In 2025, the prior authorization revenue bottleneck continues to challenge healthcare providers, clinics, and hospitals alike. Despite payer commitments to streamline the process and new federal reforms mandating electronic prior authorization (ePA), practices still report significant delays, rising denials, and high administrative costs tied to PA.
The American Medical Association (AMA) notes that 94% of physicians report care delays related to prior authorization, with 33% claiming these delays have led to serious adverse events for patients. From a financial standpoint, PA remains the single largest drag on revenue cycle management (RCM), costing practices thousands in lost reimbursements and staff productivity each month.
This blog breaks down why prior authorization remains the number one revenue bottleneck in 2025, its operational and financial implications, and how healthcare organizations can adopt smarter strategies to overcome it.
What Is Prior Authorization?
Prior authorization (PA) is a payer-mandated process requiring providers to obtain approval before delivering specific medications, imaging, procedures, or therapies. Insurers use PA to control costs, reduce unnecessary services, and ensure medical necessity.
How Does the Prior Authorization Process Work Step by Step?
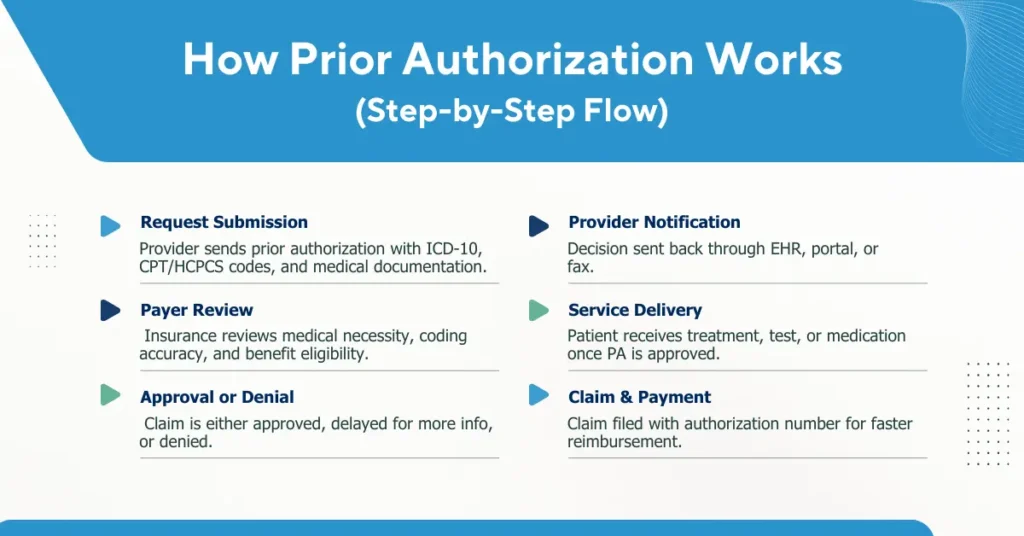
1. Request Submission
The process begins when the provider or billing team submits a prior authorization request to the payer. This submission must include complete patient demographics, accurate ICD-10 diagnosis codes, relevant CPT/HCPCS procedure codes, and supporting clinical documentation. Errors or missing details at this stage such as incomplete forms or insufficient medical necessity notes are the most common reasons for delays and denials.
2. Payer Review
3. Approval or Denial Decision
The payer then issues a decision:
- Approved: The service can move forward with an authorization number provided.
- Delayed/Pending: Additional clinical documentation, coding clarification, or physician notes are required.
- Denied: The request is rejected, often due to medical necessity disputes, coding mismatches, or missing data.
At this stage, delays are costly because they can directly impact scheduling and patient care delivery.
4. Provider Notification
The decision is communicated back to the provider via EHR integration, payer portal, fax, or phone. If approved, the provider receives an authorization number that must be included on the subsequent claim. If denied, staff must either appeal the decision or resubmit with corrected documentation, adding more administrative burden.
5. Service Delivery
6. Claim Submission & Payment
Finally, the provider submits the claim to the payer, ensuring the authorization number is attached to avoid automatic rejections. Approved authorizations accelerate claim processing and reimbursement, while missing or incorrect PA data almost always results in denials, appeals, and revenue cycle slowdowns.
Why Do Payers Require Prior Authorization?
- To validate medical necessity before approving costly or high-risk services.
- To enforce formulary or network restrictions for medications, imaging centers, or surgical facilities.
- To minimize fraud, waste, and abuse in healthcare claims.
Which Services Commonly Require Prior Authorization?
- Medications: Biologics, specialty drugs, high-cost therapies.
- Imaging: MRIs, CT scans, PET scans.
- Procedures: Cardiac interventions, orthopedic surgeries, pain management injections.
