Multi-Specialty Billing Workflows keep complex medical practices running smoothly. When several specialties share one billing team, things can get messy fast. Each department follows its own coding and documentation rules, and one small mistake can delay payments. A clear, standardized process keeps everyone on track. It improves accuracy, reduces denials, and supports a healthy revenue cycle. Backed by CMS and AMA guidelines, these workflows help every team bill correctly and consistently.
But here’s the real question: how do you create one process that fits so many different specialties? What keeps billing efficient when cardiology, orthopedics, and radiology each have their own way of working?
In busy practices, even a small delay can affect revenue. That’s why consistency matters. When workflows are aligned, billing feels less like a daily struggle and more like a steady, well-run system that supports your entire organization.
Mapping the Multi-Specialty Revenue Cycle: From Intake to Payment
Before you can fix a billing process, you need to know exactly where it breaks. That’s why mapping the entire revenue cycle is such an important first step in managing multi-Specialty Billing Workflows. It helps you see how information moves from the first patient call to the final payment post. When every step connects without gaps, billing runs faster, cleaner, and with fewer surprises.
A shared workflow also gives your team a clear view of what’s happening at each stage. Front-desk staff can verify patient data before the visit. Coders can double-check documentation right after encounters. Billers can track claims in real time and catch denials before they snowball. This kind of transparency makes it easier to find and fix problems early, instead of chasing them after the fact.
According to HFMA, practices that use unified billing processes can shorten their payment cycle by nearly 30 percent. That means less time waiting for reimbursements and more predictable cash flow. When every department follows the same path, your revenue cycle stops being a mystery and starts becoming a reliable, measurable process.
The Core Stages of a Multi-Specialty Billing Cycle
- Patient Intake & Eligibility: Verify insurance before the visit to prevent rejected claims.
- Charge Capture & Coding: Use the same charge entry rules across departments.
- Claim Submission: Automate claim checks for each specialty’s coding needs.
- Denials Management: Track denial trends and correct the real causes early.
- Payment Posting & Reporting: Combine reports for a full view of financial health.
Identifying Specialty-Specific Billing Challenges and How to Fix Them
Every specialty has its own quirks. Cardiology, orthopedics, and neurology all handle billing differently. One may deal with more prior authorizations, another with complex coding. These differences create daily challenges for billing teams.
Multi-Specialty Billing Workflows need to handle these differences in a way that keeps everything organized and efficient. Each specialty has its own coding rules, payer requirements, and documentation habits, but they all have to feed into one coordinated system. The best approach is to create a shared process that adapts to each specialty’s needs without breaking the overall structure. This balance keeps billing consistent while still giving every department the flexibility it requires to work accurately and stay compliant.
Common Specialty Billing Challenges
Each specialty brings its own set of hurdles that can slow down billing and affect cash flow. Understanding these unique challenges is the first step toward building stronger multi-Specialty Billing Workflows.
The table below highlights some of the most common issues and the best ways to handle them.
| Specialty | Main Billing Issue | Best Practice Fix |
|---|---|---|
| Orthopedics | Multiple modifiers and surgical package rules | Use automated modifier checks from AMA CPT guidance |
| Cardiology | Frequent testing authorizations | Add preauthorization steps aligned with CMS rules |
| Neurology | Complex diagnostic coding | Use AI-driven coding validation before submission |
| Oncology | Global billing for chemo and infusion | Add configurable workflows within your RCM system |
| Radiology | Split billing for technical and professional work | Sync charge capture directly through the EHR |
How to Make It Work?
Once you identify the problem areas, the next step is to build a strong structure that keeps everything running efficiently. This means setting clear rules, defining who is responsible for what, and using tools that support accuracy and speed. When each department follows the same foundation, your Multi-Specialty Billing Workflows become more predictable, consistent, and easier to manage. Small, steady habits like clear documentation, regular training, and open communication can completely change how smoothly your billing process operates.
Here are a few simple ways to strengthen your structure and keep your multi-Specialty Billing running smoothly every day.
- Keep a central compliance library that stores the latest AMA and CMS updates. This gives billers and coders one trusted source for all coding, modifier, and documentation rules, reducing confusion and mistakes.
- Use smart tools and automation to spot coding or data errors before claims are sent. Early detection saves hours of rework and helps maintain cleaner claim submissions across every specialty.
- Encourage open communication between billing and clinical teams. When information flows freely, documentation improves, and issues get resolved before they reach the payer.
Designing Standardized Workflows That Still Allow Specialty Flexibility
A standardized process should never feel rigid or forced. The goal isn’t to make every specialty work in the exact same way. It’s to build a structured system that keeps billing consistent while still leaving room for flexibility. Think of it like a simple template you can adjust. The main steps such as verifying insurance, checking codes, and reviewing claims stay the same across the board. What changes are the smaller details that fit each specialty’s workflow, like pre-authorization checks, extra documentation, or payer-specific coding rules. This balance keeps billing organized, accurate, and easy to manage without slowing anyone down.
