Accurate and timely claim processing is essential for the financial stability of healthcare facilities. For institutional providers, the UB-04 claim form also referred to as the CMS-1450 is the standardized billing tool for submitting inpatient and outpatient claims to Medicare, Medicaid, commercial insurance payers, and other government programs.
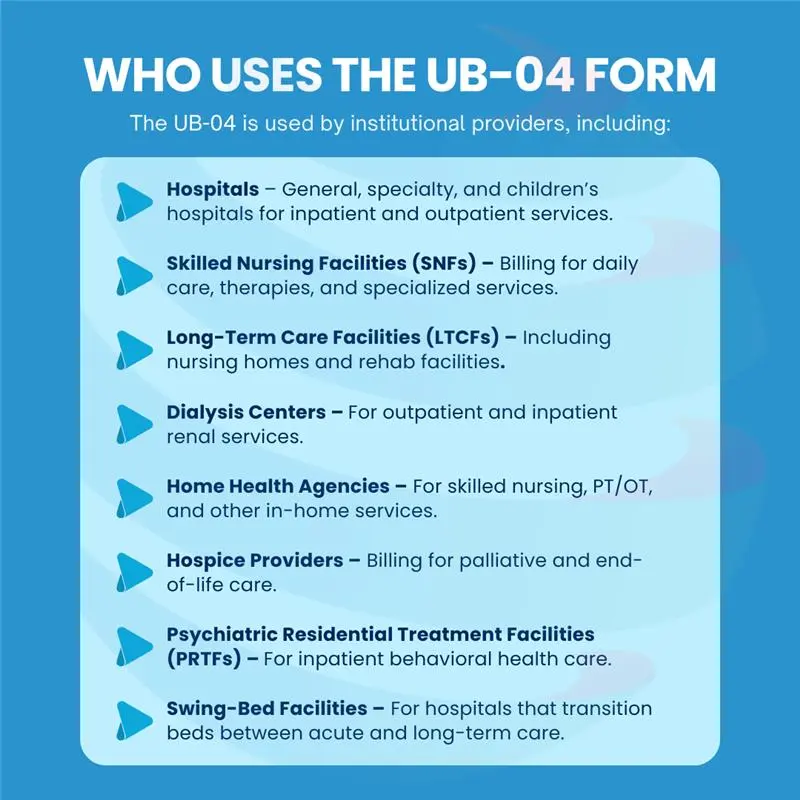
Used by hospitals, nursing homes, rehab centers, hospices, and other institutional facilities, the UB-04 is not just an administrative form, it is a compliance-driven, data-rich document that directly impacts reimbursement, audit readiness, and operational efficiency.
Submitting incomplete, inaccurate, or fraudulent data on the UB-04 can result in severe penalties, including fines, criminal charges, and long-term reputational damage. That’s why healthcare providers must fully understand its structure, purpose, and compliance requirements.
About the UB-04 Claim Form
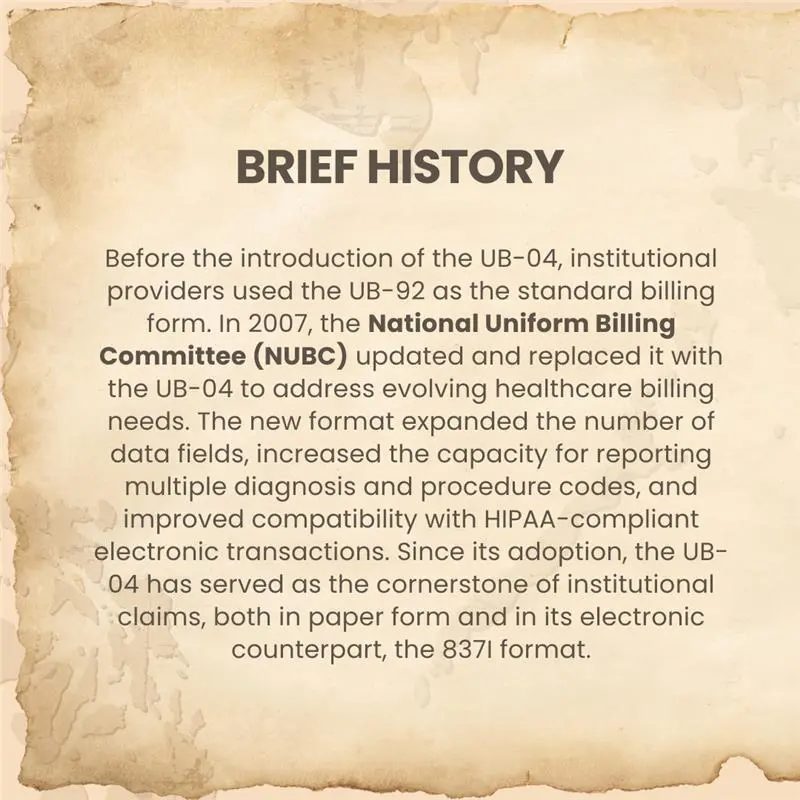
The UB-04, also known as the CMS-1450, is the standardized paper claim form used by institutional healthcare providers to submit facility-based inpatient and outpatient claims for reimbursement. While most providers submit electronically through the 837I format, the UB-04 is required when a facility has an Administrative Simplification Compliance Act (ASCA) waiver or when a payer specifically requests paper claims.
