Physical Therapy Claim Submission sounds simple on paper, but in real life, it’s a constant race against time. Every day a claim waits in the queue, your clinic’s revenue slips further out of reach. Therapists work hard, patients improve, but payments still lag. Sound familiar?
What’s the best way to fix that? How do you move from delayed claims and denials to clean, fast payments? The answer lies in smarter systems, automation, and tighter teamwork between clinical and billing staff. According to CMS, nearly 25% of outpatient therapy claims face delays because of missing or incorrect data. That’s money sitting idle. Let’s talk about how to stop that from happening.
Why Claim Submission Speed Matters in Physical Therapy?
Why does timing matter so much in billing? Because every day of delay slows your cash flow. The longer your accounts receivable stay open, the higher the chance of missing filing deadlines. Most payers give you 90 to 120 days to submit a claim. Miss that window and the payment is gone.
The Healthcare Financial Management Association (HFMA) reports that billing delays can stretch AR days by 30 to 40 percent. That kind of lag drains morale and disrupts your revenue cycle. Faster claim submission doesn’t just mean quicker payments. It keeps your clinic compliant, efficient, and less stressed.
💡 Did You Know?
Speed pays. CMS found that outpatient therapy claims sent within 48 hours get paid up to 35 percent faster. Wait five days, and the clock starts to drag. HFMA reports that every week of delay adds almost 40 percent more time to your AR cycle. Fast claims mean faster cash. Quick submission isn’t just good practice. It’s real money back in your pocket.
Common Causes of Delayed Physical Therapy Claim Submission
Ever wonder why claims get stuck? It’s almost never one giant mistake. It’s a hundred tiny ones hiding in plain sight. A therapist forgets a signature. A note sits unfinished. A code doesn’t match the service. One delay becomes two. Two turn into ten. Before you know it, a week’s worth of visits is sitting in limbo.
Manual entry makes it worse. One wrong digit and the claim stops moving. Missing authorizations pile up. Eligibility expires quietly in the background. Then comes the real pain. The clock keeps ticking while your cash flow stands still. By the time someone notices, the filing window has already shrunk and your team is racing the deadline. Below are the common causes of delayed Physical Therapy Claim Submissions
- Incomplete Documentation: Therapists skip a signature. Minutes go missing. A single unchecked box can stop a claim cold. AMA reminds clinics that signed notes aren’t just paperwork. They are proof of care. Without them, payers simply say no.
- Manual Charge Entry: One person. One keyboard. One wrong digit. That’s all it takes to turn a clean claim into a rejection. Fatigue sets in. Codes blur together. Accuracy fades. Automation never gets tired. It keeps every CPT code exact.
- Insurance Errors: Policies change. Authorizations expire. Eligibility gets ignored. And the claim ends up dead on arrival. Real-time verification catches those mistakes before they spread. It’s faster to check once than fix it five times later.
- Workflow Gaps: Notes wait. Billers wait. The clock doesn’t. A few late submissions can snowball into weeks of delay. When therapists document daily, billing stays on track. That’s the rhythm every clinic needs.
- Poor System Integration: Two systems. No connection. Endless waiting. Data falls through the cracks while claims sit unfinished. When your EHR and billing platform sync perfectly, nothing gets lost. Not time. Not money.
Picture a traffic jam. Each step, from therapist to biller to clearinghouse, can become a red light if not managed right.
