Introduction
What You’ll Learn in This Guide
This comprehensive guide is designed for healthcare providers, administrators, billing professionals, and practice managers navigating credentialing workflows. You’ll gain insight into:
- The five major types of credentialing in U.S. healthcare (insurance, hospital, board, facility, and telehealth)
- How each credentialing type affects billing, compliance, and care delivery
- Required documentation and review timelines
- Common credentialing mistakes that result in denials or delays
- The role of recredentialing and monitoring for ongoing compliance
- How credentialing integrates with payer systems like CAQH, PECOS, and NPPES
What Is Credentialing in Healthcare?
Credentialing is a formal verification process used to validate a healthcare provider’s professional qualifications, including education, training, board certification, licensure, work history, and malpractice coverage. It is required for:
- Provider enrollment with payers (insurance credentialing)
- Hospital access and clinical privileging
- Legal licensure through state medical boards
- Group and facility-level payer approvals
Credentialing ensures a provider meets the standards of competence and ethical conduct established by medical boards, insurance companies, and regulatory agencies. A lapse in credentialing can trigger claim denials, disrupt patient care, and put an organization at risk for audits and penalties.
Why Credentialing Is Essential
Credentialing plays a pivotal role in every stage of the revenue cycle. It directly affects:
- Payer Reimbursement: Insurance companies will not pay claims from uncredentialed or improperly enrolled providers.
- Hospital Access: Medical staff offices use credentialing to grant (or deny) clinical privileges.
- Compliance: Credentialing ensures a provider is legally eligible to practice under state and federal regulations.
- Provider Reputation: Credentialing protects patients by confirming that a provider meets current standards of care.
Credentialing delays, gaps, or inaccuracies can result in:
- Claim denials and delays
- Loss of hospital privileges
- Legal and financial penalties
- Network removal or payer sanctions
The Five Primary Types of Credentialing in U.S. Healthcare
1. Insurance Credentialing (Payer Enrollment)
Insurance credentialing is the process of becoming an approved provider with insurance payers such as Medicare, Medicaid, and commercial plans like BCBS, Aetna, Cigna, and UnitedHealthcare.
Typical Requirements:
- Active state license and NPI registration
- Malpractice insurance
- Education and residency verification
- Work history with gap explanations
- No disciplinary or legal issues
Credentialing Tools: CAQH ProView (commercial), PECOS (Medicare), and state-specific portals. Without payer enrollment, providers are considered out-of-network and will not receive direct reimbursements.
2. Hospital Privileging and Credentialing
Hospital credentialing is a comprehensive review conducted by the Medical Staff Office and credentials committee. It grants clinical privileges based on a provider’s qualifications and scope of practice. Includes:
- Medical school transcripts
- Board certification validation
- Procedure logs and case studies
- Peer references
- NPDB (National Practitioner Data Bank) query
Credentialing cycles may occur every 2–3 years and are mandatory for continued hospital access. Many surgical and procedural-based specialties require facility-specific privileging in addition to payer credentialing.
3. State Medical Board Credentialing
All clinical providers must be credentialed and licensed through the medical board in each state they practice. This foundational credentialing process includes:
- State-specific license applications and renewals
- Fingerprinting and background checks
- Primary source verification (PSV) of education and training
- Examination history (USMLE, COMLEX, NBME)
- CME (Continuing Medical Education) documentation
Medical board credentialing must be renewed periodically, typically every 1 to 3 years depending on the state.
4. Facility Credentialing
Facility credentialing is often necessary for Medicaid group enrollment and Commercial group TIN/NPI credentialing. For group practices, behavioral health clinics, and ambulatory surgical centers (ASCs), credentialing also applies at the facility level.
Facility Credentialing Verifies:
- Site compliance with OSHA and HIPAA regulations
- Liability insurance coverage
- Fire and safety inspections
- Ownership and leadership structure
Facility credentialing is required to obtain a group NPI and bill under that entity.
5. Telehealth Credentialing
Telehealth credentialing has become increasingly critical in the post-pandemic landscape.
Key Requirements:
- Proof of HIPAA-compliant telehealth platforms
- Multistate licenses for interstate patient care
- Documentation of telehealth training (as required by some payers)
- POS code 02 or 10 and modifier -95 for claims
States participating in the Interstate Medical Licensure Compact (IMLC) make multistate credentialing easier.
