According to CMS, In 2024, Medicare reported $31.7 billion in improper payments, much of it linked to coding and documentation errors, underscoring why physicians need a solid grasp of billing fundamentals
Medical billing is the process of preparing, submitting, and tracking healthcare claims to insurance payers so providers are reimbursed for the care they deliver. According to the Centers for Medicare & Medicaid Services, this involves collecting patient and insurance details, generating accurate claims based on documented services, and following up on payments or denials to keep the revenue cycle flowing smoothly.
Medical coding translates clinical documentation such as diagnoses, procedures, and treatments into standardized code sets like ICD-10-CM, CPT®, and HCPCS. The World Health Organization’s ICD-10 classification, along with other coding standards, ensures that every service is recorded in a universally recognized format, supporting medical necessity, meeting payer compliance requirements, and enabling accurate and timely reimbursement.
Understanding medical billing basics for physicians is particularly important because it bridges the gap between clinical care and reimbursement.
Why Medical Billing and Coding Matter in 2025?
Medical billing and coding are the foundation of healthcare revenue cycle management (RCM). Every time a patient visits a doctor, undergoes a diagnostic test, or receives a procedure, the serdenivice must be translated into standardized codes. These codes are then processed through efficient Medical Billing Workflows to ensure timely payment.
In 2025, medical billing and coding sit at the center of healthcare revenue performance. Every claim that leaves a practice is judged on two things: medical necessity and coding accuracy. According to MGMA, practices that consistently maintain a clean-claim rate above 95% see reimbursement arrive an average of 10–14 days faster than those with lower rates.
Accurate coding not only supports payment but also protects practices against payer audits and compliance penalties, which CMS reports cost the industry billions in improper payments each year. For physicians, understanding these workflows is no longer optional. It’s a frontline skill for safeguarding revenue and keeping administrative burdens low.
When implemented effectively, strong medical billing workflows and proactive denial-management strategies help healthcare providers maintain financial stability and focus more on patient care. Understanding this process empowers providers to streamline operations, strengthen revenue performance, and explore rewarding career opportunities in the growing field of Medical Billing and Coding.
For physicians, mastering medical billing basics helps ensure smoother workflows, timely payments, and compliance with payer regulations.
The Medical Billing Process: Step by Step
Medical Billing and Coding form the backbone of healthcare revenue management. This process connects the clinical services patients receive with the financial operations that keep healthcare practices running.
Here’s how the Medical Billing Process unfolds from the first patient visit to final payment.
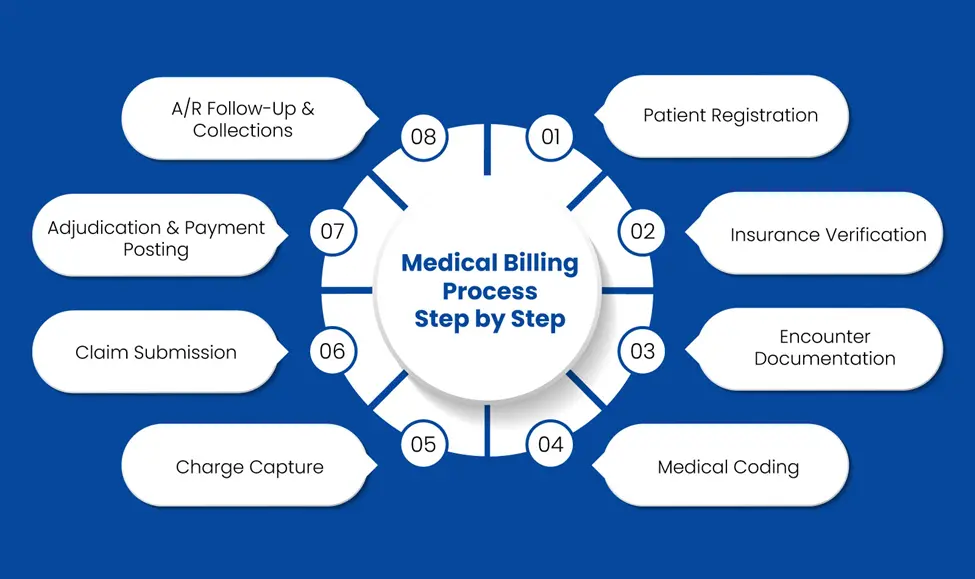
Step 1: Patient Registration
Patient registration is the first and most critical step in the Medical Billing Process.