Start by setting the basics that never change: verifying coverage, checking documentation, and confirming coding accuracy. Then add optional steps for each department’s unique billing flow.
Shared Workflow Foundation
Every team should follow the same checkpoints for charge entry, claim validation, and denial follow-up. These shared steps create a common rhythm that keeps Multi-Specialty Billing Workflows consistent and easy to manage. When everyone uses the same structure, it’s simpler to spot errors, maintain compliance, and complete audits without confusion.
Specialty Add-Ons
Some specialties, like oncology or radiology, may need a few extra steps such as prior authorization or treatment plan review. These steps should connect smoothly with the main workflow instead of sitting apart from it. This flexibility keeps standardizing billing workflows for Multi-Specialty practices practical and adaptable while still respecting each department’s unique needs.
Ongoing Oversight
Every workflow needs someone responsible for keeping it current. Assign a few workflow owners to monitor CMS updates, track payer policy changes, and train staff on new rules. Regular reviews help maintain Multi-Specialty medical billing best practices and prevent compliance issues before they start.
Leveraging Technology and Automation to Keep Billing Consistent
Technology makes standardization easier. Modern RCM platforms can automate many parts of multi-Specialty Billing Workflows, saving time and cutting errors. When billing software connects to your EHR, charge capture becomes seamless. Smart rules engines can alert staff to missing data or invalid codes before claims are sent. Automation tools also help track denials and provide reports in real time.
Using RPA (robotic process automation) or AI-driven coding review tools can reduce manual work. It ensures staff spend more time solving issues rather than chasing them. These tools also help maintain CMS billing compliance across specialties.
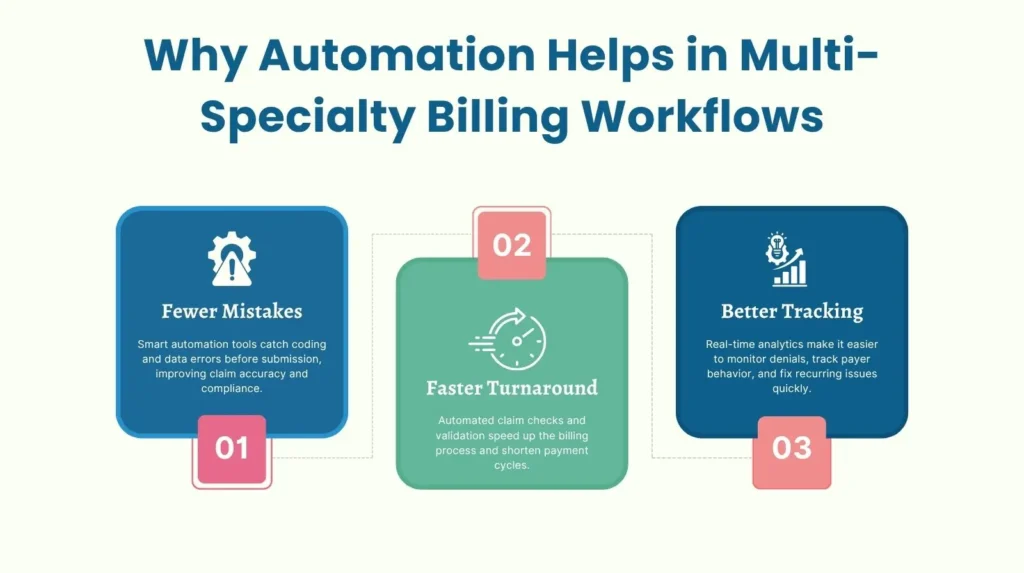
Why Automation Helps
Automation makes billing faster, cleaner, and easier to track. The points below highlight how technology improves Multi-Specialty Billing Workflows at every stage.
Training, Governance and Change Management for Workflow Adoption
Even the best billing systems can fail if people don’t know how to use them. That’s why strong training and governance are the foundation of effective Multi-Specialty Billing Workflows. Every team member, from new hires to experienced billers, needs to understand the process and follow it the same way. When everyone works from one clear playbook, billing becomes faster, cleaner, and easier to manage.
Start by creating a detailed onboarding plan that covers your entire revenue cycle process. Make sure new staff learn not just how tasks are done, but why they matter. Then, build consistency through regular audits and quarterly refresher sessions. A dedicated governance team made up of coding specialists, compliance officers, and RCM managers should meet often to review processes, evaluate compliance, and share updates from CMS or AMA.