This form captures detailed billing data including patient demographics, provider identifiers, service dates, diagnosis and procedure codes, revenue codes, and total charges in a format recognized by Medicare, Medicaid, and most commercial insurers.
Key Facts About the UB-04 Claim Form:
- Regulated by the National Uniform Billing Committee (NUBC): The NUBC develops and maintains the UB-04 format to ensure national consistency, payer compliance, and compatibility with HIPAA transaction standards.
- Primary Purpose: Serves as the official record of all billable care provided to a patient during a facility stay or visit, enabling accurate reimbursement from Medicare, Medicaid, and other payers.
- High Adoption Rate: According to Streamline Health, the UB04 form is used in more than 98% of Medicare claims and over 80% of all institutional claims.
- Designed for Institutional Billing: Commonly used by hospitals, skilled nursing facilities, rural health clinics, rehabilitation centers, hospices, and other large-scale care facilities.
- Includes NPI Data Fields: Contains specific Form Locators for National Provider Identifier (NPI) entry, ensuring accurate provider identification and streamlined communication with payers. For example, FL-56 captures the billing provider’s NPI, while FL-76 through FL-79 capture NPIs for attending, operating, and other relevant providers.
Importance of the UB-04 Form
1. Standardized Communication Between Providers and Payers
In healthcare billing, one of the biggest challenges is ensuring that payers whether Medicare, Medicaid, or commercial insurers clearly understand what services were provided, why they were necessary, and how they should be reimbursed. Without a consistent format, each provider might present information differently, leading to confusion and processing delays.
The UB-04 addresses this by providing a nationally standardized claim format. It uses ICD-10-CM codes for diagnoses and applies ICD-10-PCS codes for inpatient procedures, while CPT/HCPCS codes are used for outpatient and ancillary services. All codes are aligned with the appropriate revenue codes to ensure payer accuracy. This structured approach removes ambiguity, allowing payers to process claims faster and more accurately.
2. Ensures Accurate and Complete Reimbursement
Healthcare facilities provide a wide range of services during a single patient encounter room and board, diagnostic imaging, surgeries, medications, and more. If these services aren’t captured and billed accurately, the facility risks significant revenue loss.
The UB-04 ensures that every reimbursable service is itemized and clearly linked to the patient’s stay or visit. This prevents underpayments by making sure no services such as lab tests, specialized therapies, or ancillary procedures are missed in the billing process.
3. Reduces Claim Denials and Delays
A large portion of claim denials can be traced to missing or incorrect claim data. Payers require specific details such as patient demographics, revenue codes, and service dates to validate a claim. If these are absent or formatted incorrectly, the claim may be rejected or delayed for corrections.
The UB-04 reduces this risk by using Form Locators to ensure all necessary data fields are completed consistently. When filled out correctly, it improves first-pass acceptance rates and minimizes back-and-forth between providers and payers.
4. Supports Compliance and Audit Readiness
The UB-04 is more than just a billing form, it serves as a legal record of the care provided. Medicare, Medicaid, and commercial insurers require strict adherence to coding and billing regulations. An accurately completed UB-04 demonstrates compliance with these requirements.
In the event of an audit, a clean UB-04 provides auditors with a clear, organized summary of the patient’s care, directly tied to the supporting clinical documentation. This can protect providers from penalties, repayment demands, or allegations of improper billing.
5. Facilitates Multi-Provider Care Coordination
In an institutional setting, patient care often involves multiple providers and departments surgeons, anesthesiologists, therapists, radiology staff, and others. The UB-04 allows all these services to be recorded and linked in a single claim, ensuring nothing is overlooked.
This is especially valuable in bundled payment models, where one payment covers an entire episode of care. The UB-04 ensures accurate attribution of services, fair payment distribution among providers, and improved coordination across departments.
Where is the UB-04 Claim Form Used?
The UB-04 form is a universal billing tool for institutional healthcare claims and is accepted by virtually all payer types in the United States. Its use is not limited to Medicare and Medicaid many private and government-funded programs require UB-04 for claim submission.
1. Commercial Insurance Companies
Private health insurers use the UB-04 to process claims for facility-based services rendered to their members. Because commercial plans vary in their reimbursement rules, the standardized format ensures consistent data submission regardless of payer-specific requirements.
Example: A large commercial payer may require specific condition codes for same-day surgeries. The UB-04 allows the provider to include these codes in designated Form Locators for faster adjudication.
