Abdominal pain is one of the most clinically diverse and frequent complaints encountered in healthcare today. According to data from the Centers for Disease Control and Prevention (CDC), the number of non-injury emergency department (ED) visits where abdominal pain was the primary reason for the encounter has increased by nearly 32% in recent years.
Because it is a symptom that can point to anything from minor indigestion to life-threatening surgical emergencies, the Abdominal Pain ICD 10 codes (the R10 series) are some of the most vital tools in a medical coder’s arsenal.
For providers, the challenge lies in capturing the "complex symptom" with enough anatomical specificity to satisfy payer requirements while remaining compliant with ICD-10-CM guidelines. This guide provides an in-depth look at how to master the Abdominal Pain ICD 10 series, ensuring your documentation supports medical necessity and your claims remain "clean."
What is the Correct Abdominal Pain ICD 10 Series?
The ICD-10-CM (International Classification of Diseases, 10th Revision, Clinical Modification) uses the R10 series to categorize symptoms involving the abdomen and pelvis. Specifically, these codes are found in Chapter 18: "Symptoms, Signs, and Abnormal Clinical and Laboratory Findings, Not Elsewhere Classified."
By definition, an Abdominal Pain ICD 10 code is a "symptom" code. It is designed to be used when a definitive diagnosis has not yet been established by the provider. In the fast-paced environment of an Emergency Department or an Urgent Care center, the R10 series is the bridge between the patient's initial complaint and the final diagnostic outcome.
The Coding Hierarchy
Coding follows a logical progression from general to specific. The goal of every coder and clinician should be to reach the highest level of anatomical specificity supported by the clinical notes.
Which Code Matches the Anatomical Location of the Pain?
The Abdominal Pain ICD 10 codes are organized by location. Payer - including Medicare and private insurers - frequently deny claims that use "unspecified" codes if the clinical notes clearly describe a specific quadrant.
Table 1: Upper Abdominal Pain (R10.1 Series)
Upper abdominal symptoms often involve the liver, gallbladder, stomach, or pancreas.
| ICD-10 Code | Clinical Description | Common Clinical Associations |
|---|---|---|
| R10.10 | Upper abdominal pain, unspecified | General upper discomfort without a quadrant |
| R10.11 | Right upper quadrant (RUQ) pain | Cholecystitis, Hepatitis, Biliary colic |
| R10.12 | Left upper quadrant (LUQ) pain | Splenic infarct, Gastritis, Pancreatitis (tail) |
| R10.13 | Epigastric pain | GERD, PUD, Myocardial Infarction (referred) |
Table 2: Lower Abdominal and Pelvic Pain (R10.2 - R10.3 Series)
Lower abdominal pain is a common trigger for surgical consultations and specialized imaging.
| ICD-10 Code | Clinical Description | Common Clinical Associations |
|---|---|---|
| R10.2 | Pelvic and perineal pain | Ovarian cysts, Prostatitis, Endometriosis |
| R10.30 | Lower abdominal pain, unspecified | General lower discomfort |
| R10.31 | Right lower quadrant (RLQ) pain | Appendicitis, Crohn's disease, Cecal diverticulitis |
| R10.32 | Left lower quadrant (LLQ) pain | Diverticulitis, Ulcerative colitis, Constipation |
| R10.33 | Periumbilical pain | Early appendicitis, Small bowel obstruction |
Table 3: Generalized and Severe Pain
When pain is not localized or presents as a surgical emergency, these codes are utilized.
| ICD-10 Code | Clinical Description | Clinical Context |
|---|---|---|
| R10.0 | Acute abdomen | Severe, sudden onset; rigid abdomen; surgical emergency |
| R10.84 | Generalized abdominal pain | Diffuse pain throughout multiple quadrants |
| R10.9 | Unspecified abdominal pain | No location documented (Use as a last resort) |
When Should You Use an Abdominal Pain ICD 10 Code?
A common point of confusion in medical billing is determining when a symptom code is appropriate versus a definitive diagnosis code.
Use the R10 Series When:
- The Cause is Unknown: The patient presents with pain, but after the physical exam and initial workup, the physician is still unsure of the etiology.
