Healthcare providers across the U.S. are increasingly evaluating whether to keep billing in-house or partner with Outsourced Medical Billing companies. With rising labor costs, compliance challenges, and payer scrutiny, the decision directly impacts revenue cycle management (RCM), denial rates, and overall profitability.
This guide provides a comprehensive analysis of Outsourced Medical Billing, its advantages, drawbacks, cost implications, and the strategic factors providers must consider in 2025.
Why Outsourced Medical Billing Matters in 2025?
In today’s healthcare landscape, the ability to manage revenue efficiently is as important as providing quality patient care. Outsourced Medical Billing has emerged as a strategic solution for providers facing staffing shortages, high overhead costs, and rising payer scrutiny. According to recent industry reports, over 40% of practices in the U.S. now outsource some or all of their billing functions, a trend expected to grow as reimbursement rules become more complex.
The outsourcing decision directly impacts Revenue Cycle Management (RCM) by influencing claim accuracy, denial prevention, and compliance readiness. For practices navigating value-based care, telehealth expansion, and tighter CMS regulations, outsourcing is no longer just about cutting costs, it’s about safeguarding financial stability and ensuring scalability.
What Is Outsourced Medical Billing?
Outsourced Medical Billing is the process of delegating billing, coding, and RCM operations to a specialized third-party vendor instead of maintaining an in-house team. Outsourced partners handle:
- Claim submission and payment posting
- Coding accuracy and compliance audits
- AR follow-up and denial management
- Eligibility verification and prior authorizations
- Reporting, analytics, and compliance documentation
While historically associated with small practices, Outsourced Medical Billing Services are now widely used by large physician groups, hospitals, and specialty clinics seeking scalability, compliance, and efficiency.
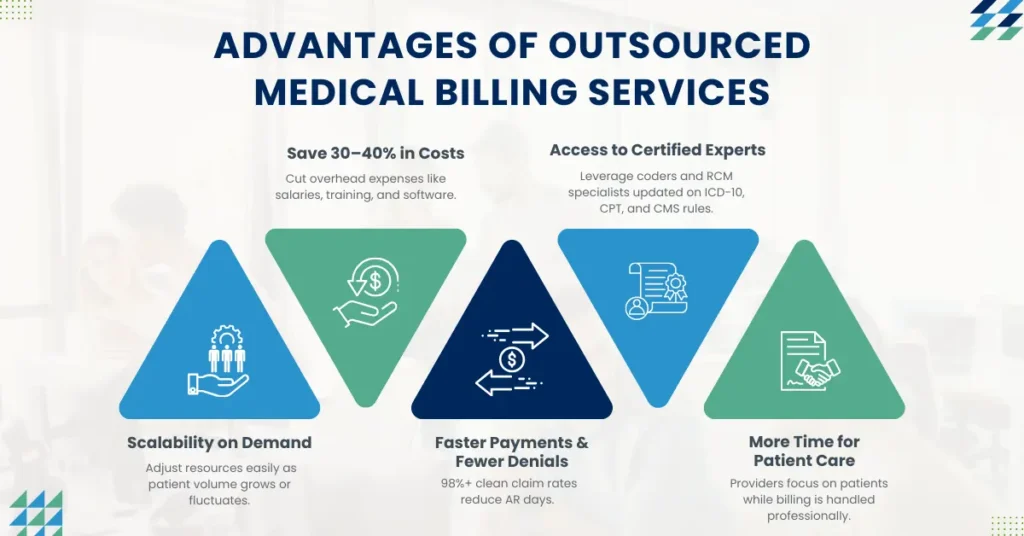
What Are the Advantages of Outsourced Medical Billing?
Outsourced Medical Billing offers several measurable benefits that impact both financial performance and operational efficiency. Below is a detailed breakdown of the advantages providers typically experience when choosing Outsourced Medical Billing Services over in-house billing models.