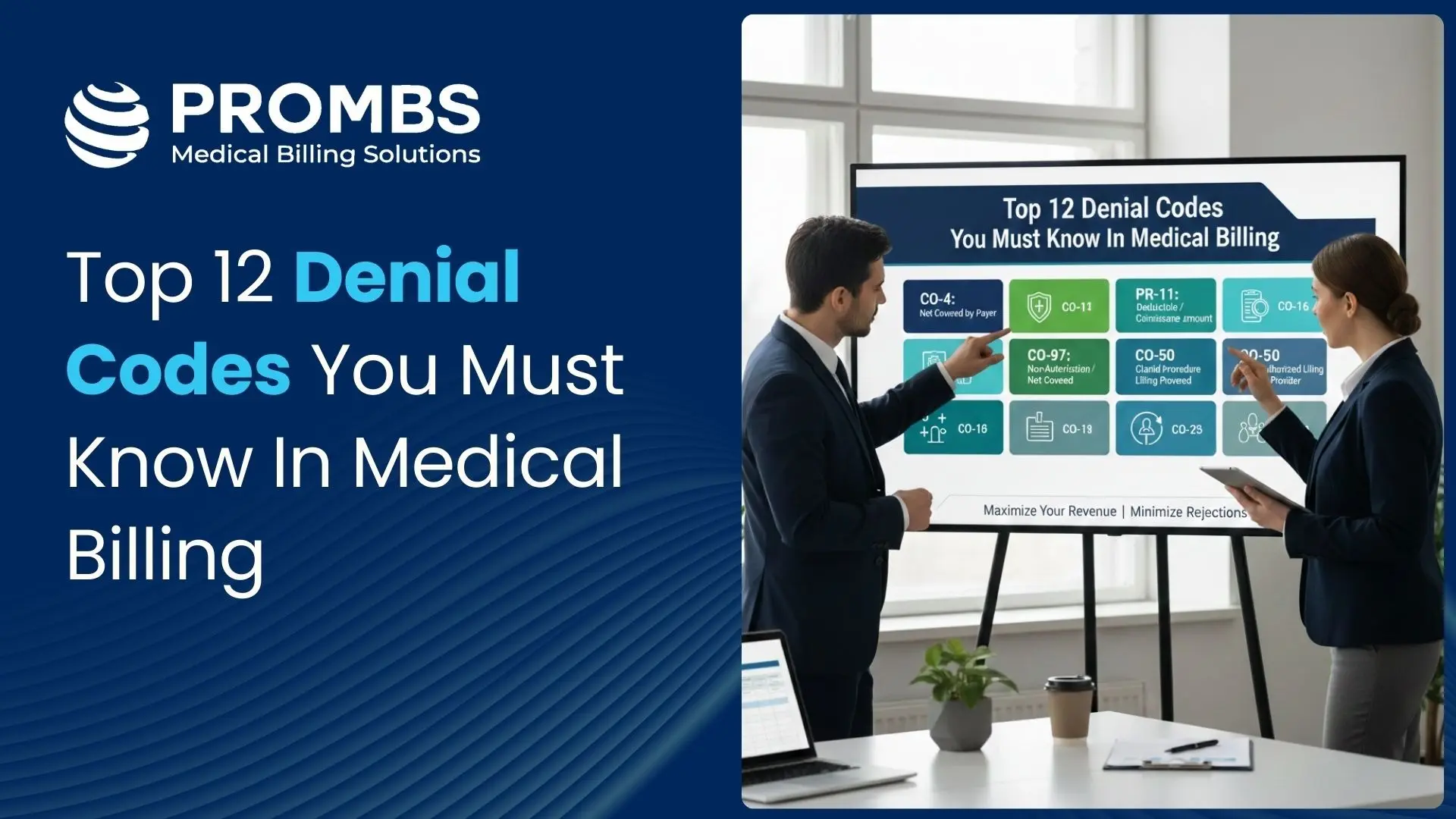
Common Credentialing Mistakes and Their Consequences
| Mistake | Consequence |
|---|---|
| Incomplete applications | Delayed approval, payer rejections |
| Missed recredentialing | Deactivation from insurance panels |
| Outdated license/NPI info | Denials, legal exposure, claim recoupments |
| Lack of documentation | Hospital privileges delayed or denied |
| Not monitoring expiring documents | Results in lapse of billing eligibility and auto-deactivation by payers |
Recredentialing Frequency by Payer Type
| Payer / Entity | Recredentialing Cycle | Notes |
|---|---|---|
| Commercial Insurance (e.g., Aetna, Cigna, BCBS) | Every 2–3 years | Typically managed through CAQH; automatic reminders sent if opted in. |
| Medicare (PECOS) | Every 5 years | Revalidation required by CMS; check PECOS for revalidation due dates. |
| Medicaid (State-specific) | Every 3–5 years | Varies by state; some states require annual updates for managed care. |
| Hospitals / Medical Staff Offices | Every 2 years | Includes peer review, clinical performance, and privilege renewals. |
| State Medical Boards | 1–3 years (license renewal) | Includes CME verification and fingerprint/background updates. |
| Facility Credentialing (Groups, ASCs, Clinics) | Every 2–3 years | Requires site inspection updates, compliance reports, and insurance docs. |
| Telehealth Credentialing | Aligned with state/facility | Reverify tech compliance, multistate licensure, and payer-specific rules. |
How PROMBS Simplifies the Credentialing Lifecycle
Our credentialing team is equipped to handle high-volume enrollments, revalidations, and multistate requirements. Our services include:
- Full-service application preparation and submission
- Credentialing for individuals, facilities, and multi-site networks
- Continuous monitoring for recredentialing and license expiration
- Support for CAQH, PECOS, NPPES, and commercial portals
- Credentialing audits and documentation workflows
Whether you're a solo provider or multi-location group, Pro-MBS ensures clean, timely, and audit-ready credentialing workflows.