Inpatient Prospective Payment is how Medicare pays hospitals for inpatient stays. It is one of the most important billing rules in hospitals today. Every coder must understand it. Every biller must follow it.
For FY 2026, Medicare updated key rules under this system. These updates come from the CMS inpatient prospective payment system. They help reflect current hospital costs and patient care trends.
Hospitals do not bill each service under this method. They receive one set payment per inpatient stay. That payment still depends on coding accuracy.
Recent FY 2026 changes include updates to high-cost case rules. The cost outlier threshold was lowered to about $40,397. This means hospitals may qualify for extra payment sooner on costly cases.
CMS also added some Medicare Advantage data to readmission measures. This helps create fair comparisons across hospitals. It also affects quality-related payment reviews.
This guide explains the Inpatient Prospective Payment first. Details come later. Examples stay simple.
If you work in IPPS medical billing, this matters every day. If you are a student, this is core knowledge for your career.
What Is Inpatient Prospective Payment
Inpatient Prospective Payment is a Medicare payment method. It applies only to inpatient hospital claims.
Under Inpatient Prospective Payment:
- Fixed Payment: Hospitals receive one fixed payment for each inpatient admission, no matter how much care is given
- Full Stay Coverage: The payment covers the full stay, from admission day through discharge day
- Service Independence: Services do not change payment, so more tests or treatments do not increase reimbursement
Hospitals do not bill each test. They do not bill each supply. They do not bill each treatment.
The payment amount is set in advance. This supports predictable Medicare inpatient payment. This system does not apply to outpatient care. It does not apply to doctor office visits.
What Is the Inpatient Prospective Payment System IPPS
The inpatient prospective payment system is the formal name. It is often called IPPS. The inpatient prospective payment system was created by the Centers for Medicare & Medicaid Services (CMS). CMS manages Medicare inpatient payment rules.
Under the Inpatient Prospective Payment System:
- Payment is pre-set, meaning the hospital knows the payment amount before the patient is discharged
- Length of stay does not increase payment, even if the patient stays more days than expected
- Extra services do not increase payment, including added tests, treatments, or supplies
Hospitals must manage care efficiently. Coders must code carefully. Billers must follow IPPS billing rules. This structure defines IPPS medical billing in hospitals.
Why Inpatient Prospective Payment Matters in Medical Billing
Inpatient Prospective Payment directly affects hospital revenue. Every code affects Medicare inpatient payment.
Errors can cause:
- Underpayment
- Overpayment
- Claim denials
- Audits
Overpayment creates compliance risk. Underpayment causes lost income. IPPS medical billing is closely monitored. CMS reviews inpatient claims carefully.
New coders face a higher risk. Students often miss key diagnoses. Learning Inpatient Prospective Payment early reduces errors.
How Inpatient Prospective Payment Works Step by Step
The Inpatient Prospective Payment System follows a clear process. Each step affects the final payment.
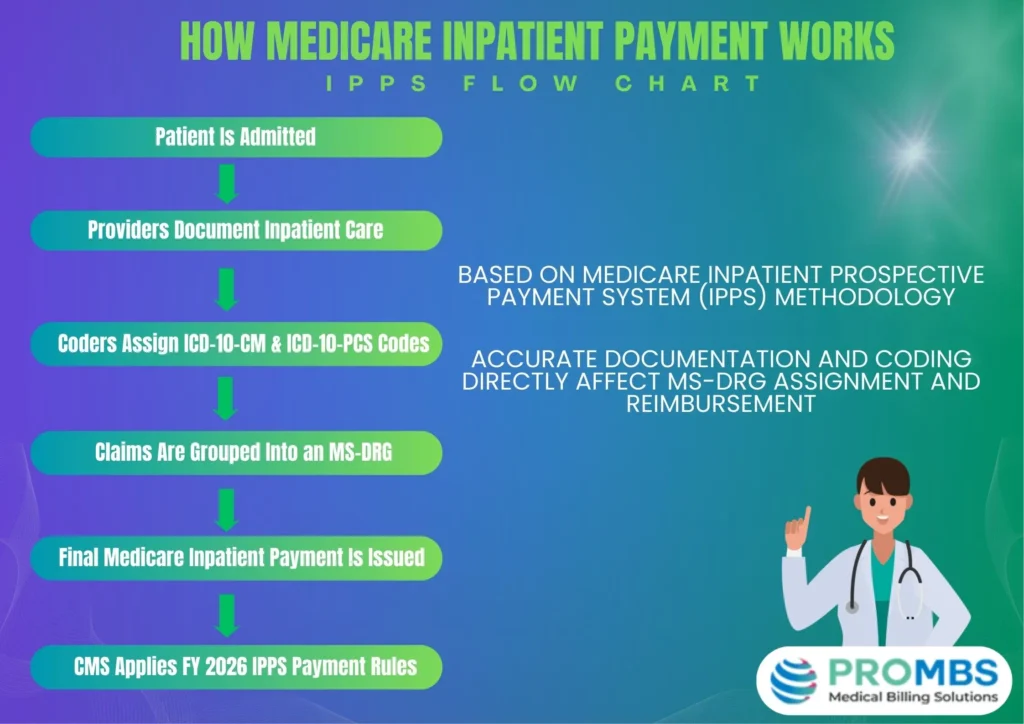
Basic Process:
- The patient is admitted as an inpatient, which confirms the stay qualifies for inpatient payment rules
- Providers document conditions and care, including diagnoses, symptoms, and treatments
- Coders review the full medical record, looking for clear and complete documentation
- Diagnosis and procedure codes are assigned, based on what the provider documented
- The claim groups into a DRG, which determines the payment amount
- Payment is issued under IPPS, using the assigned DRG and hospital factors
The payment amount is final. Mistakes change Medicare inpatient payment results.