1. Cost Savings
One of the primary drivers for Outsourced Medical Billing is the significant reduction in overhead expenses. In-house billing requires staffing salaries, employee benefits, ongoing training, EHR and billing software licenses, clearinghouse fees, and IT infrastructure. By partnering with a medical billing outsourcing company, providers eliminate these fixed costs and replace them with a predictable service fee.
An Outsourced Medical Billing vs in-house billing comparison shows that practices can save 30–40% in operational expenses by outsourcing. This is especially impactful for small to mid-sized practices where margins are tighter. Additionally, outsourcing reduces the financial risks tied to staff turnover and costly billing errors, making it a sustainable cost-containment strategy.
2. Specialized Expertise
Outsourced Medical Billing companies employ certified medical coders, denial management experts, and RCM (Revenue Cycle Management) specialists who are trained across multiple specialties. This level of expertise is difficult and expensive for most practices to maintain in-house.
By outsourcing, providers gain access to professionals who are constantly updated on payer policy changes, ICD-10 and CPT coding updates, and compliance regulations such as HIPAA and CMS guidelines. This expertise translates into fewer denied claims, faster reimbursement, and compliance-readiness. For practices in specialties with complex coding such as oncology, orthopedics, or cardiology, this expertise is invaluable.
3. Scalability
As practices grow or experience seasonal fluctuations in patient volume, managing billing in-house can become a challenge. Hiring and training additional staff to meet higher demand requires time and resources, and layoffs during slow periods can be disruptive.
Outsourced Medical Billing Services provide built-in scalability. Outsourcing partners can quickly adjust staffing and resources to match claim volume, ensuring that practices maintain consistent claim submission timelines and revenue flow. This flexibility makes outsourcing a practical solution for practices anticipating growth, mergers, or expansion into new specialties.
4. Improved Revenue Cycle Performance
One of the most compelling benefits of Outsourced Medical Billing is their direct impact on revenue cycle performance. Many vendors report 98%+ clean claim rates, meaning the vast majority of claims are accepted on the first submission without errors. This translates into fewer denials, reduced AR days, and faster reimbursements.
For providers, this improvement in the revenue cycle means stronger and more predictable cash flow. Denial reduction alone can increase collections by 15–25% compared to in-house billing teams that may lack denial prevention workflows. In short, outsourcing medical billing reduces denials, accelerates payments, and ensures consistent revenue integrity.
5. Focus on Patient Care
Perhaps the most overlooked but equally important advantage of medical billing outsourcing is that it allows providers to dedicate more time to patient care. In-house billing requires constant oversight of claim submission, AR follow-up, and compliance tracking, which can distract staff and physicians from direct patient engagement.
By transferring billing responsibilities to an Outsourced Medical Billing provider, practices free up valuable internal resources. Physicians and staff can focus on improving patient satisfaction, growing their practice, and delivering higher-quality care. In today’s competitive healthcare landscape, this improved focus on patient experience often translates into stronger patient retention and practice growth.
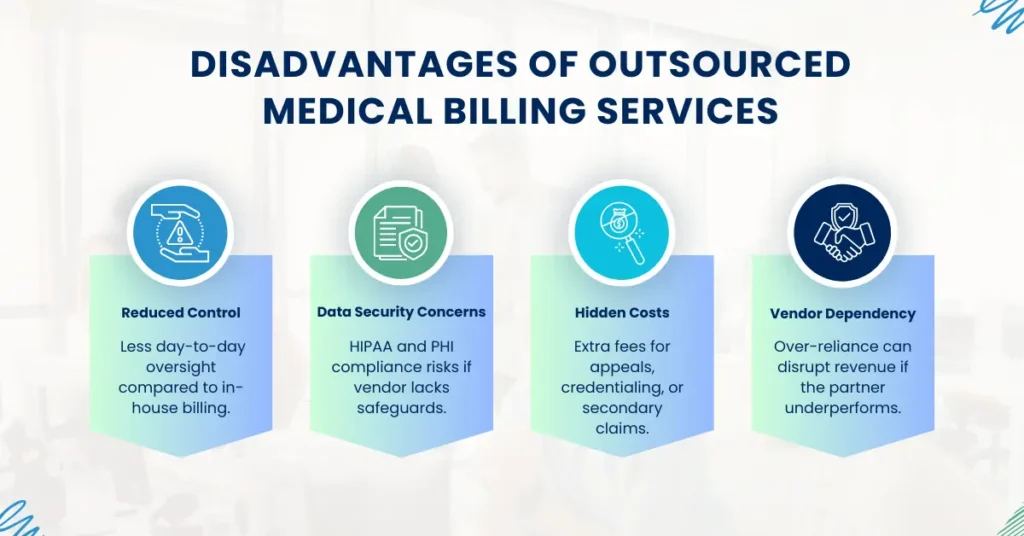
What Are the Disadvantages of Outsourced Medical Billing?
