CPT Codes sit at the heart of neurosurgery billing. Strange how a few numbers can decide if a claim gets paid or denied. Yet here we are. One small slip can cost a practice thousands. Every neurosurgeon knows the weight of each cut, each stitch, and each step.
So why do so many groups still lose revenue to coding errors that could be prevented? What is the best way to safeguard each claim before it leaves the door?
Clean coding is not only smart. It is survival. Neurosurgery sits under sharp payer review because the RVUs are high and the stakes are higher. CMS, AMA, and major payers like UnitedHealthcare look at these codes with care.
They expect perfect alignment between the note and the claim. Miss one detail and the denial hits fast. This guide breaks down the codes that matter most and the signs that show when a claim is ready to stand on its own.
Quick Summary: Key CPT Codes for Neurosurgery
Here is a fast list of the most used CPT Codes in neurosurgery. Each code shows a path. Each path tells the story of the work done and the claim that must follow.
Craniotomy and Craniectomy Codes
61304–61548. These codes mark the cuts that open the skull. They guide access, ease pressure, and clear a way to deeper work.
Spinal Decompression Codes
63030, 63047, 63048. These codes tell when a disc is freed or when a nerve finds space to breathe again.
Laminectomy and Laminotomy Codes
63001–63048. The choice shifts with each level and each move the surgeon makes.
Fusion and Instrumentation Codes
22612, 22842, 22845. These codes show when the spine is held steady with hardware built to last.
Why Do CPT Codes Matter in Neurosurgery Billing?
Why do CPT codes carry so much weight in neurosurgery? Because the work is intense. Each case involves risk. Each step has purpose. And each part of the surgery ties back to a code that must tell the story with exact detail.
High RVUs bring closer review by CMS and commercial payers. They want proof the service was needed. They want proof it was done. They want proof the level count is right.
Incorrect CPT codes can cause denials that choke revenue flow. Some practices wait weeks for payment that never comes. Many ask the same question. How did this claim fail when the surgery was clear?
The answer often sits inside a missing add-on code, unclear steps, or a bundled service the coder did not see. Clean claims matter because neurosurgical cases are complex and long. The coding must show that same care.
What Are the Core CPT Codes Used in Neurosurgery?
When you think of daily neurosurgical billing, these codes often come to mind first. They form the base of most routine claims.
They also help coders match the surgeon’s words to the correct intent. What is the best way to understand which codes belong to which service? Start with the common groups.
| Procedure Type | Codes | Notes |
|---|---|---|
| Craniotomy and Craniectomy | 61304 to 61548 | Used for access, decompression, and major cranial work. |
| Spinal Decompression | 63030, 63047, 63048 | Used for disc issues or nerve root relief. |
| Laminectomy and Laminotomy | 63001 to 63048 range | Code choice depends on the level and method used. |
| Fusion and Instrumentation | 22612, 22842, 22845 | Covers arthrodesis and hardware placement. |
These codes shape the claim. They tell the payer what was done and why. They also show the level of skill the surgeon needed for the case.
How Should CPT Codes Be Applied in Spine Procedures?
Spine billing feels like a world of its own. So many levels. So many steps. So many choices. What is the best way to know if a case needs decompression, fusion, or both? Look at the intent of the surgery. Look at the note. Look at the outcome.
Decompression vs Fusion Codes
If imaging does not support surgical need, payers deny without pause. They want proof in black and white, not hope or habit. A missing film note turns a clean case into a dead claim.
Why risk that when Neurosurgery Billing Services can turn a single clear line into armor that shields thousands? One detail, caught in time, can stop a denial long before the payer ever draws its blade.
Common Spine Coding Mistakes
Wrong level counting is one of the top errors seen by UnitedHealthcare audits. Another common mistake is skipping add-on codes that show extra work. When claims do not match the note well, the payer assumes something is missing and holds payment.
Add On Instrumentation Codes
Codes like +22853 or +22859 show cage placement or extra steps. These codes build on base fusion procedures. They help the payer see the true scope of the surgery.
How Do CPT Codes Work in Minimally Invasive Neurosurgery?
Endoscopic Decompression Codes
Codes 63020 and 62162 apply when an endoscope guides access or decompression. These cases must state scope use with clarity.