- Awaiting Test Results: The patient is being discharged from the ED or clinic while waiting for outpatient imaging (like a CT or MRI) or laboratory results.
- Differential Diagnosis Only: If the physician lists "suspected," "questionable," or "rule out" conditions (e.g., "Rule out appendicitis"), the coder must code the symptom (Abdominal Pain ICD 10) rather than the suspected condition in the outpatient setting.
Do NOT Use the R10 Series When:
- A Diagnosis is Confirmed: If the provider determines the patient has acute cholecystitis, you must code the cholecystitis (0) instead of the pain.
- The Pain is an Integral Part of a Disease: If a patient has a known stomach ulcer (x), the abdominal pain is considered an inherent symptom of that condition and is not coded separately.
How Does Specificity Drive Revenue Cycle Management?
In the world of medical billing, the Abdominal Pain ICD 10 code you choose serves as the justification for every other service provided during that encounter. This is known as Medical Necessity.
Supporting Diagnostic Imaging
If a physician orders a CT scan of the abdomen and pelvis, the insurance company's automated system looks for a matching diagnosis code.
- If you use R10.9 (Unspecified), the payer may flag the claim, questioning why an expensive CT was necessary for vague pain.
- If you use R10.31 (Right lower quadrant pain), the medical necessity for a CT to check for appendicitis is clear and supported.
Avoiding "Unspecified" Denials
Many modern payer contracts include "Specific Coding" clauses. These allow the insurance company to deny or downcode a claim if an "unspecified" code is used when a more specific code was available in the medical record. By ensuring the Abdominal Pain ICD 10 code matches the physician's physical exam notes (e.g., "tenderness in the RLQ"), you protect the practice from avoidable revenue loss.
How Do You Apply Abdominal Pain ICD 10 Codes in Real Scenarios?
To understand the practical application of the Abdominal Pain ICD 10 series, let's look at two common clinical paths.
Case Study 1: The Epigastric Evaluation
Presentation:
A 52-year-old female presents with sharp pain in the upper-middle abdomen that worsens after eating.
Physician Note:
"Patient reports epigastric distress. Differential includes GERD vs. Peptic Ulcer Disease. Ordering an H. pylori breath test and starting Omeprazole."
Coding Choice:
Because the GERD and Ulcer are only "differential" (suspected), the coder must use R10.13 (Epigastric pain). This Abdominal Pain ICD 10 code correctly describes the patient's state at the time of the encounter.
Case Study 2: The Appendicitis Workup
Presentation:
A 19-year-old male presents with sudden, severe pain in the right lower quadrant with rebound tenderness.
Physician Note:
"Suspected acute appendicitis. Patient transferred to surgery."
Coding Choice:
In the initial ED encounter, the code is R10.31 (Right lower quadrant pain). However, once the surgeon performs the appendectomy and the pathology confirms the disease, the surgeon will bill using K35.80 (Unspecified acute appendicitis). The Abdominal Pain ICD 10 code served its purpose during the diagnostic phase.
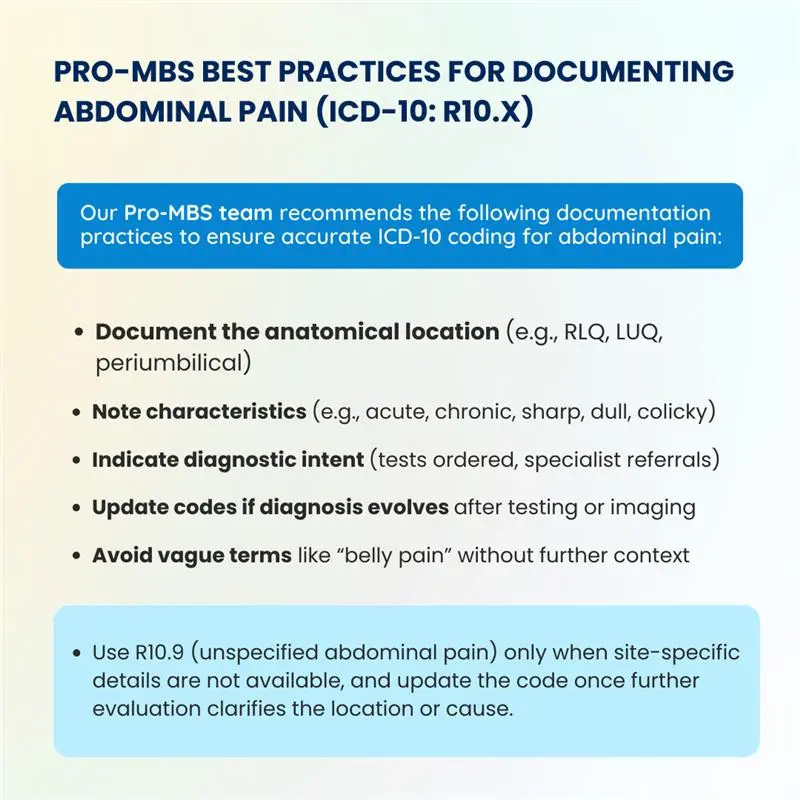
What are the Best Documentation Tips for Providers?
