CPT 99396. One code. A hundred mistakes are waiting for happening. Ever wonder why preventive visits spark so much confusion? What’s the right way to bill them? How do you keep payers from kicking claims back?
You’re not alone. Many providers trip over this one, even seasoned billers. This guide breaks it down, plain, direct, and usable. You’ll see how CPT 99396 works, what to document, and how to link ICD-10 codes the smart way. No fluff. Just the truth from AMA, CMS, and field experience that keeps practices compliant and paid.
What Is CPT 99396 and When to Use It
Let’s start simple. CPT 99396 covers a preventive medicine visit for an established patient aged 40–64. Not a sick visit. Not a follow-up. A full preventive exam with history, exam, and counseling. Think of it as a health check, not a problem-solver. The patient feels fine, but you’re checking everything that keeps them that way.
So, what’s included?
- A comprehensive history that includes lifestyle, family, social, and risk factors.
- A full exam that’s age-appropriate, head to toe.
- Preventive counseling on diet, exercise, screenings, and habits.
If the patient mentions something new like back pain, fatigue, or a rash, that’s a separate problem-oriented service. Bill it with the right E/M code and add modifier 25. That’s straight from AMA guidance.
CPT 99396 Across Different Specialties
Every specialty views prevention through its own lens. But CPT 99396 keeps the same rule for all. The goal is simple: see the whole person, not just the symptom.
Family Medicine / Internal Medicine
The annual physical. The foundation of primary care. You check vitals, labs, lifestyle, and risk. You talk about habits, not just history. You plan, not react. This is where 99396 feels most natural. It is the rhythm of preventive care, steady, consistent, and personal. One visit can reset an entire year of health. And when coded right, it keeps your claims clean and your compliance solid.
Obstetrics and Gynecology
Prevention in women’s health tells its own story. The well-woman exam is more than a checkup. It is reassurance, education, and early protection. CPT 99396 fits perfectly. Remember, the Pap test or pelvic exam stands alone and should be billed separately if performed. This visit is about talking through what comes next such as birth control, menopause, screenings, or lifestyle changes. The goal is to anticipate, not chase. Document the counseling clearly. Preventive intent keeps your reimbursement secure.
Behavioral Health / Integrated Clinics
Prevention does not stop with blood pressure and labs. More clinics now merge physical and mental health, and that is where CPT 99396 truly proves its flexibility. A visit might include depression screening, anxiety discussion, or lifestyle stressors along with cholesterol checks and BMI. That is still prevention. The AMA recognizes integrated care as part of total wellness. If your team provides full-body and mind screening, this code fits. It shows payers you are not treating illness; you are preventing it.
Multi-Specialty Groups
Did You Know?
According to AMA, nearly four out of ten denied preventive claims fail because of missing or weak documentation. A line left blank. A code linked wrong. A note typed too fast. Small things that cost big money. A few extra seconds of detail can mean the difference between fast payment and a rejected claim.
Documentation Requirements for CPT 99396
What’s the best defense against denials? Solid notes. No guesswork. No gaps. Just clear, complete documentation. Auditors from CMS do not look for fancy words. They look for proof. Proof that the visit met every preventive requirement. Proof that the care you billed was actually delivered.
Three things matter every single time:
- Comprehensive History: Document lifestyle, risks, family, and social habits.
- Comprehensive Exam: Record findings appropriate to age and gender.
- Preventive Counseling: Address habits, diet, exercise, substance use, and mental health.
Time doesn’t decide this code. Content does. You could spend 20 minutes or 60. What matters is what’s documented. Make it clear and complete. Add anticipatory guidance, that forward-looking education piece payers expect. Without it, you risk downcoding even when the care was excellent.
ICD-10 Codes Commonly Linked with CPT 99396
How do you tell the payer this visit was preventive? With the right ICD-10 code. That is your signal. Your proof. Your protection. A single wrong code can flip the meaning of a claim. It can turn prevention into treatment. It can turn payment into denial. That is why choosing the right code is not a clerical step. It is strategy. Z-codes are your allies here. They tell payers, “This visit was about prevention, not disease.” Each one carries intent, and intent is what keeps the claim clean.