MIS Fusion Techniques
Stereotactic Radiosurgery Codes
Codes 61796 to 61799 apply to SRS. Code choice depends on the number of targets and the plan complexity. CMS wants strong notes for these services since they hold high value.
What Documentation Prevents CPT Code Denials?
Documentation is the shield that protects revenue. What is the best way to prevent denials? Make the note impossible to doubt.
Every payer, including CMS, AMA, and UnitedHealthcare, expects clear language that shows exactly what the surgeon did.
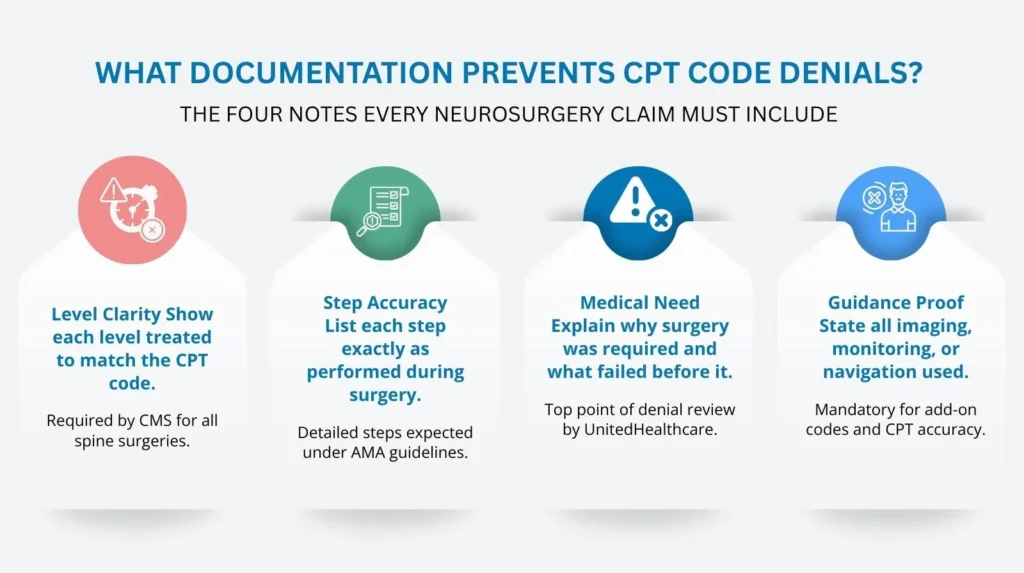
Key documentation must include:
- Level-by-level detail for spine work
- Complete steps for each part of the surgery
- Proof of medical need
- Notes on imaging, monitoring, and navigation
Top denial reasons include:
- Missing operative details
- Wrong level counts
- Missed add-on codes
- Mutually exclusive codes used by mistake
When a claim shows strong detail, the payer has fewer reasons to deny it. The claim stands firm.
How Can a Partner Improve Neurosurgery Billing?
Neurosurgery billing deserves a team that understands each risk, each rule, and each payer demand. Pro-MBS brings coders who know how neurosurgery works behind the scenes.
They follow AMA and CMS rules with care. They check level counts. They verify add-on codes. They build clean claims that move fast through payer review.
If you want stronger revenue, sharper claims, and fewer denials, a skilled partner can make that change real. Schedule your free consultation today.
| Common Neurosurgery Denial Reason | How Smart Systems Prevent It |
|---|---|
| Missing prior auth | Automated checks sweep the path early, catching missing approvals before the first cut. No surprises. No ambush. |
| Incorrect global period handling | Alerts rise like sentries, guiding teams toward the right moment to bill. Timing becomes a shield, not a trap. |
| Diagnosis mismatch | Code crosswalks lock CPT and ICD-10 pairs together with precision. No gaps. No fractures for payers to exploit. |
| Implant billing errors | Implant tracking keeps every unit and cost tight and clear. Nothing slips through the cracks. Nothing invites attack. |
| Missing op report details | Prompts pull rich details from the surgeon’s memory before they fade. Each note becomes armor against denial. |
| Duplicate submissions | System checks stand guard, blocking repeat claims before they wander into payer fire. Clean. Controlled. Certain. |
| LCD and NCD conflicts | Payer rules flare warnings early, long before the claim leaves your hands. Conflicts die before they can strike. |
Neurosurgery practices feel financial pressure more than most fields. Why does cash flow swing so wildly here? Because each case carries high value.
