coding, Vomiting ICD 10 falls under Chapter 18. This chapter includes symptoms signs, and findings, not diseases. Payers review these claims closely.
Using the correct ICD 10 code for nausea and vomiting protects payment. It supports medical need. It keeps claims moving.
Coders face real choices. When does vomiting lead the claim? When does nausea with Vomiting ICD 10 follow another diagnosis? When should teams avoid R11.10?
This guide explains ICD 10 Nausea and Vomiting, the R11 code range, and Nausea and Vomiting in Pregnancy ICD 10 rules for 2025.
How Does Vomiting Happen in the Body?
Vomiting means the body forces stomach contents out. The brain controls this response. It reacts fast when the body senses danger. Triggers include infection, food toxins, pain, medication, and pregnancy.
These triggers often cause Nausea Vomiting ICD 10 symptoms together. The body follows a clear sequence during vomiting.
- A Trigger Appears
- The Brain Reacts
- Muscles Tighten
- The Stomach Moves Upward
- Vomiting Occurs
In coding, this matters. If nausea and vomiting share one cause, that cause leads. If no cause appears, vomiting and nausea ICD 10 codes stand alone. These symptoms fall under symptoms signs and abnormal findings that are not a diagnosis classifiable elsewhere.
How Does Vomiting ICD 10 Affect Coding Decisions?
Coding follows reason, not habit. If the provider documents a cause, that cause comes first. Vomiting becomes secondary.
Examples help.
- Gastroenteritis with vomiting → code gastroenteritis first.
- Medication reaction with nausea vomiting ICD 10 → code the reaction first.
- Pregnancy-related vomiting → use nausea and vomiting in pregnancy ICD 10, not R11.
When no cause appears, coders must choose the best ICD 10 Code for Vomiting or ICD 10 Code for Nausea Vomiting based on detail.
Known cause first. Symptom second. No cause? Symptom leads.
Which Vomiting ICD 10 Codes Should Coders Use?
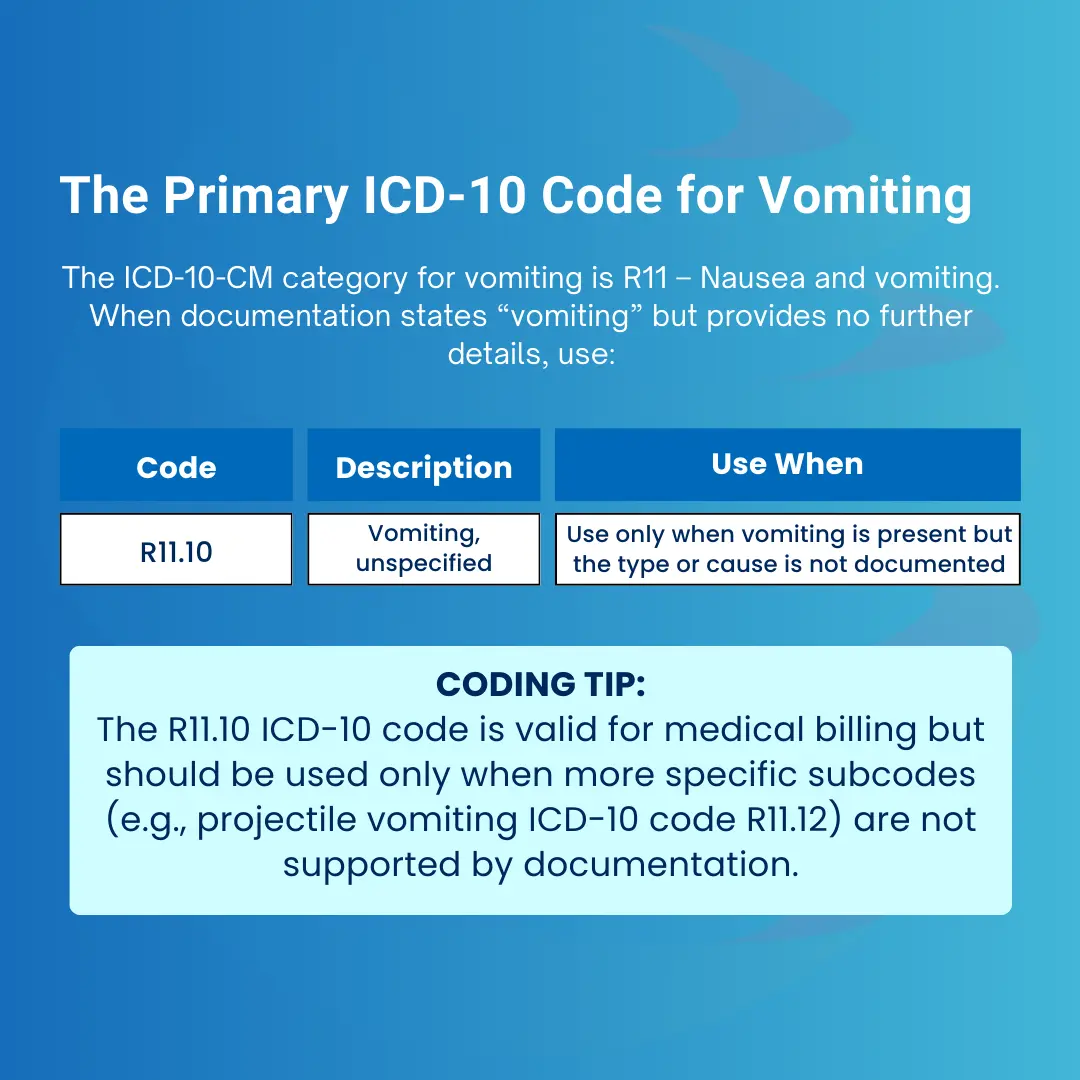
Choosing the right vomiting ICD 10 code depends on symptom detail. Details drive clean claims. The Vomiting ICD 10 category includes specific codes within categories R00–R94 consist of symptom-based diagnoses only.