2. Medicare and Medicaid
Medicare (Part A) and state Medicaid programs rely heavily on the UB-04 for institutional claims. This includes acute hospital care, skilled nursing stays, rehabilitation, and hospice care.
Note: Medicare requires the UB-04 for inpatient services, while Medicaid often mandates it for both inpatient and outpatient facility claims.
2. Medicare and Medicaid
Medicare (Part A) and state Medicaid programs rely heavily on the UB-04 for institutional claims. This includes acute hospital care, skilled nursing stays, rehabilitation, and hospice care.
Note: Medicare requires the UB-04 for inpatient services, while Medicaid often mandates it for both inpatient and outpatient facility claims.
4. Workers’ Compensation Programs
For workplace injuries requiring hospital stays, surgeries, or rehab, the UB-04 is used to bill state workers’ comp programs. These claims often require precise occurrence and accident codes to align with injury reports.
5. Self-Pay Patients
Even for uninsured patients, facilities may use the UB-04 to generate a formal bill. This ensures the patient receives a comprehensive, itemized statement in a standardized format helpful for payment plans, legal documentation, or reimbursement from supplemental coverage.
UB-04 Structure: Understanding Form Locators (FLs)
| FL | Field | Details | Inpatient | Outpatient |
|---|---|---|---|---|
| 1 | Provider Name & Address | Must match NPI in FL56 | Required | Required |
| 4 | Type of Bill Code | 3-digit code identifying facility type, care type, and sequence | Required | Required |
| 6 | Statement Covers Period | Start/end dates of care | Required | Required |
| 42 | Revenue Codes | Categorize services (e.g., 0100–0219 for room/board) | Required | Required |
| 67–75 | Diagnosis Codes | ICD-10-CM and ICD-10-PCS | Required | Required |
| 76–79 | Provider Identifiers | NPI and credentials for attending/operating providers | Required | Required |

Paper vs. Electronic UB-04 Submission
Paper CMS-1450 (UB-04) is permitted when CMS allows paper typically via an ASCA waiver otherwise, the HIPAA-compliant 837I is the standard.
Paper UB-04 (CMS-1450)
It is primarily used when a provider has an Administrative Simplification Compliance Act (ASCA) waiver, which exempts them from the requirement to submit claims electronically. An ASCA waiver is typically granted to small-volume providers, facilities in rural areas with limited internet access, or situations where electronic claim submission is technically infeasible. Providers seeking paper submission must request an ASCA waiver from their Medicare Administrative Contractor (MAC), and most institutional providers are expected to file electronically whenever possible.
Some payers also still allow or in rare cases require paper submission for certain claim types, such as adjustment claims, corrected claims, or special program claims where electronic formats cannot accommodate all required data. However, paper claims generally have longer processing times, are more prone to manual entry errors during payer intake, and often require more follow-up to resolve issues. For this reason, paper UB-04 use is limited and declining.
Electronic UB-04 Equivalent (837I Transaction)
The electronic version of the UB-04 is submitted using the 837I transaction format, which follows HIPAA-compliant Electronic Data Interchange (EDI) standards. The 837I contains the same core data elements as the paper UB-04 but is transmitted electronically to payers through direct connections, clearinghouses, or integrated EHR/RCM platforms.
Electronic submission is the preferred method for nearly all payers because it offers significant advantages:
- Faster Processing: Claims are received instantly, bypassing postal delays.
- Fewer Errors: Built-in edits and claim scrubbers can catch missing or invalid data before submission.
- Better Tracking: Submission confirmations and payer acknowledgments are sent electronically, reducing uncertainty.
- Integration with Technology: Electronic submission allows seamless communication between the provider’s Electronic Health Record (EHR) system, billing software, and payer systems.
Because of these benefits, most large facilities and high-volume institutional providers rely exclusively on the 837I format, using paper UB-04s only for exceptions or when required by payer policy.
Conclusion
The UB-04 claim form remains the foundation of institutional medical billing in the United States, bridging the gap between patient care delivery and accurate financial reimbursement. Its standardized design ensures that complex inpatient and outpatient service data is communicated clearly to Medicare, Medicaid, commercial insurers, and other payers, reducing ambiguity, streamlining processing, and supporting timely payments.
For institutional providers from hospitals and skilled nursing facilities to rehabilitation centers and hospices mastering UB-04 completion is not simply an administrative skill, but a critical component of revenue cycle management. By understanding its structure, knowing where and when it’s required, applying best practices, and adhering to NUBC and CMS guidelines, providers can minimize denials, maintain compliance, and safeguard revenue integrity.
In an era of increasing regulatory scrutiny and evolving payer requirements, the ability to submit accurate, compliant UB-04 claims whether on paper under an ASCA waiver or electronically via the 837I format directly impacts a facility’s cash flow and operational stability. Continuous training, proactive error prevention, and the use of technology-driven claim validation tools can ensure that the UB-04 continues to serve as a reliable, compliant, and efficient billing instrument for years to come.