Physical Therapy Billing Mistakes don’t always shout. They whisper. They hide inside modifiers, time logs, and treatment notes. And before you notice, they’ve quietly taken a bite out of your revenue. What’s the best way to stop that bleed? You’d think billing is simple, code, submit, get paid. But in physical therapy, nothing is ever that clean. One small mistake can turn a $200 session into a denied claim.
That’s the reality many clinics face every day. The errors aren’t always big, but their impact is. Miss a modifier? The claim gets rejected. Forget to justify medical necessity? The payer flags you. And if you ignore these patterns, your clinic bleeds cash month after month. Let’s walk through what really causes those denials and how you can stop them.
Why Physical Therapy Billing Needs Precision
Have you ever asked why physical therapy billing feels more complicated than other specialties? It’s because every minute counts. Each CPT code, each modifier, even each payer has its own set of rules. CMS defines strict time-based coding standards, and AMA guidelines require exact documentation for medical necessity.
So when a therapist misses the 8-minute rule or confuses a service code, it’s not just a small oversight. It’s a compliance risk. And compliance mistakes don’t vanish quietly. They leave a trail of denials, repayments, and sometimes even audits. Every minute in physical therapy billing matters. CMS calls it out clearly. If your time doesn’t match the code, the code doesn’t get paid. It’s that simple. One wrong calculation can shift a claim from valid to void. And payers notice. They always notice. They expect precision, clean notes, correct codes, clear intent. Anything less, and the system grinds to a stop. Claims sit in limbo. Cash flow slows. Staff scramble to find what went wrong.
Billing in physical therapy isn’t just about numbers. It’s about discipline. Every note, every code, every minute logged is a promise to your payer. Break that promise, and payment disappears. One mistake may seem small, but Physical Therapy Billing Mistakes never stay small. They stack, they echo, and they cost you. Precision isn’t a choice. It’s survival. The clinics that win don’t rush. They focus. They care.
Did You Know?
According to CMS, nearly 20% of physical therapy claim denials result from timing and modifier errors. One misplaced modifier can turn a clean claim into a compliance risk. Precision isn’t paperwork. It’s profit protection.
What Is the Best Way to Avoid Physical Therapy Billing Mistakes
Errors may seem harmless until they start stacking up. One missed note. One wrong modifier. One small oversight that no one catches. Then suddenly, the numbers stop making sense. Reimbursements dip. Payments drag. Denials pile up. It doesn’t happen all at once. It happens quietly, in the background, while your team keeps moving. You don’t notice the leak until the bucket is half empty.
That’s how most Physical Therapy Billing Mistakes begin. Small, silent, and consistent. A code left unchecked. A report not updated. A modifier skipped because it didn’t seem important. But every little slip carries weight. Each error adds another barrier between your clinic and your payment. Over time, those barriers become walls. So, what are the most common Physical Therapy Billing Mistakes that drain your revenue? Let’s break them down and see where clinics lose the most money, and how to stop it before it starts.
| Mistake | Impact on Revenue | Prevention Strategy |
|---|---|---|
| Missing or incorrect modifiers (e.g., 59, KX) | Causes automatic claim rejections | Train staff on modifier use and payer policies |
| Time-based code miscalculations | Leads to underbilling or overbilling | Apply the CMS 8-minute rule correctly |
| Lack of medical necessity documentation | Denials for insufficient proof of therapy need | Keep detailed notes tied to functional goals |
| Incomplete progress reports | Payers may stop payments mid-treatment | Schedule report reviews regularly |
| Overlapping CPT codes | Flagged for potential duplication | Audit claims before submission |
| Ignoring payer-specific edits | Repeated denials and delays | Maintain payer rule reference sheets |
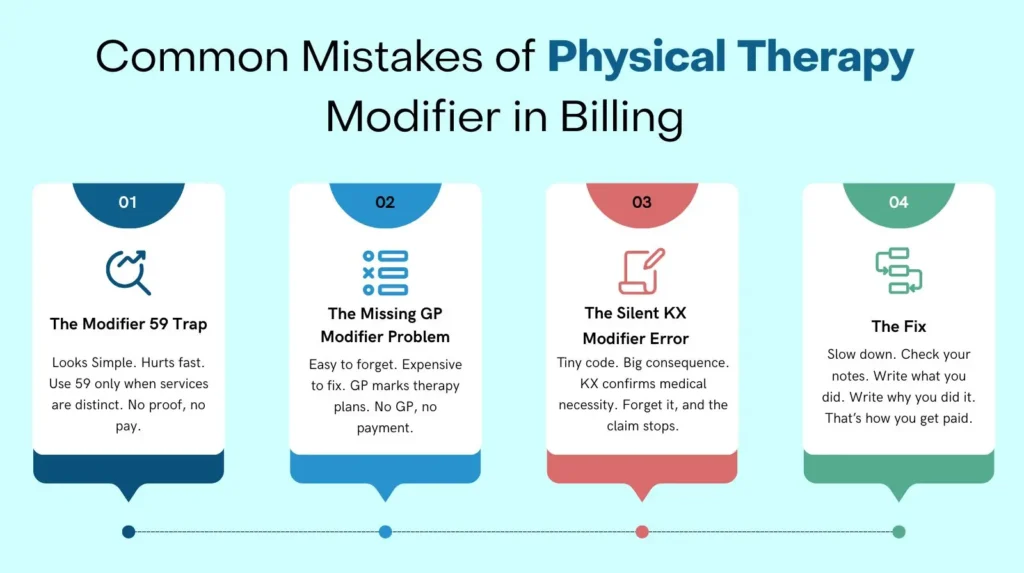
But what do these really mean day to day? Think about missing modifiers. AAPC data shows modifier errors are among the top three causes of denials in outpatient therapy. Why? Because they tell payers that your procedures are distinct and billable. Forget to use them, and your claims lose context.