- R11.0 – Nausea only
- R11.10 – Vomiting, unspecified
- R11.11 – Vomiting without nausea
- R11.12 – Projectile vomiting
- R11.13 – Vomiting of fecal matter
- R11.14 – Bilious vomiting
- R11.15 – Cyclical vomiting syndrome
- R11.2 – Nausea with vomiting
- O21.x – Excessive vomiting in pregnancy
These codes reflect symptoms signs abnormal results and abnormal clinical and laboratory findings. Follow type 2 excludes notes to avoid errors.
Related ICD-10 Codes for Vomiting
| ICD-10 Code | Description | Usage Criteria |
|---|---|---|
| R11.0 | Nausea | Only nausea is documented |
| R11.1 | Vomiting | Parent category (non-billable) – see subcodes below |
| R11.11 | Vomiting without nausea | Use when vomiting occurs without accompanying nausea |
| R11.12 | Projectile vomiting | Sudden, forceful expulsion (common in pyloric stenosis) |
| R11.13 | Vomiting of fecal matter | Often linked to intestinal obstruction |
| R11.14 | Bilious vomiting | Green/yellow vomit caused by bile reflux |
| R11.15 | Cyclical vomiting syndrome, not intractable | Recurrent vomiting episodes without clear cause |
| R11.2 | Nausea with vomiting, unspecified | Use when both symptoms are documented without more detail |
| O21.x | Excessive vomiting in pregnancy | Use for pregnancy-related cases (hyperemesis gravidarum) |
What Documentation Is Needed for Vomiting ICD 10?
Strong documentation supports the right ICD 10 Nausea Vomiting code.
Providers should answer clear questions. When did nausea and vomiting start? How often do symptoms occur? Does vomiting occur with or without nausea?
Type matters. Projectile vomiting changes the code. Bilious vomiting changes the code.
Context matters too.
- Abdominal Pain
- Fever
- Diarrhea
- Headache
Pregnancy status matters most. Nausea and vomiting in pregnancy ICD 10 follows a different rule set. If the cause stays otherwise specified unknown etiology, detail becomes critical.
Why Do Vomiting ICD 10 Claims Get Denied?
Denials follow patterns. The most common error involves overusing R11.10 when records support more specific codes. Another issue is sequencing. Vomiting should not lead when a condition explains it.
Pregnancy errors also cause denials. ICD 10 nausea and vomiting does not replace O21.x when pregnancy exists. Missing details create payer questions. These remain important problems in medical billing.
What Are Best Practices for Coding Vomiting ICD 10?
These rules work every time. Use the most specific Vomiting ICD 10 code available. Code the cause first when known. Apply Nausea with Vomiting ICD 10 only when both appear.
Reserve R11.10 for true lack of detail. Use Nausea and Vomiting in Pregnancy ICD 10 only for pregnant patients. Review claims before submission.
This approach aligns with international versions of ICD-10 and the 2026 edition of ICD-10-CM.
How Does Pro-MBS Prevent Vomiting ICD 10 Denials?
Pro-MBS handles ICD 10 Vomiting and ICD 10 Nausea and Vomiting with precision.
Our team reviews charts closely. We confirm documentation supports the chosen code. We check payer rules. We fix issues early.
Higher acceptance. Fewer denials. Faster payments.