Introduction
Pneumonia is a leading cause of morbidity and hospital admissions in the United States. According to the CDC, pneumonia results in roughly 2.2–2.5 million healthcare encounters per year, including about 1.2 million emergency department visits and ~1.1 million hospitalizations across all age groups. In 2011, pneumonia hospitalization costs reached $10.6 billion in direct medical expenses
Among the most frequently used codes is ICD-10 J18.9, representing "pneumonia, unspecified organism." It accounts for a large percentage of inpatient and outpatient claims where a causative agent is not yet identified.
But while the code may seem simple, misapplying it can lead to claim denials, delayed payments, compliance risks, and poor clinical documentation.
This guide will help you:
- Understand the correct use of J18.9
- Apply it in real-world billing scenarios
- Avoid common billing mistakes
- Improve documentation to support clean claims
What Is J18.9 ICD-10 Code?
The ICD-10 code J18.9 is used when pneumonia is diagnosed but no specific causative organism has been identified. It is commonly used during initial patient evaluation, before culture or lab results return.
Code Breakdown:
- J18: Pneumonia
- .9: Unspecified organism
Use J18.9 only when no bacterial, viral, fungal, or parasitic organism has been confirmed.
When to Use J18.9 in Clinical Practice
Outpatient Use Case:
A 47-year-old patient presents with fever, productive cough, and dyspnea. A chest X-ray confirms pneumonia, but no sputum or blood cultures are performed. Diagnosis is pneumonia, unspecified organism. J18.9 is appropriate.
Inpatient Use Case:
A 72-year-old is admitted with bilateral pneumonia. Cultures are pending, but treatment starts immediately. J18.9 is used initially. Upon confirmation of Streptococcus pneumoniae, the code is updated to J13.
Key Documentation Elements for J18.9
To assign J18.9 appropriately, the provider’s documentation must clearly support a diagnosis of pneumonia without identifying a causative organism. Payers and auditors require certain clinical details to validate the use of an “unspecified” code like J18.9. Here are the key documentation elements that justify this code:
Documentation Element | Why It Matters |
Diagnosis of pneumonia | Establishes the medical necessity for using a pneumonia-related ICD- 10 code |
Symptom description | Supports clinical severity and need for intervention (e.g., cough, fever, SOB) |
Imaging results (CXR/CT) | Provides objective evidence of pulmonary infection |
Culture or lab notes | Confirms whether an organism has or hasn't been identified |
Absence of specific pathogen | Justifies use of the "unspecified" J18.9 code when no organism is confirmed |
Always remember if culture results become available later in the hospital stay or follow-up, the diagnosis code should be updated to reflect the specific pathogen (e.g., J13 for Streptococcus pneumoniae). Accurate, timely documentation ensures compliance and prevents reimbursement issues.
Common Billing Mistakes and Fixes
Mistake 1: Using J18.9 When Organism is Known
Once lab results confirm an organism, update the code to reflect the specific diagnosis.
Correct Alternatives:
- J13 – Pneumonia due to Streptococcus pneumoniae
- J15.0–J15.9 – Bacterial pneumonias
- J12.9 – Viral pneumonia, unspecified
Mistake 2: No Clinical Justification
Do not assign J18.9 without documentation of pneumonia via imaging or clinical findings.
Mistake 3: Failure to Update During Inpatient Stay
Always revise the code if organism data is received during hospitalization.
COVID-19 and J18.9: When Not to Use It
J18.9 should never be used when COVID-19 is the confirmed cause of a patient’s pneumonia. Doing so results in miscoding and could lead to reimbursement issues or compliance violations.
COVID-19 has specific ICD-10 codes that must be used to accurately capture the diagnosis and related conditions:
Use Instead:
- 1 – Confirmed COVID-19 diagnosis (lab-confirmed SARS-CoV-2)
- 82 – Pneumonia due to COVID-19
These codes should be used in combination, where appropriate, to reflect both the underlying viral infection and the resulting pneumonia.
Using the correct COVID-19-related codes ensures accurate claims, better tracking of COVID-related complications, and full alignment with CDC and payer billing guidelines.
Quick Comparison Table: Pneumonia Coding by Etiology
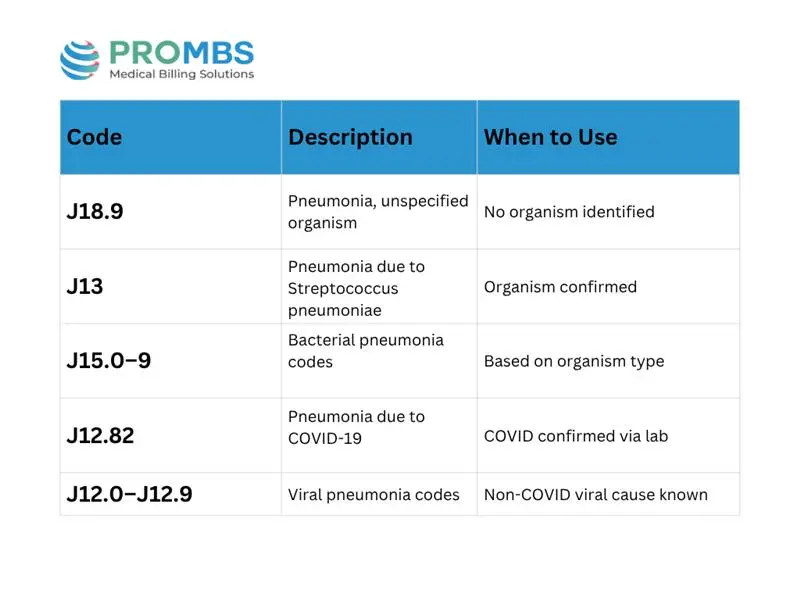
Tips for Clean Respiratory Billing
- Always document symptom onset, imaging, and treatment plan
- Track pending cultures in the EHR
- Update codes as labs return
- Confirm that the patient’s discharge summary reflects final diagnosis
- Stay updated with CMS ICD-10 revisions every October
How EHR Systems Improve Pneumonia Coding
Modern EHRs can support better respiratory billing by:
- Prompting documentation of imaging
- Flagging when labs are pending
- Reminding providers to update diagnoses before discharge
- Preventing duplicate coding or outdated entries
But remember: automation is a tool not a substitute for clinical and coding oversight.
Why Choose Pro-MBS for Pneumonia Billing
Getting respiratory billing right especially in high-volume cases like pneumonia requires expertise in both ICD-10 and payer policy.
Pro-MBS billing experts specialize in:
- Accurate coding for pneumonia across all care settings
- Real-time tracking of lab results and code adjustments
- Ensuring documentation aligns with payer requirements
- Reducing denials through detailed claim reviews
- Providing training for providers and admin staff
Whether you manage a small clinic or a large hospital group, our team ensures your pneumonia billing is clean, compliant, and efficient.
Conclusion
The J18.9 ICD-10 code is essential for accurately billing pneumonia cases where no specific organism has been identified. While it's commonly used in clinical settings, its apparent simplicity can be misleading without thorough documentation and timely updates, it can lead to denials, disrupt revenue flow, and attract payer scrutiny. To avoid these pitfalls, ensure that each claim is backed by clear clinical findings, imaging results, and documentation of culture status. Codes should be promptly revised as lab results return, and EHR systems should be used to track and update diagnoses efficiently. By using J18.9 with precision, providers can improve claim accuracy, maintain compliance, and deliver higher-quality care.