Neurosurgery Billing Services guide each step of the payment path for complex cases. So what’s the best way to keep claims safe when payers watch every small detail? The answer sits in a clean and simple workflow that stops errors early.
Neurosurgery cases move fast, yet payers slow them down with tight review. They follow rules from CMS and AMA, and they expect each part of the record to match. One small gap can cause a denial that drags on for weeks.
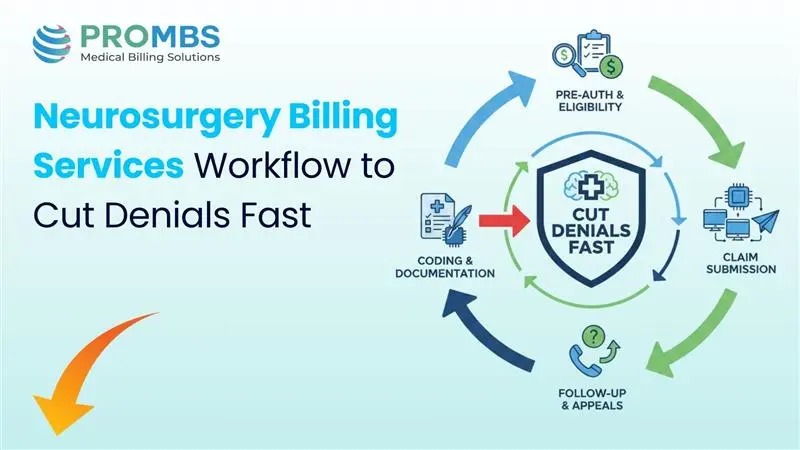
This guide shows how to build a steady billing path for all neurosurgery services. It uses short steps, clear notes, and smart checks. Each part works together to cut denials before they start.
Let me walk you through the workflow and ask the key question at each stage. How can these steps make payment faster and smoother?
Why Do Neurosurgery Billing Services Need a High-Precision Workflow?
Neurosurgery billing needs more care than most fields. The work is complex. The risks are high. And the codes bring high RVUs that attract close payer eyes. That pressure creates the need for a sharp, steady path.
So why do denials happen so fast in neurosurgery? It often starts with unclear notes. A missing spine level. A short line about the approach. No mention of devices used in the case. These small gaps lead review teams to hold or deny the claim.
Payers lean on CMS and AMA rules when checking medical need. They want a clean story from the first visit to the final bill. If any part feels unclear, the claim slows down or stops.
Neurosurgery services cover spine work, cranial work, trauma, and more. Each case needs simple and steady records. A tight workflow guards the claim and protects the practice.
Step 1: Pre-Auth Steps for Safer Claims
Pre-auth is the first test. What’s the best way to make it smooth? Give the payer every key detail before the case starts, and let Neurosurgery Billing Services guide the flow.
Almost all neurosurgery cases need pre-auth. Plans want proof that surgery is needed. They want imaging like MRI or CT. They want notes that show the patient tried safer care first. They want the surgeon’s reason for choosing surgery now.
Here is what pre-auth needs:
| Requirement | Purpose | Notes |
|---|---|---|
| MRI or CT | Shows real need for surgery | Needed by most plans |
| Conservative care notes | Shows patient tried simple care first | Important for spine cases |
| Surgeon reason | Links findings to surgery choice | Must match ICD-10 |
Step 2: How to Write Strong Operative Notes
Levels, Laterality, and Approach
Implants and Devices
Intraoperative Events
If anything changed during the case, it must appear in the note. These details help coders match the right codes and help payers follow need. A clear record of each turn keeps the claim safe.
Neurosurgery Billing Services use templates to make this step easy. These templates help surgeons write clear notes that support billing and keep claims safe.
Step 3: Smart Coding Basics for Clean Claims
Why is coding the number one cause of neurosurgery denials? Because codes must match each detail of the OR note. And even one small mismatch can spark an edit.
- CPT Categories: Neurosurgery uses codes for spine, cranial, trauma, and neurostimulation. Each group has strict rules set by the AMA. Coders must follow these rules to avoid errors.
- Modifier Accuracy: Modifiers like 51, 59, 62, 80, 82, and AS help explain the case. Wrong use can trigger bundling edits or stop the claim. Clean claims need clean modifier use.