- Durable Medical Equipment (DME): Power wheelchairs, oxygen therapy.
While intended to ensure proper utilization, prior authorization has become synonymous with delays, administrative burden, and revenue leakage.
What Is the Financial Impact of Prior Authorization on Healthcare Revenue?
The financial consequences of prior authorization delays extend far beyond administrative inconvenience. For most practices, PA is not only a clinical barrier but also a direct threat to revenue integrity. Every stalled approval slows down billing, increases accounts receivable (A/R) aging, and drives up operational costs. Over time, this creates measurable revenue leakage that undermines practice profitability.
- On average, physicians process 41 PA requests per week, consuming nearly 15 staff hours weekly (AMA survey, 2024).
- Each manual PA request costs an estimated $20–$50 in administrative labor depending on complexity, and for high-cost drugs the cost can exceed $100.
- Denial rates typically fall between 15–20%, most often tied to incomplete documentation or ICD-10 mismatches, though certain specialties may experience higher spikes.
- For many practices, this equates to thousands in lost revenue each month due to delayed or denied authorizations.
What Operational Bottlenecks Does Prior Authorization Create?
The prior authorization revenue bottleneck is not only a financial drain; it also creates significant operational challenges that disrupt daily workflows across practices and hospitals.
Administrative Burden
Providers and staff spend up to 16 hours per week managing PAs, contributing to billions of dollars in wasted administrative costs annually across the U.S. healthcare system. This constant manual work limits staff productivity and diverts attention from patient care.
Payer Variability
Each insurer uses its own rules, forms, and timelines. The absence of standardization forces practices to adapt to multiple systems, creating inefficiencies and increasing the likelihood of errors or missed deadlines.
Documentation Errors
Incomplete medical records, ICD-10 code mismatches, and missing medical necessity statements are among the most common reasons for PA denials. These errors trigger rework, appeals, and extended claim cycles.
Denial Risks
Nearly 1 in 3 PA requests face initial rejection, often requiring multiple resubmissions and appeals. Each denial not only delays revenue but also ties up staff resources in repetitive follow-up.
How Does Prior Authorization Act as a Revenue Cycle Management (RCM) Bottleneck?
Within the revenue cycle, prior authorization creates a structural choke point that slows financial performance at its very first stage. Since services cannot be billed until authorization is secured, claims submission is delayed, which directly impacts cash flow and disrupts payment predictability for providers.
These delays often lead to revenue leakage, as some patients abandon or postpone care when approvals take too long. Every deferred service represents a missed billing opportunity, while pending claims extend accounts receivable (A/R) cycles and tie up valuable revenue that practices rely on for stability.
Beyond lost revenue, there are also hidden operational costs. Staff spend countless hours on manual follow-up, leading to burnout, higher turnover, and new training expenses. Taken together, these factors prove that prior authorization is not just an administrative inconvenience, it is a systemic barrier that disrupts the entire revenue cycle from scheduling through reimbursement.
What Regulatory and Industry Reforms Are Changing Prior Authorization in 2025?
Despite mounting pressure from providers and advocacy groups, prior authorization (PA) remains deeply entrenched in the U.S. healthcare system. That said, 2025 has seen meaningful regulatory and industry-driven reforms designed to reduce administrative burden and accelerate approvals. While these initiatives are promising, implementation remains slow, and their benefits have yet to fully reach providers at the point of care.
Electronic Prior Authorization (ePA) Mandates
The Centers for Medicare & Medicaid Services (CMS) finalized rules requiring Medicare Advantage and Medicaid managed care plans to adopt electronic prior authorization systems by 2027. Under this mandate, payers must process urgent requests within 72 hours and standard requests within 7 calendar days. This represents a major step toward reducing fax- and phone-based submissions, but the full rollout is still years away, and many payers have yet to upgrade their systems.
Insurer Policy Shifts
Major insurers including UnitedHealthcare, Humana, and Cigna announced plans to cut prior authorization requirements by 10–20% in 2025. They also pledged to publish greater transparency around approval and denial rates. While this reduces some friction, the cuts often apply to lower-cost services rather than the high-value specialty drugs and procedures that drive most revenue delays. As a result, the bottleneck persists for high-cost, high-priority cases.
Gold-Carding Programs
Federal Standardization Efforts
Proposed legislation, such as the Improving Seniors’ Timely Access to Care Act, seeks to mandate uniform prior authorization criteria across all payers, require clinician involvement in denial decisions, and establish minimum turnaround times. While strongly supported by groups like the AMA and MGMA, the bill remains under congressional review, with lobbying from insurers slowing its progress. If enacted, these measures would standardize a process that is currently fragmented and highly payer-specific. However, as of 2025, these bills remain under review, with lobbying from insurers slowing legislative momentum.