So, what does that look like in real coding? Here is a quick reference you can keep at your desk:
| Purpose of Visit | ICD-10 Code |
|---|---|
| General adult exam, no complaint | Z00.00 |
| Encounter with abnormal findings | Z00.01 |
| Screening for depression | Z13.89 |
| Lipid disorder screening | Z13.220 |
| Diabetes screening | Z13.1 |
Always choose Z-codes to reflect preventive intent. Pairing 99396 with a chronic diagnosis like hypertension flips the claim from preventive to problem-oriented. That single mismatch is one of the most common denial triggers reported by CMS. Your code tells the story. Write that story right. Show intent, show purpose, show prevention. When you choose correctly, the claim passes. The patient is covered. The work gets paid. That is clean coding, and it starts with the right ICD-10.
Common Coding Errors and Denial Triggers
Let’s be honest. Everyone slips up on preventive coding now and then. But some mistakes happen again and again. They sneak in quietly. A missed modifier. A wrong code. A rushed note. And suddenly, a clean claim turns into a denial you have to chase down later. Why does it happen? Because preventive coding feels simple. It looks easy on paper. But the rules are sharp, and payers read every detail. Even one mismatch between CPT 99396 and an ICD-10 code can change the entire claim story.
You think you billed for prevention. The payer thinks you treated a problem. You think it is covered. The payer flags it as non-preventive. That is how rejections start. That is how revenue leaks out of good clinics every single day. So what are the mistakes that repeat the most? Let’s call them out clearly.
- Billing CPT 99396 for chronic condition follow-ups instead of true preventive visits.
- Forgetting to link a proper Z-code to show preventive intent.
- Leaving out counseling or education notes that prove prevention was discussed.
- Skipping modifier 25 when a problem-oriented visit happens on the same day.
- Billing routine labs but failing to connect them to the preventive diagnosis.
Each one seems small until it stacks up. Denials rise. Audits follow. Time gets wasted fixing claims that could have been clean from the start. The solution is not complicated. Slow down. Review templates. Train your team. Have coders and providers look at the same documentation together. When everyone sees prevention the same way, your numbers improve fast. Clean documentation protects more than money. It protects trust. It shows CMS and payers that your coding matches your care. Every visit tells a story. Make sure yours reads clearly from start to finish.
Reimbursement Guidelines and Payer Nuances
What’s the reimbursement rule for CPT 99396? It sounds simple, but it never is. Most commercial payers cover one preventive visit every 12 months, yet even that rule bends from plan to plan. Some count by calendar year. Others count exactly 365 days from the last service date. Miss that detail, and a clean claim turns into a denial. Here is where it gets tricky. Each payer writes its own preventive policy. Some allow flexibility. Others are strict. A few even require patients to reach a full year before the next covered visit, not one day sooner.
Medicare follows a different path. It does not recognize CPT 99396. Instead, it uses its own wellness codes. Bill G0438 for the Initial Annual Wellness Visit and G0439 for the Subsequent Annual Wellness Visit. That guidance comes straight from CMS. Submit CPT 99396 under Medicare and it will be denied every time. Medicaid adds another challenge. Coverage rules change from state to state. Some programs require documented risk factors to justify a preventive visit. Others follow commercial payer timelines but add extra reporting steps. If your clinic serves Medicaid patients, check your state’s policy before billing.
A quick eligibility check can save hours of follow-up later. Before scheduling, confirm if the patient has already used their preventive benefit for the year. That single habit protects your reimbursement and reduces rework for your team. When you think about it, prevention works on two levels. You prevent disease for the patient and prevent revenue loss for the practice. Both start with one smart move: verify coverage before you bill.