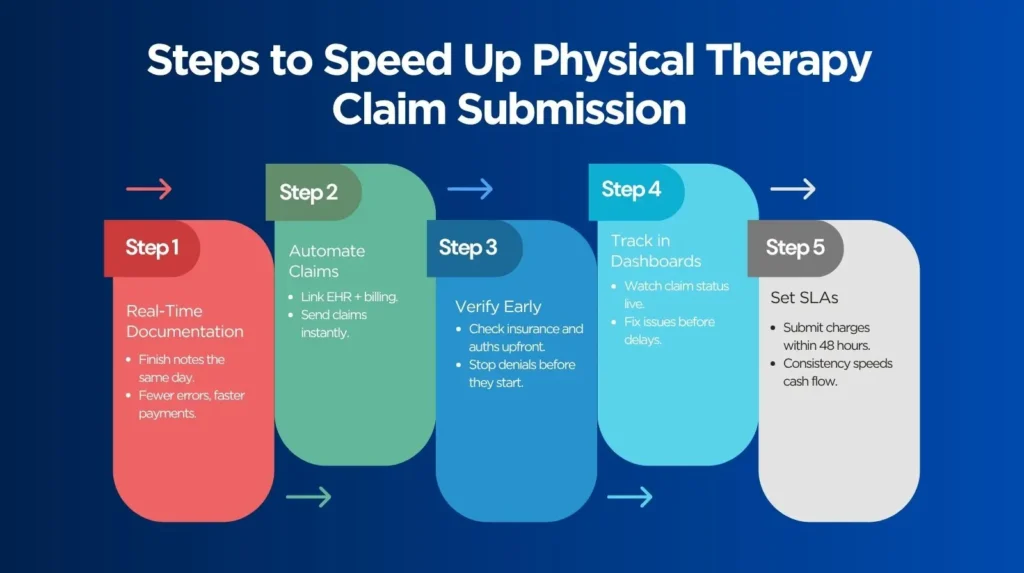
Steps to Speed Up Physical Therapy Claim Submission
Adopt Real-Time Documentation Practices
What if your therapists finished notes the same day as the visit? That one habit can change everything. Same-day documentation keeps your billing cycle tight and predictable. Use ready-made templates for common codes like 97110 and 97140. CMS points out that real-time documentation cuts coding errors and keeps you compliant. The sooner the notes are done, the faster the money moves.
Automate Claim Creation and Submission
Verify Patient Information Upfront
How often do claims bounce back for simple insurance mistakes? Too often. Run eligibility checks before the first session. Confirm authorizations early so nothing stops the payment later. AMA recommends checking coverage every 30 days for long-term therapy cases. It takes minutes to verify but days to fix a denial.
Use Claim Tracking Dashboards
Would you know if a claim got stuck yesterday? Dashboards show you the truth in real time. See which claims are sent, which are pending, and which need attention. You don’t have to wait for a rejection letter. You can act before the delay turns into lost revenue.
Set Internal SLAs
Set rules and stick to them. Make it clear that all charges must be submitted within 48 hours of each visit. The Medical Group Management Association (MGMA) reports that practices with firm SLAs reduce AR days by 20 percent or more. Consistency speeds everything up. The faster you submit, the faster you get paid.
Leverage Automation and Analytics for Efficiency
Data doesn’t lie. Automation and analytics reveal where delays happen before they cost you money. Automation tools catch missing fields before submission. Analytics show you how long claims take to move through each stage. You’ll know which payers delay the most and which therapists need support with documentation.
Key Metrics to Monitor:
- Submission Turnaround Time: Count the days between the visit and the claim. Fewer days, faster cash. Every extra hour slows your revenue.
- Clean Claim Rate: How many claims get accepted on the first shot. The higher it is, the smoother your billing runs. One clean claim saves hours of fixing.
- First-Pass Resolution Rate: How many claims get paid the first time. No edits. No rework. Just clean, quick payments that keep your cash flow alive.
Dashboards replace guessing with control. You spot problems as they appear, not weeks later.
Strengthen Coordination Between Clinical and Billing Teams
Do your therapists and billers communicate daily? If not, you’re probably losing time.
Many delays start with poor communication. Set up quick weekly huddles. Review open claims together. Use shared tools like Teams or Slack to flag missing notes or coding issues immediately. CMS advises regular coordination between clinical and billing teams to keep documentation accurate and avoid compliance risks.
When everyone works together, everything clicks. Claims stop crawling and start moving. Denials drop before they ever reach the payer. The billing team stays ahead instead of playing catch-up. Therapists focus on care, not paperwork. Billers focus on accuracy, not chasing notes. Stress fades, and the numbers finally make sense. Collaboration isn’t just nice to have. It’s the engine that keeps revenue alive and your clinic running smooth.
Improve Payer Communication and Clearinghouse Integration
o you know how your clearinghouse interacts with your payers? That often explains recurring delays. Direct payer connections reduce waiting time and transmission errors. Automated payer response tracking catches rejections instantly. Instead of waiting for a letter, your system alerts you as soon as something goes wrong.