Why Does Prior Authorization Remain the #1 Bottleneck Despite Reforms?
Despite industry-wide reforms such as electronic prior authorization (ePA) mandates, insurer pledges to reduce requirements, and legislative efforts to standardize the process, prior authorization continues to dominate as the leading revenue bottleneck in 2025. The reason is that these reforms, while promising on paper, have not yet translated into measurable improvements for most providers. Several factors continue to reinforce PA as the most persistent choke point in revenue cycle management.
High Volume of Requests
The sheer scale of prior authorization requests overwhelms the system. According to AMA surveys, physicians face an average of 41 PA requests per week, translating into tens of millions of authorizations nationally each year. With the expansion of specialty medications, biologics, and advanced imaging services, the volume of PA requirements continues to grow rather than shrink. This workload creates unavoidable delays, as payer staff cannot process requests quickly enough to keep pace.
Fragmented Tech Adoption
While electronic prior authorization (ePA) tools are designed to accelerate turnaround, adoption remains inconsistent. Many providers still rely on fax-based forms, phone calls, and manual entry, making the process slow, error-prone, and resource-intensive. On the payer side, not all insurers have fully transitioned to ePA systems either, resulting in a fragmented landscape where technology exists but is not universally integrated. The consequence is that automation benefits are uneven, leaving bottlenecks intact.
Staff Shortages and Burnout
Administrative staff shortages amplify the bottleneck. The average practice spends 14–16 hours per week on PA tasks, with many billers and coders reporting burnout from repetitive, manual work. High staff turnover forces practices to constantly recruit and train new personnel, which further undermines efficiency. When combined with rising patient volumes, the human capital challenge makes it nearly impossible for practices to stay ahead of PA demands.
Payer Incentives and Denial Strategies
Perhaps the most under-discussed factor is that denials remain financially advantageous for payers. Every delayed or denied claim represents reduced immediate payout, improved cash flow for insurers, and, in some cases, permanent savings when providers fail to appeal. This structural incentive means that while insurers may pledge reforms publicly, their internal business models still reward friction and delays. As long as payer incentives remain misaligned with provider efficiency, the PA bottleneck will persist.
In short, reforms have not dismantled the bottleneck because the drivers volume, technology gaps, staffing shortages, and payer incentives are systemic and deeply embedded. For healthcare providers, the impact is clear: delayed care, disrupted revenue cycles, and growing administrative costs.
What Is the Best Decision Framework for Providers to Overcome Prior Authorization Bottlenecks in 2025?
When evaluating how to address the prior authorization revenue bottleneck, healthcare executives should use the following checklist:
✅ Calculate true cost-to-collect: Include staff salaries, training, software, payer portal fees, and compliance audits, then compare with outsourcing/automation costs.
✅ Review denial trends: Track how often PA-related denials occur and what percentage require appeals or rework.
✅ Assess staff capacity: Measure burnout, turnover, and retraining needs; if staff are overloaded, efficiency will continue to decline.
✅ Audit turnaround times: Monitor how long it takes for your practice to obtain approvals and whether delays impact patient care or cash flow.
✅ Evaluate scalability: Determine if your current PA process can handle growth, new locations, or increased service lines without major new investments.
✅ Weigh patient experience: Consider whether PA delays frustrate patients or contribute to care abandonment.
👉 If most of these checklist items reveal inefficiency, outsourcing or automation becomes the most financially sustainable choice.
How Does Pro-MBS Help Providers Eliminate Prior Authorization Bottlenecks?
We specialize in eliminating the inefficiencies that make prior authorization the number one revenue bottleneck for providers. Our approach combines automation, payer-specific expertise, and seamless RCM integration to accelerate approvals, reduce denials, and protect cash flow.
Automated Submission Tracking
Every authorization request is tracked in real time, with built-in checks for missing documentation or payer-specific requirements. This reduces first-pass errors and ensures compliance from the start.
Payer-Specific Rules Engine
Instead of one-size-fits-all workflows, Pro-MBS applies payer-specific logic to each request. This customization minimizes denials, shortens approval timelines, and improves first-pass acceptance rates.
Certified Authorization Specialists
Our team of credentialed billers, coders, and authorization experts manage requests end-to-end. They stay current with the latest payer policy updates, preventing costly rework and compliance issues.
Seamless EHR and RCM Integration
Pro-MBS integrates directly with existing EHR and billing platforms, eliminating duplicate data entry and reducing staff workload. This ensures that authorizations flow smoothly into the revenue cycle without disruption.
By combining technology, compliance expertise, and operational efficiency, Pro-MBS enables providers to transform prior authorization from a revenue bottleneck into a streamlined, predictable process.