Or take time-based coding. It sounds simple, but therapists often miscount total treatment minutes. Underbill, and you lose money. Overbill, and you invite an audit. Neither option ends well. Every error tells the same story: lost time, lost money, and more stress for your billing team.
The Real Cost of PT Billing Errors
So what’s the price of a mistake? Let’s say your clinic processes 500 claims a month. If just 10% are denied due to incorrect modifiers or missing documentation, you’re looking at 50 delayed claims. At an average of $120 per session, that’s $6,000 locked up, money you might never see again. CMS reports that over 12% of therapy claims are denied for preventable documentation issues. AAPC found that 15% of PT claims get flagged for modifier misuse.
That’s real money, lost for small errors. And it’s not just the revenue you lose, it’s the time you spend chasing it. Every reworked claim takes an average of 15 to 30 minutes to fix. Multiply that across dozens of denials, and your staff loses entire days. Cash flow slows. Stress builds. Suddenly, your clinic’s biggest problem isn’t patient care. It’s paperwork. So, what’s the fix? It starts with stronger documentation.
But fixing lost revenue starts long before the claim is sent. It begins with what you write. And how you document it.
Did You Know?
AAPC reports that 15% of outpatient therapy claims are denied due to modifier misuse. Most are preventable with better documentation and staff training. Every denied claim is lost time and a lost revenue.
Documentation Is Your Defense
What’s the first thing an auditor checks? Notes. Always notes. Good documentation doesn’t just tell a story. It proves it. It connects every treatment to a medical necessity, every minute to a measurable outcome. According to AMA, each entry must show why therapy was needed, what was done, and how the patient responded.
Here’s a quick checklist to tighten your documentation game:
- Write clear, concise daily notes that reflect measurable progress.
- Record total time for each time-based CPT code.
- Tie every service to a treatment goal and functional outcome.
- Review documentation weekly for completeness.
- Keep all progress reports updated and signed.
Miss one step, and a payer might call your service “not medically necessary.” And once they do, you’re not getting that money back. But when your notes are airtight, something powerful happens. Denials drop. Payers stop second-guessing you. And your staff stops wasting hours fixing preventable errors.
How Compliance and Training Drive Real Revenue
What if compliance wasn’t a chore but a moneymaker? Most clinics see audits as threats, not opportunities. But in truth, compliance and education build your revenue’s safety net. When your team understands CMS documentation standards and modifier requirements, mistakes shrink fast. They catch issues before they hit a claim. Every corrected error becomes recovered revenue.
Many physical therapy practices underestimate this. They focus on speed instead of accuracy, believing more claims mean more money. But without a solid compliance process, those fast claims turn into slow payments. Accuracy is the real growth engine.
Turn Compliance into Opportunity
Compliance isn’t a box to check. It’s a tool to protect your income. CMS and AMA guidelines exist to ensure fair and accurate reimbursement. Not to slow you down. Clinics that follow these rules closely often see cleaner claim rates and also fewer payer disputes. The smartest clinics treat compliance as a business strategy, which track denial trends and review payer feedback. It uses that data to improve billing precision. When compliance becomes part of daily operations, it changes from obligation to opportunity.