1. Loss of Direct Control
When a practice manages billing in-house, leadership has direct oversight of claims, denials, and AR follow-up on a day-to-day basis. With Outsourced Medical Billing Services, that immediate visibility is reduced, and providers must rely on vendor reports and communication channels. This can create a sense of disconnect, especially for practices accustomed to hands-on management.
To mitigate this, providers must establish clear service-level agreements (SLAs) with their outsourcing partner. SLAs should define turnaround times for claim submission, denial appeals, AR follow-up, and reporting frequency. Without strong contractual safeguards, a practice may feel less control over its revenue cycle, which can directly impact financial stability.
2. Data Security and HIPAA Compliance Risks
One of the biggest concerns in outsourcing medical billing is HIPAA compliance and data security. Patient health information (PHI) is highly sensitive, and any breach can result in regulatory penalties, reputational harm, and patient mistrust. Not all vendors maintain the same level of security infrastructure, creating potential risks.
Before contracting, practices must verify that the vendor has robust cybersecurity protocols, HIPAA training, and Business Associate Agreements (BAAs) in place. This includes confirming the use of encrypted data exchange, role-based access, secure servers, and regular compliance audits. Failure to confirm these safeguards exposes providers to liability if a vendor mishandles PHI.
3. Hidden Costs
While medical billing outsourcing is marketed as a cost-saving solution, some providers encounter hidden costs of outsourcing medical billing that were not clear during initial negotiations. These may include additional charges for denial appeals, secondary insurance submissions, credentialing support, or patient collections.
Such hidden costs can erode the financial advantages of outsourcing if not identified upfront. Practices should conduct a detailed cost analysis of outsourced billing contracts, carefully reviewing service inclusions and exclusions. Transparent vendors provide flat-rate or percentage-based pricing with minimal extra charges, but less reputable companies may bury add-ons in fine print.
4. Vendor Dependency
Another potential drawback of outsourcing billing services is becoming overly reliant on a single vendor. If the outsourcing partner fails to meet performance expectations, experiences staffing issues, or suffers from system outages, the provider’s revenue cycle may be disrupted. Transitioning to a new vendor is possible but can be time-consuming and disruptive, especially if data migration is complex.
To reduce vendor dependency risks, practices should build redundancy into their billing workflows and retain access to all claim and AR data within their own systems. This ensures that if the outsourcing relationship deteriorates, the practice can transition more smoothly without jeopardizing collections or compliance.
Is Outsourced Medical Billing Worth It for Small Practices?
For small and solo practices, medical billing outsourcing often delivers significant advantages. Hiring and maintaining an in-house billing team is expensive, requiring salaries, training, software, and compliance oversight. By outsourcing, smaller practices gain access to certified coding expertise, advanced claim tracking technology, and reduced administrative burdens all at a lower overall cost.
Clinics with fewer than 10 providers especially benefit, as outsourcing helps stabilize revenue and reduce compliance risks. While cost savings and efficiency are clear advantages, contracts should be carefully reviewed to avoid hidden fees. When structured properly, outsourcing offers small practices a reliable way to improve cash flow and focus on patient care without the weight of managing a full billing department.