Front-desk staff collect the patient’s demographic details such as name, date of birth, address, and contact information along with insurance data like the payer’s name, policy number, and group ID.
Accurate registration sets the tone for the rest of the medical billing and coding workflow. Even minor errors, such as a misspelled name, wrong date of birth, or outdated insurance details, can lead to denied or delayed claims. Verifying eligibility and recording details correctly at the start helps prevent costly rework later.
Step 2: Insurance Verification
Before a provider delivers care, the billing team verifies the patient’s insurance coverage.
This includes confirming the policy’s active status, benefit limits, copay amounts, deductibles, and any prior-authorization requirements.
Insurance verification helps providers understand the patient’s financial responsibility upfront and prevents revenue loss caused by unpaid claims. Without this step, services might be provided that the payer refuses to cover, leading to denials and payment delays.
Step 3: Encounter Documentation
During the visit, the provider documents all relevant clinical information in the medical record, including the chief complaint, diagnoses, procedures performed, treatments given, lab orders, and follow-up plans.
Accurate documentation is both a clinical and financial requirement. It establishes medical necessity, which payers use to approve or deny reimbursement. If notes are incomplete or vague, coders may be forced to use unspecified codes, raising the risk of denials and compliance issues.
Step 4: Medical Coding
Once documentation is complete, certified coders translate the provider’s notes into standardized billing codes used by payers:
- ICD-10-CM codes for diagnoses
- CPT® codes for physician services and procedures
- HCPCS Level II codes for supplies, drugs, and equipment
Correct coding ensures the claim reflects both the clinical picture and payer rules. Coding errors can lead to denials, compliance issues, or audits. Quality coding services reduce errors and improve claim acceptance rates.
Step 5: Charge Capture
In this step, all coded services from the encounter are entered into the billing system as billable charges. Charge capture ensures that every service provided, no matter how small, is recorded and billed appropriately.
If a service is missed, the provider delivers care without reimbursement, resulting in revenue loss. Effective charge capture links clinical work to financial outcomes.
Step 6: Claim Submission
After charges are captured, the billing team prepares and submits claims electronically through a clearinghouse or directly to the insurance payer.
Submitting a clean claim, accurate, complete, and compliant on the first attempt, shortens payment cycles and minimizes rejections. Timely submission also avoids losses due to missed filing deadlines.
Step 7: Adjudication & Payment Posting
Once the claim is submitted, the payer reviews it for accuracy and medical necessity in a process called adjudication. The claim may be approved (paid in full or partially), denied, or returned for additional information.
After adjudication, the provider receives payment along with an Explanation of Benefits (EOB) or Electronic Remittance Advice (ERA) showing how the claim was processed. The billing team posts the payment to the patient’s account and reconciles it with the original charges.
Step 8: A/R Follow-Up & Collections
The final stage of the Medical Billing and Coding process involves monitoring unpaid or underpaid claims, addressing denials, and following up with payers or patients for outstanding balances.
An efficient Accounts Receivable (A/R) follow-up process ensures cash flow remains stable and no claims are left unresolved. Poor A/R follow-up often leads to revenue leakage and increased write-offs.
What Are the Career Opportunities in Medical Billing and Coding?
A strong and skilled Medical Billing and Coding workforce is essential for both healthcare providers and billing service companies. For physicians in private practice, understanding medical billing basics can improve oversight of their revenue cycle and enhance collaboration with billing teams.
These professionals ensure that claims are submitted accurately, reimbursements are timely, and compliance is maintained.