What Is a DRG in the Inpatient Prospective Payment System?
A DRG is a Diagnosis-Related Group. It groups similar inpatient cases. DRGs control payment under Inpatient Prospective Payment. This is called the DRG payment system.
Each inpatient stay:
- Gets one DRG
- Receives one payment
- Is paid regardless of services
DRGs are based on:
- Principal diagnosis
- Procedures performed
- Patient severity
Correct DRGs are essential in IPPS medical billing.
Codes Used in Inpatient Prospective Payment
IPP uses inpatient codes only. Outpatient codes do not apply. Coding accuracy controls the DRG payment system.
Diagnosis Codes (ICD-10-CM)
Diagnosis codes explain why the patient was admitted.
Key points:
- One principal diagnosis
- Secondary diagnoses affect severity
- Missing codes lower payment
These codes directly affect Medicare inpatient payment.
Procedure Codes (ICD-10-PCS)
Inpatient procedures use ICD-10-PCS codes. CPT codes are not used.
PCS codes:
- Describe inpatient procedures
- Often change DRGs
- Impact payment
PCS errors are common in IPPS medical billing.
Discharge Status Codes
Discharge status shows how the patient left.
Errors can:
- Reduce payment
- Trigger audits
- Delay claims
Correct status supports IPPS billing rules.
What Affects Payment Under the Inpatient Prospective Payment System?
Payment under this System depends on set factors. These factors adjust the DRG payment system.
Payment Factors:
- DRG weight, which reflects how complex and costly the patient’s care was
- Hospital location, since payment rates vary by region, and labor costs
- Teaching status, because teaching hospitals receive payment adjustments
- Patient severity, which reflects how sick the patient was during the stay
- Complications, which show added conditions that required more care
Complications include:
- CC, which means a condition that increases care needs
- MCC, which means a major condition that greatly increases care needs
Correct coding increases proper Medicare inpatient payment.
Common Inpatient Prospective Payment Mistakes by Beginners
Beginners often make the same mistakes. These errors affect Inpatient Prospective Payment results.
Common Errors:
- Wrong principal diagnosis
- Missing secondary diagnoses
- Incorrect inpatient status
- Using CPT instead of PCS
- Weak documentation support
Each error can:
- Change the DRG
- Reduce payment
- Increase audit risk
Strong basics prevent these issues.
Inpatient Prospective Payment vs Other Payment Systems
IPPS works differently than other models.
Key Differences
- Inpatient payment is per stay
- Outpatient payment is per service
- Fee-for-service pays per item
In inpatient billing:
- More services do not increase payment
- Coding accuracy matters more
This difference explains IPPS billing rules importance.
Who Should Learn Inpatient Prospective Payment First?
Inpatient Prospective Payment is core knowledge for hospital billing work. Learning it early builds strong billing and coding skills.
- It is important for:
- Medical billing students, because inpatient billing rules differ from outpatient rules
- Entry-level coders, since inpatient coding directly controls hospital payment
- Hospital billing staff, who submit claims that must follow IPPS requirements
- Revenue cycle teams, because inpatient payment affects overall hospital revenue
Early learning reduces errors and confusion. It also improves accuracy in IPPS medical billing.
Key Takeaways for Students and Coders
IPP pays hospitals one set amount for each inpatient stay. This payment method applies only to Medicare inpatient claims. It is not used for outpatient visits or doctor office care.
The CMS inpatient prospective payment system controls how hospitals are paid. Payment amounts are adjusted based on hospital factors and patient needs. These adjustments can include a cost of living adjustment for certain locations.
Coding accuracy drives the DRG payment system under Inpatient Prospective Payment. Correct codes help hospitals receive proper Medicare inpatient prospective pay. Missing or incorrect codes can lower payment or trigger audits.
IPPS medical billing requires careful review of documentation. Errors increase audit risk and delay reimbursement.
About the Author
This article was written by a healthcare revenue cycle professional with hands-on Inpatient Billing experience. The author has worked with hospital claims, DRG assignment, and IPPS medical billing rules. Their background includes coding accuracy, billing compliance, and Medicare reimbursement workflows. This experience ensures the content is accurate, current, and beginner-friendly.
Frequently Asked Questions About Inpatient Prospective Payment
What does Inpatient Prospective Payment mean?
Inpatient Prospective Payment means hospitals are paid one fixed amount for an inpatient stay. This payment comes from the Medicare inpatient prospective payment system. The amount is decided before the patient leaves the hospital.
It covers all care during the stay, including tests and treatments. The payment does not change if the patient stays longer or receives more services.
Who uses the inpatient prospective payment system?
Medicare uses the inpatient prospective payment system IPPS to pay hospitals. This system applies only to inpatient hospital claims.
Hospitals must follow set rules when billing under this system. Coding accuracy is required because codes decide the payment amount. This is why IPPS medical billing is closely monitored.
Is it used for all hospitals?
No, the Medicare inpatient prospective payment system is not used for every hospital. Some hospitals are excluded due to location or special status. Examples include certain rural or specialty hospitals. These hospitals follow different Medicare payment rules.