Rejection reports are more than paperwork. They’re a roadmap to improvement. The American Academy of Professional Coders (AAPC) recommends reviewing rejection trends regularly to guide cleaner future submissions.
| Process | What It Does | Why It Matters |
|---|---|---|
| Direct Payer Connections | Send claims straight to payers without third-party delays. | Reduces waiting time and transmission errors. |
| Automated Payer Response Tracking | Flags rejections and errors as soon as they happen. | Helps staff fix issues before resubmission deadlines. |
| Clearinghouse Integration | Syncs your EHR and billing systems for real-time claim updates. | Keeps all teams aligned and informed. |
| Rejection Reports Review | Identifies recurring errors or weak points in documentation. | Improves clean claim rate and first-pass resolution. |
Better payer communication changes everything. Payments move faster. Errors drop before they reach the payer. Surprises disappear because your team already knows what’s coming. Clear reports replace guesswork. You stop reacting and start controlling the process. With real-time feedback, every claim becomes a closed loop. That’s how strong communication turns billing chaos into steady, predictable cash flow.
Measure and Maintain Your Progress
You can’t improve what you don’t track. Consistent performance reviews are essential. Set measurable goals. Try to submit 95 percent of claims within 48 hours. Track clean claim rate, AR days, and denial rates every month.
When numbers slip, investigate why. Did documentation lag? Did a payer change its policy? Continuous monitoring keeps your workflow sharp. Quarterly workflow audits, as encouraged by CMS, help identify compliance risks before they become costly problems.
Partner with Pro-MBS for Fast, Accurate Claim Submission
Keeping up with billing rules and payer changes takes time that most therapy clinics simply don’t have. Every payer updates requirements. Every form seems to change overnight. Staying compliant feels like a full-time job on its own. That’s where Pro-MBS steps in. We handle the complexity so you can focus on patients, not paperwork. Our team tracks payer updates, manages submissions, and fixes issues before they ever reach your desk. While others chase denials, you stay ahead.
Our team specializes in physical therapy billing and automation. We deliver a 98.9 percent clean claim rate and an average 48-hour submission turnaround. Every claim is tracked in real time through secure, HIPAA-compliant dashboards that give you full visibility. Our process focuses on speed, accuracy, and peace of mind so your staff can focus on care, not chasing payments.
Frequently Asked Questions
What is the 15-minute rule for physical therapy?
Fifteen minutes. One unit. Eight minutes minimum. That is the rule. It keeps time, care, and payment aligned. Follow it and your Physical Therapy Claim Submission stays clean and compliant. At Pro-MBS, we turn those minutes into money that moves on time.
How to avoid timely filing denials?
Denials don’t come from chance. They come from delay. Document daily. Verify early. Automate everything. Real-time tracking keeps your Physical Therapy Claim Submission alive before deadlines close. Pro-MBS makes sure your claims never miss the clock.
How to maximize physical therapy billing?
Speed starts with structure. Notes on time. Data synced. Codes checked. Automation in PT billing keeps every move sharp and seamless. Pro-MBS builds that flow so your Physical Therapy Claim Submission turns effort into revenue.
What is a red flag in physical therapy?
A missing signature. A wrong modifier. A note that doesn’t match the code. Each one slows your claim like sand in a gear. Clean notes mean clean claims. Pro-MBS helps you catch red flags before they cost you cash.
What happens if you don’t meet the 8-minute rule?
Less than eight minutes means no claim. No exceptions. CMS calls it non-billable. Keep logs tight and sessions documented. Precision protects your Physical Therapy Claim Submission from rejections. Pro-MBS keeps your timing, coding, and payments aligned.
What is the claim submission process?
It starts with notes and ends with money. Documentation, coding, verification, submission. Each step needs to move as one. When automation connects them, the process runs silently and fast. Pro-MBS keeps your Physical Therapy Claim Submission smooth from start to payment.
How do I submit a reimbursement claim?
Collect the data. Verify coverage. Match CPTs. Send it clean and digital. That is how reimbursement happens without friction. PT billing automation makes it instant. Pro-MBS turns your Physical Therapy Claim Submission into a system that pays back fast.