To help your coding team select the most accurate Abdominal Pain ICD 10 code, providers should focus on three specific elements in their charting:
- Localization:
Clearly state the quadrant (RUQ, LUQ, RLQ, LLQ) or region (Epigastric, Periumbilical, Pelvic). - Severity and Onset:
Distinguish between "generalized" pain and an "acute abdomen." This changes the code from R10.84 to R10.0, which reflects a higher level of clinical intensity. - Associated Symptoms:
Documenting tenderness, guarding, or rebound tenderness helps justify the use of more complex R10 codes and supports the level of Evaluation and Management (E/M) billed.
Why Choose Pro-MBS for Your Medical Coding Needs?
Navigating the nuances of the Abdominal Pain ICD 10 series requires a blend of clinical knowledge and coding expertise. At ProMBS, we specialize in helping practices move away from "unspecified" coding and toward high-specificity documentation.
Our Approach:
- Documentation Alignment: We review provider notes to ensure the physical exam findings match the assigned ICD-10 codes.
- Denial Management: We proactively identify claims where an Abdominal Pain ICD 10 code might be rejected due to lack of specificity and work with your team to correct them before submission.
- Real-time Guidance: We provide staff training on anatomical terminology to ensure that clinical language translates seamlessly into billing codes.
In an era where healthcare reimbursements are increasingly tied to the quality and specificity of documentation, mastering the Abdominal Pain ICD 10 R10 series is not optional—it is a financial and clinical necessity.
Frequently Asked Questions
Does a confirmed diagnosis replace an abdominal pain ICD 10 code?
A specific diagnosis always overrides a symptom code once the physician confirms the underlying cause. If testing reveals acute appendicitis or a stomach ulcer, you must report the definitive condition. Using an abdominal pain ICD 10 code alongside a confirmed diagnosis often leads to claim denials for redundant coding.
How does anatomical specificity affect reimbursement for abdominal pain?
Payers use anatomical specificity to determine the medical necessity of expensive diagnostic tests. Coding for right upper quadrant pain (R10.11) justifies a gallbladder ultrasound, whereas unspecified codes like R10.9 frequently trigger automated audits. Precise coding protects your revenue cycle by aligning the patient's symptoms with the services rendered.
When should providers use the acute abdomen code R10.0?
The R10.0 code applies specifically to severe, sudden-onset pain characterized by muscular rigidity or guarding. This code signals a potential surgical emergency to the payer, reflecting a higher level of clinical intensity. Use this only when the physical exam confirms "acute abdomen" findings, rather than general discomfort.
Can you bill abdominal pain ICD 10 codes for "rule out" conditions?
In outpatient settings, coders must report the patient's current symptoms rather than suspected or "rule out" diagnoses. If a physician suspects diverticulitis but awaits imaging results, you should submit the abdominal pain ICD 10 code for the specific quadrant. This ensures the claim remains accurate to the current stage of evaluation.
What documentation elements support the R10 series for medical necessity?
Effective documentation must pinpoint the exact quadrant and include associated findings like rebound tenderness or localized guarding. These clinical details validate the selection of specific R10 codes over generalized options. Clear localization in the provider’s note streamlines the billing process and provides a transparent audit trail for insurers.