Change management is just as important as training. When new tools or automation systems are introduced, explain the reason behind the change and how it helps daily workflows. Encourage questions and feedback to build trust and engagement. According to HFMA, organizations that invest in structured staff education see up to 25 percent fewer denials. That’s a powerful reminder that the right training doesn’t just improve accuracy; it directly strengthens your bottom line.
Simple Adoption Steps
To make sure your Multi-Specialty Billing Workflows run efficiently, it helps to keep the adoption process simple and repeatable. The steps below show how to build consistency and accountability across every team.

Measuring Success: KPIs, Improvement and Growth
You can’t manage what you don’t measure. That’s why tracking performance is crucial in Multi-Specialty Billing Workflows. Data helps you find weak spots, spot delays, and prove the value of your improvements. Keep an eye on denial rates, days in accounts receivable (AR), and clean claim percentages. Watch how long it takes for claims to get paid. These numbers tell the story of how well your billing operation runs.
Performance Measures to watch
To keep your Multi-Specialty billing Workflows running efficiently, it’s important to track a few key performance measures that reveal how well your billing process is working.
- Clean Claim Rate: How many claims go through without edits.
- Denial Rate: How often payers reject claims.
- AR Days: How long it takes to collect payments.
- First-Pass Resolution Rate: The share of claims paid on the first try.
- Team Productivity: Average claims processed per biller each day.
Over time, use these insights to refine the process. Continuous monitoring and adjustment help practices grow smoothly while keeping their billing tight and compliant.
Let Pro-MBS Handle Your Billing Workflows
Managing Multi-Specialty Billing Workflows takes more than technology. It requires structure, expertise, and a partner who understands how each specialty operates. Pro-MBS helps healthcare organizations create streamlined billing systems that improve accuracy, reduce denials, and keep every department aligned with CMS and AMA standards.
Our team offers specialized support through RCM Optimization and Workflow Automation Services. We identify process gaps, strengthen charge capture, and introduce automation tools that make billing faster and cleaner across all specialties. With Pro-MBS, your workflows become simpler, your revenue more predictable, and your staff better equipped to focus on patient care instead of paperwork.
Frequently Asked Questions
What does Multi-Specialty mean?
Multi-Specialty means power through unity. Different disciplines. One heartbeat. Cardiology, Orthopedics, and Radiology. Each speaks its own language, yet they move under one Billing Workflow. It is order built from chaos. Aligned, compliant, and precise under CMS and AMA guidance.
At Pro-MBS, we bring this unity to life. Our structured workflows keep every specialty aligned, compliant, and ready for clean claims.
What is Multi-Specialty Coding?
Multi-Specialty Coding is discipline in motion. One framework. Many specialties. Coders walk the same line. Clean entries. Flawless modifiers. No wasted steps. Each code follows CMS and AMA rules like runes carved in stone. The result is accuracy that does not break. Compliance that never sleeps.
At Pro-MBS, our coders master the art of multi-specialty coding. Every claim that leaves our system stands strong against payer scrutiny.
What do you mean by Multi-Specialist?
A Multi-Specialist group is no random gathering. It is a crafted alliance of many minds with one mission. Each specialty fights its own battles, yet the Billing Workflow unites them. Documentation tight. Claims clean. Errors caught before they can breathe.
Pro-MBS builds that unity. We connect every department through one consistent workflow that keeps claims moving without friction.
What are Examples of Specialty Services?
Orthopedics. Cardiology. Neurology. Oncology. Radiology. Each one complex. Demanding. Each one alive with unique coding rituals and payer rules. But within a Multi-Specialty Billing Workflow, they follow one rhythm. Clean claims. Faster payments. No lost motion.
With Pro-MBS, every specialty finds its rhythm. We align diverse workflows into one seamless revenue cycle that never misses a beat.
Is Multispecialty one word?
Yes. One word. One idea. Multispecialty means unity in structure. Departments moving together under one RCM Workflow. No fragmentation. No confusion. Just precision forged through alignment.
Pro-MBS specializes in building that structure. We make multispecialty billing simple, scalable, and perfectly synchronized.
What is the difference between Multi-Specialty and Super-Specialty hospitals?
A Multi-Specialty Hospital spreads wide with many disciplines under one workflow. A Super-Specialty Hospital dives deep into one field with unmatched mastery. Both demand structure. But only a unified Billing Workflow keeps their rhythm steady when payers tighten the reins.
Pro-MBS ensures that rhythm never breaks. Whether wide or deep, our systems keep billing precise, compliant, and fast.
What is a Multi-Specialty Practice Setting?
A Multi-Specialty Practice Setting is a living system. Different departments breathe through one Billing Workflow. Front-desk, coders, and billers move in sync. Accuracy sharpens. Denials fall. The revenue cycle hums like a well-tuned blade.
At Pro-MBS, we make that hum stronger. We design workflows that bring calm to chaos, clarity to claims, and growth to your practice.