Medical Billing vs Coding – What’s the Difference?
| Aspect | Medical Coding | Medical Billing |
|---|---|---|
| Role | Reviews clinical documentation and assigns standardized codes. | Uses assigned codes to prepare, submit, and track claims. |
| Key Code Sets | ICD-10-CM, CPT®, HCPCS | Uses codes from coders to create claims for payers. |
| Main Focus | Accuracy of diagnosis and procedure coding. | Ensuring claims are processed and payments collected. |
| Goal | Translate medical services into universal codes. | Secure timely and correct reimbursement. |
| Skills Needed | Knowledge of medical terminology, coding guidelines. | Knowledge of claim forms, payer policies, and follow-ups. |
Key Roles in Medical Billing and Coding
Medical coders translate clinical documentation into standardized ICD-10-CM, CPT®, and HCPCS Level II codes, ensuring compliance with payer and regulatory guidelines.
Medical billers use these coded records to generate, submit, and reconcile claims, monitor adjudication, and manage A/R workflows for optimal reimbursement.
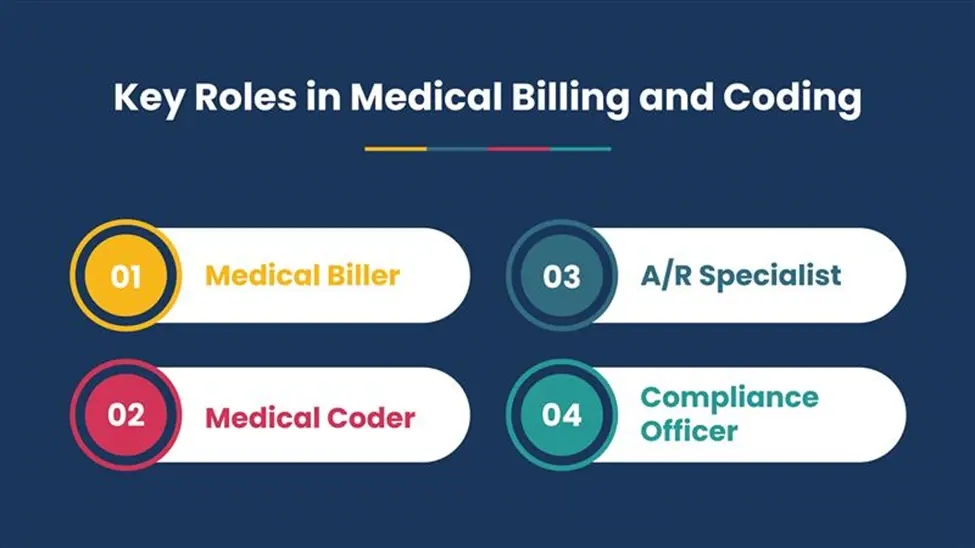
Medical Biller: A Medical Biller manages every stage of the Medical Billing Process, from claim preparation to follow-ups and denial resolution.
Medical Coder: A Medical Coder assigns precise ICD-10, CPT®, and HCPCS codes that convert clinical documentation into billable services. Accurate Medical Coding is the foundation for clean claims.
A/R Specialist: An A/R Specialist focuses on accounts receivable, pursuing unpaid claims and optimizing cash flow within the Medical Billing Cycle.
Compliance Officer: A Compliance Officer oversees regulations, payer rules, and internal audits to keep Medical Billing and Coding Operations compliant and audit-ready.
Key Skills for Medical Billing and Coding Professionals
Professionals in Medical Billing and Coding need:
- In-depth knowledge of coding guidelines and updates for ICD-10 and CPT®
- Familiarity with payer-specific policies and reimbursement procedures
- Attention to documentation quality to support clean claims and prevent denials
- Strong communication skills to collaborate with providers, payers, and revenue cycle teams
Salary Outlook for Medical Billing and Coding Careers
According to AAPC’s 2024 data, AAPC members earn an average of $65,401 annually, with those holding multiple credentials often earning more. In practice, healthcare organizations and B2B billing firms prize certified medical billing and coding talent because it contributes to higher first-pass claim acceptance rates, fewer denials, and smoother overall revenue cycle operations.