A single denial delays thousands. AR days stretch beyond forty-five. Payment posting slows down. Appeals stack higher each week. Weak reports hide true performance.
Smart systems steady the storm. They predict high-risk claims early. They highlight trends. They support clean follow-ups with automated tasks.
These tools help practices see where money stalls. How to mend the wound before it cuts deeper. Neurosurgery Billing Services turn that insight into action that shields the bottom line.
What Does a Smart Neurosurgery Workflow Look Like Today?
What does a modern system look like when built for neurosurgery services? It delivers clear steps and fast checks that guide teams through complex rules.
It automates prior auth. It scrubs claims with AI. It checks CPT and ICD-10 codes against payer rules. It tracks implant cost with accuracy.
It warns teams when global periods block billing. It gives surgeons dashboards that reveal revenue status in real time. It keeps every small detail aligned with expectations from AMA and CMS authorities.
Why Partner with Pro-MBS for Neurosurgery Billing Services?
Neurosurgeons need a partner who knows this world. Pro-MBS brings sharp coding skill and strong denial defense.
We watch payer rules. We support teams with clear templates and smart tools. We keep AR tight and claims moving. We help surgeons see revenue risk before it grows.
When you want a billing partner who understands every cut, stitch, and code, our team stands ready. Schedule your free consultation today.
Frequently Asked Questions
How do Neurosurgery Billing Services reduce denials in complex surgical claims?
Neurosurgery Billing Services cut denials by catching weak spots before payers strike. They track every step across neurosurgery services, from imaging to implants.
Smart tools read patterns and spot gaps that human eyes miss. Claims move cleaner, faster, and with fewer wounds. Want a team that stops trouble before it lands? Pro-MBS can lead that charge.
Why are documentation mistakes so costly in neurosurgery services?
In neurosurgery, one missing detail can shatter the entire claim. Payers study every line with cold precision. Neurosurgery Billing Services tighten each note so no gap becomes a weapon.
Stronger documentation means stronger payment defense. When every word matters, you need a partner who guards each page. Pro-MBS stands ready.
What makes neurosurgery coding more complex than other specialties?
Neurosurgery coding mirrors the surgeon’s blade. Every choice must match the exact work done. Neurosurgery Billing Services track each approach, level, implant, and add-on with disciplined accuracy.
Neurosurgery services leave no room for guesswork, and coding errors cut deep. Want precision without fear of denial? Pro-MBS delivers it.
How do smarter systems help shorten AR days for neurosurgery practices?
Smart tools hunt for errors long before a claim reaches a payer’s gate. They catch missing auths, mismatched codes, and timing traps that slow AR.
Neurosurgery Billing Services use these systems to push claims forward with clean momentum. Neurosurgery services rely on speed and clarity to protect cash flow. Ready to cut AR delays? Pro-MBS can make it happen.
Why do neurosurgery services often break traditional billing workflows?
Neurosurgery moves through many stages, and each stage tests weak workflows. ER to imaging. OR to post-op. Every step demands its own rules. Neurosurgery Billing Services link this chain so nothing slips into chaos.
When workflows fail, claims fall apart fast. For structure that never cracks, Pro-MBS brings the discipline you need.
How can Neurosurgery Billing Services improve financial stability for surgeons?
Unstable cash flow haunts neurosurgery more than any other field. High-value cases mean high-value losses when claims fall.
Neurosurgery Billing Services steady that storm by predicting risk. guarding documentation and clearing denials early. Strong revenue comes from strong systems. Want the certainty your practice deserves? Pro-MBS is the shield you need.
What does a modern billing workflow look like for neurosurgery services?
A modern workflow is fast, sharp, and unforgiving of errors. AI scrubs claims. Systems track implants. Alerts guard global periods.
Neurosurgery Billing Services unite all these parts, giving surgeons a clear view of revenue with no shadows. Neurosurgery services thrive when nothing is left to chance. Want a workflow built for real precision? Pro-MBS is your path forward.