Training Is the Real Revenue Booster
How do you make that happen? Through training. Not once a year, but continuously. Run mock audits and code reviews. Share payer bulletins with your team. Discuss real examples of denials and show what caused them. The more your staff sees how small errors lead to lost revenue, the more invested they become in accuracy. Training also builds confidence. When coders and therapists understand the “why” behind every rule. They make smarter decisions. And fewer mistakes.
Build a Culture of Collaboration
Revenue health depends on teamwork. Coders, therapists, and billing specialists should never work in silos. Collaboration closes the gaps where denials hide. Hold short huddles to review complex claims. Encourage therapists to document clearly so coders can bill with precision. Let billers share common payer issues during team meetings. Each conversation strengthens your compliance chain. When everyone owns the process, your practice moves faster. Claims go out clean, payments come in sooner, and frustration fades away.
Compliance That Pays for Itself
Compliance doesn’t slow you down. It speeds you up. The time you spend training today saves hours of rework tomorrow. Each accurate claim reduces denials, improves cash flow, as well as boosts your payer’s trust. Smart training turns compliance into confidence. And confidence into consistent revenue. Think of it this way: every dollar you invest in staff education returns tenfold through clean claims and fewer audits. And also through steady growth. That’s the secret many clinics overlook. Compliance isn’t a cost. It’s a profit center waiting to be used.
Did You Know?
Clinics that conduct quarterly compliance training reduce PT billing errors by over 25%. That means faster payments, fewer denials, and stronger relationships with payers. Knowledge truly pays for itself.
How Pro-MBS Helps Physical Therapy Practices Stay Audit-Proof
What if you didn’t have to fight denials alone? That’s where Pro-MBS steps in. Our team specializes in physical therapy billing, coding audits, and payer compliance. We know the rules because we live by them. We don’t just fix errors; we find their root cause. We review your CPT coding, modifiers, and documentation line by line. We help you align with CMS and AMA standards so your claims get paid the first time.
Want proof? Our clients see denial rates drop by up to 25% within three months of partnering with us. That’s more money in your account and less stress for your team. So, what’s the best way to protect your practice? Don’t wait for the next denial. Get ahead of it. If your PT practice is losing money to avoidable denials, Pro-MBS can help you recover revenue and stay audit-ready.
Did You Know?
The OIG has reported that nearly one in four symptom-based claims are denied due to incomplete documentation or ICD–CPT mismatch errors. PROMBS’ structured claim-preparation and compliance auditing process built on CMS and AHIMA validation protocols ensures that each abdominal tenderness icd 10 code (R10.819) claim passes both compliance and payer scrutiny with precision.
Frequently Asked Questions
What is the biggest issue in physical therapy?
The real threat hides in the notes. Poor documentation fuels Physical Therapy Billing Mistakes, turning clean claims into denials. Miss a progress report, skip a goal, lose the payment. Pro-MBS builds your defense through stronger documentation and compliance systems that keep cash flow alive and steady.
Which are common problems that may occur during the billing process?
The usual suspects never change. Missing modifiers. Wrong codes. Miscounted minutes. Each one bleeds revenue in silence. Pro-MBS audits your process, fixes these Physical Therapy Billing Mistakes, and trains your team to catch errors before payers do.
What is the 8-minute rule for physical therapy billing?
The 8-minute rule decides how time-based CPT codes live or die. Eight minutes earns one unit, twenty-three earns two. One miscount, and your revenue slips away. Pro-MBS automates your timing checks to eliminate one of the most common Physical Therapy Billing Mistakes before it reaches Medicare.
What is the biggest challenge in medical billing?
The challenge is constant change. Payer rules shift. Modifiers evolve. Audits tighten. Most clinics chase speed and lose accuracy. Pro-MBS brings structure, mastery, and real-time updates so your team stays compliant and your billing never falls behind.
What are examples of incorrect pay billed errors?
Wrong codes. Wrong units. Wrong payer. These small errors define most Physical Therapy Billing Mistakes. Each one confuses payers and drains revenue drop by drop. Pro-MBS conducts precision audits that clean your claims, restore accuracy, and keep your payments flowing on time.
What is a red flag in physical therapy?
A missing note. A vague plan. A treatment without proof. That’s what auditors call a red flag. It signals risk, overbilling, and noncompliance. Pro-MBS locks your documentation to CMS and AMA standards so every claim stands strong and every audit passes clean.
What does claim submitted to incorrect payer mean?
It means time lost and money trapped. Sending a claim to the wrong payer is one of the simplest yet most damaging Physical Therapy Billing Mistakes. Eligibility checks are your shield. Pro-MBS builds payer verification into your workflow so your claims reach the right hands the first time.