Cost Analysis: How Much Does Outsourced Medical Billing Cost in 2025?
Medical billing outsourcing cost models vary, but typically fall into three categories:
| Pricing Model | Typical Range | Notes |
|---|---|---|
| Percentage of Collections | 4% – 8% of monthly collections | Most common; aligns vendor success with practice revenue. |
| Per-Claim Fee | $3 – $7 per claim | Suited for high-volume practices; may exclude follow-up services. |
| Flat Monthly Fee | $1,000 – $5,000+ | Best for large practices needing predictable costs. |
Key insight: While outsourcing can appear costly, when factoring in overhead savings (staff salaries, software, training), most practices see net cost savings of 20–40% compared to in-house operations.
What Risks Are Involved with Outsourced Medical Billing?
Compliance Risk
One of the most significant risks in medical billing outsourcing is compliance. If a vendor fails to maintain HIPAA and CMS standards, practices may face severe penalties for breaches of protected health information (PHI). Without proper Business Associate Agreements (BAAs) and secure data handling protocols, providers expose themselves to regulatory and legal consequences.
Denial Risk
Accurate coding requires specialty-specific knowledge. If an outsourcing partner lacks this expertise, claims may be submitted incorrectly, leading to frequent denials and delayed payments. Inconsistent denial management processes can further disrupt the revenue cycle, directly affecting cash flow and reimbursement timelines.
Financial Risk
While outsourcing often reduces costs, poorly structured contracts may introduce hidden fees. Vendors may charge extra for denial appeals, credentialing support, or secondary claim submissions. These costs can add up quickly, undermining the expected savings from outsourcing. Careful contract review is essential to avoid financial surprises.
Reputation Risk
Some outsourcing vendors handle patient-facing billing and collections. If these interactions are managed poorly, patients may experience confusion, frustration, or even aggressive collection practices. This not only harms patient trust but can also damage the provider’s professional reputation and patient retention rates.
In-House vs. Outsourced Medical Billing: Which Is Better?
In-House Billing
For larger healthcare groups or hospital systems, in-house medical billing can be advantageous. These organizations typically have the resources to support full compliance teams, certified coding staff, and robust IT infrastructure. With these safeguards in place, they maintain direct control over the revenue cycle, allowing for greater oversight of claim submission, denial management, and payer negotiations.
Outsourced Billing
Comparison Table:
| Factor | In-House | Outsourced Medical Billing |
|---|---|---|
| Cost | High (staff, software, training) | Lower (service fee, scalable) |
| Control | Maximum | SLA-based, less direct |
| Expertise | Depends on internal staff | Certified coders, multi-specialty RCM experts |
| Scalability | Limited | High |
| Denial Prevention | Inconsistent | Structured workflows |
Choosing the Right Outsourcing Partner
To succeed with outsourcing, providers must choose a partner with:
- Proven clean claim rates (>98%)
- Transparent reporting and analytics
- Specialty-specific coding expertise
- HIPAA-compliant, audit-ready systems
- SLA-based contracts ensuring accountability
Why Pro-MBS Is the Best Choice for Outsourced Medical Billing
When it comes to Outsourced Medical Billing, not all vendors deliver the same level of accuracy, compliance, and revenue cycle performance. Pro-MBS stands out because we go beyond routine claim submission. We integrate advanced denial prevention workflows, payer-specific rule validation, and compliance-driven audits into every step of the billing process. This ensures that providers not only get paid faster but also remain audit-ready in an increasingly regulated environment.
Our team of certified coders, AR specialists, and compliance professionals is trained across multiple specialties, from high-volume primary care to complex fields like oncology and orthopedics. We leverage technology-enabled claim tracking and real-time reporting to give providers complete visibility into their revenue cycle while reducing administrative burden. Unlike generic billing vendors, Pro-MBS builds SLA-based partnerships that guarantee measurable outcomes such as higher clean claim rates, reduced AR days, and stronger cash flow stability.