- ICD-10 Linking: The diagnosis code must match the symptoms, imaging, and plan. CMS rules require this link. If the link is weak, medical-necessity denials rise fast.
Coding drives payment. A clear OR note and skilled coding shape a claim that moves through payers without trouble. Strong Neurosurgery Billing Services help keep that path clean.
Step 4: Claim Scrubbing for Fewer Denials
Claim scrubbing is the final check before submission. What’s the best way to lower risk? Find errors before the payer does.
Scrubbing reviews medical need, NCCI edits, MUEs, and the full code set. It catches mismatched codes and stops unbundled pairs. It checks for missing documents.
Neurosurgery claims often need more files than other fields. OR notes. Implant logs. Imaging. Without these, payers may deny or delay the claim, which strong Neurosurgery Billing Services work hard to prevent.
A clean scrub followed by correct routing helps the claim reach the right payer lane. This step can save weeks of waiting and remove many preventable denials.
Step 5: Fast AR Follow-Up and Denial Fixes
What should the team do once the claim leaves the office? Move fast. High-value claims need tight follow-up, the kind supported by strong Neurosurgery Billing Services.
Many denials fall into simple groups:
• Missing pre-auth
• Weak medical need
• Bundling errors
• Note and code mismatch
AR teams check claims every 24 to 48 hours. This pace keeps cases from sitting in queues. If a payer denies the claim, the appeal must be strong. Appeal letters need clear patient facts.
They also use CMS need rules and AMA coding rules. These letters help show why the surgery was right and why the claim should be paid.
If a payer still blocks the claim, the team can request a second review. If needed, they move to peer-to-peer. Each step gives the case a new chance.
What Makes Pro-MBS a Strong Partner for Neurosurgery Billing Services?
Your practice needs a team that knows how to protect complex claims. Pro-MBS supports all neurosurgery work with a clear workflow and steady follow-up. Their team keeps claims clean with simple tools, smart scrubbing, and strong coding help.
They also handle tough denials fast and help your office understand what caused them. You get clear reports and weekly talks, so your team stays informed. If you want fewer denials and faster pay, Pro-MBS can help your practice stay strong and steady.
If your neurosurgery billing workflow needs fewer denials and faster pay, Pro-MBS can help. They bring skill and strong systems to your team through trusted Neurosurgery Billing Services.
People Also Ask
What makes Neurosurgery Billing Services so strict?
These claims move under tight eyes. Small gaps spark fast denials. That’s why Neurosurgery Billing Services must follow each step with care. Clean notes and strong proof keep the claim alive. For steady support, reach out to Pro-MBS.
How do Neurosurgery Services link to strong billing results?
Good care needs good records. Neurosurgery Services create the story that the claim must follow. Each detail shapes how payers judge the case. Clean steps protect your pay path. For help with both sides, trust Pro-MBS.
Why does pre-auth matter so much in Neurosurgery Billing Services?
Pre-auth is the first gate. If the notes miss one key fact, the claim can fall. Neurosurgery Billing Services use clear steps to keep that gate open. Strong checks save time and stress. Let Pro-MBS guide the process.
How do strong OR notes protect Neurosurgery Services?
Simple lines carry power. A full OR note shows what happened and why it mattered. It keeps Neurosurgery Services safe from denials. When notes stay sharp, claims stay steady. For safer workflows, partner with Pro-MBS.
What coding mistakes cause most denials in Neurosurgery Billing Services?
Missed links. Wrong modifiers. Codes that drift from the OR note. These small slips can stall the claim. Neurosurgery Billing Services keep each code tight and true. For cleaner claims, work with Pro-MBS.
Why is follow-up so critical in neurosurgery claims?
Payers move slow, but denials hit fast. Strong follow-up keeps claims alive. It guards both billing and Neurosurgery Services from long delays. Fast checks bring fast pay. Stay ahead with Pro-MBS.
How can Pro-MBS help reduce denials in Neurosurgery Billing Services?
They track each step with care. They clean claims, fix gaps, and move cases forward. Their work boosts both billing and Neurosurgery Services. When trouble hits, they act fast. For true support, choose Pro-MBS.