In-House vs. Outsourced Billing for Providers
Healthcare providers must choose between managing billing themselves or partnering with experts to improve efficiency and revenue.
| Aspect | In-House Billing | Outsourced Billing |
|---|---|---|
| Definition | Keeps the entire medical billing and coding process within the healthcare organization. | Partners with a specialized billing service provider. |
| Control | Offers more direct oversight of staff, processes, and data. | Relies on an external partner, with less hands-on control. |
| Staff & Resources | Requires hiring, training, and managing dedicated billing staff and maintaining technology. | Uses the expertise, tools, and infrastructure of the service provider. |
| Efficiency & Expertise | Dependent on internal team’s skill and capacity; may face productivity or knowledge gaps. | Leverages specialized experts and proven workflows to optimize billing operations. |
| Denial Management | May struggle with high denial rates due to limited resources or outdated processes. | Often reduces denials by applying advanced analytics, compliance standards, and payer-specific knowledge. |
| Cash Flow Impact | Can face delays due to staffing shortages, system errors, or limited scalability. | Generally improves cash flow through streamlined processes and faster claim turnaround. |
Healthcare organizations must decide whether to keep Medical Billing in-house or outsource it to a trusted partner.
How to Choose the Right Medical Billing Partner?
For B2B healthcare providers and billing firms, the right billing partner can mean the difference between steady revenue and cash flow problems. Predictable revenue comes from clean claims, minimal denials, and timely reimbursements, while poor processes lead to delays, rework, and financial strain.
A reliable partner brings strong workflows, coding accuracy, and compliance expertise. By integrating with EHR systems and proactively managing denials, they accelerate reimbursements, reduce audit risk, and support long-term financial stability.
Partner with Pro-MBS for Smarter, Compliance-Driven Medical Billing
At Pro-MBS, we deliver end-to-end medical billing and coding solutions designed for the unique challenges of healthcare providers and billing firms. Our certified specialists work as an extension of your team, ensuring accurate code selection, precise charge capture, and full alignment with payer policies and compliance standards to minimize delays, reduce denials, and keep your cash flow strong.
We go beyond routine claim processing. By combining advanced billing protocols, streamlined workflows, and proactive denial-management strategies, we help you optimize the entire revenue cycle, from charge entry to final payment.
Our consultative approach focuses on documentation integrity, real-time error resolution, and ongoing process improvement, empowering you to achieve higher first-pass acceptance rates, faster reimbursements, and sustainable financial growth, all while allowing your clinical team to stay focused on delivering exceptional patient care.
FAQs
Can I teach myself medical coding and billing?
Yes, you can, but it’s challenging. Medical coding and billing require extensive knowledge of ICD-10-CM, CPT, payer-specific edits, and compliance rules. Most providers prefer to rely on experienced professionals to avoid errors that can lead to denied claims or audits.
What is the golden rule in medical billing and coding?
This principle ensures that every code assigned in a claim is fully supported by the provider’s clinical documentation. It protects against upcoding or under coding, reduces claim denials, and keeps the billing process compliant with payer and CMS regulations.
What is the hardest thing about medical billing and coding?
The hardest part of medical billing and coding is keeping up with constant regulatory changes while ensuring every claim is accurate and compliant. It requires precise interpretation of clinical documentation, adherence to payer rules, and ongoing updates to avoid denials or audits.
What is the rule of 9 in medical coding?
The Rule of Nines in medical coding is used to estimate the total body surface area (TBSA) affected by burns for accurate ICD-10-CM coding. It divides the body into regions, each representing 9% or a multiple of 9% of TBSA, such as head and neck (9%), each arm (9%), each leg (18%), and anterior or posterior trunk (18%). This calculation supports proper documentation, coding, and treatment planning for burn cases.
What are the basics of medical coding for beginners?
Medical coding involves converting clinical documentation like diagnoses, treatments, and procedures into standardized alphanumeric codes for claims and compliance. The key code sets are ICD-10-CM for diagnoses, CPT for procedures, and HCPCS Level II for services and supplies. Beginners should focus on understanding anatomy, medical terminology, and payer guidelines to ensure accuracy and compliance.