Tips for Multi-Specialty Practices
Want to make preventive coding painless? Build systems that think ahead. Do not wait for denials to teach your team what went wrong. Set up workflows that catch errors before claims leave your EHR. Good systems turn coding from a reaction into a habit. So, what does that look like in real practice? Start with these simple but powerful steps:
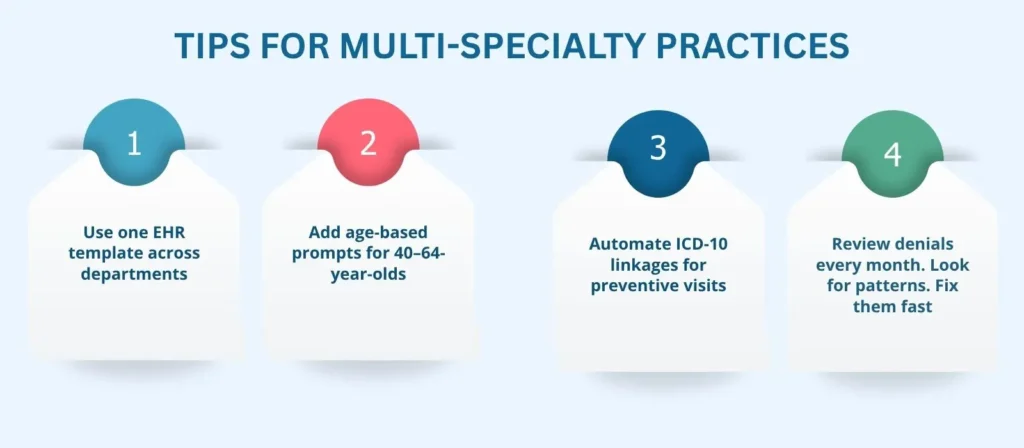
Clean data means cleaner revenue. The fewer edits your coders make, the faster claims clear. Accuracy at the front end saves hours at the back. When information flows right the first time, denials drop, payments move faster, and your team stays focused on care instead of corrections.
Did You Know?
According to CDC, nearly 60 percent of adults in the U.S. live with a chronic condition. Preventive visits like those billed under CPT 99396 help catch these conditions early before they spiral. Yet thousands of practices still underbill. Why? Missing documentation. Wrong codes. Unclear intent. Every lost preventive claim is lost care. When you document well, you don’t just protect revenue; you protect patients.
Partner with Pro-MBS for Coding Accuracy
Precision in coding builds trust. It keeps payers satisfied and your revenue steady. But staying accurate takes more than good intentions. It takes structure, training, and a partner who understands the rules inside and out. That is where Pro-MBS steps in. Our team helps practices stay compliant, uncover hidden errors, and strengthen preventive visit coding through expert audits and hands-on education.
We do not just review claims; we teach the process behind them. We help your staff see what payers see. From template design to ICD-10 mapping, from documentation review to denial analysis, we guide your team toward clean, confident billing. We speak payer language so you do not have to guess what they want. You focus on care. We focus on clarity.
FAQs
What are the billing guidelines for CPT code 99396?
CPT 99396 is a preventive medicine visit for established adult patients aged 40 to 64. It covers a full annual exam, including history, exam, and counseling. Always link a preventive Z-code and avoid mixing treatment diagnoses to ensure clean wellness visit reimbursement.
How to code a preventive visit?
Use the right adult preventive care CPT code based on age and patient status. Document lifestyle, risk factors, and counseling. Assign Z00.00 or Z00.01 to show preventive intent. Consistent documentation is what keeps multi-specialty coding accurate.
Does 99396 require a modifier?
Not for routine preventive visits. Add modifier 25 only when you perform a separate problem-oriented service during the same encounter. Clear notes must support both. This keeps your CPT 99396 claim compliant and protected during audits.
What is the age limit for CPT code 99396?
CPT 99396 applies to adult patients aged 40 through 64. Younger patients use 99391–99395, while older adults move to 99397. For Medicare patients, switch to G0438 or G0439 to stay aligned with preventive medicine visit rules.
Does CPT have guidelines?
Yes. The AMA CPT manual defines all documentation requirements for preventive medicine coding. It details what history, exam, and counseling elements must appear in the record. Following these keeps annual exam coding compliant and audit-ready.
Does Medicare pay for CPT code 99396?
No. Medicare does not cover CPT 99396. Instead, it pays for G0438 (Initial Annual Wellness Visit) and G0439 (Subsequent Wellness Visit). Always check CMS preventive policies before billing to ensure proper wellness visit reimbursement.
What are common CPT coding mistakes?
Using CPT 99396 for sick visits, missing Z-codes, or skipping counseling notes. These small gaps cause big denials. Strong documentation and smart multi-specialty coding practices keep preventive claims clean and paid on time.



