Updated for 2026 ICD-10-CM rules
Reviewed by a CPC (Certified Professional Coder) at Pro-MBS,
specializing in medical coding accuracy, billing compliance, and ICD-10-CM standards
What Is Vertigo ICD 10?
Vertigo feels like the world spins when you stand still.
Vertigo ICD 10 is the diagnosis code system used to explain that spinning feeling for medical billing and records. Vertigo is not a disease first. It is a symptom. Doctors code it when the visit happens because of spinning, imbalance, or motion sensation.
Why does ICD 10 treat vertigo differently from dizziness?
Because dizziness is vague. Vertigo has movement. Payers want clarity. CMS coding rules separate the two to reduce misuse and overbilling.
If the chart only says “dizzy,” vertigo coding fails. If the chart explains spinning or motion, vertigo coding stands strong. This section answers one question clearly:
What is Vertigo ICD 10? It is the ICD 10 coding method used to describe spinning symptoms that drive care.
What Is the ICD 10 Code for Vertigo?
The ICD 10 Code for Vertigo is used when vertigo symptoms cause the visit, and no final condition is confirmed yet.
Doctors use this code during early evaluation. They use it when testing is still ongoing. Why do payers expect progress?
Because CMS expects diagnosis codes to evolve. If vertigo stays coded the same across many visits, audits begin. Vertigo codes explain why care happened. They do not replace the final diagnosis.
This is why ICD 10 Vertigo works best at the start, not forever.
Vertigo ICD 10 Code Categories (With Code Examples)
Vertigo does not use one single ICD-10-CM code. Instead, Vertigo ICD 10 coding follows a clear path based on how much the provider knows at the time of the visit.
ICD-10-CM separates symptom reporting from confirmed inner ear disorders on purpose. This structure allows payers to see how the diagnosis develops over time. Early visits focus on what the patient feels. Later visits reflect what the provider confirms through exams, testing, or specialist input.
At the start of care, symptom-based codes explain why the patient came in. As providers gather more information, coding must move forward. This progression matches CMS documentation expectations and helps reduce audit risk.
The table below shows the most commonly used ICD-10-CM codes for vertigo and explains how each category fits into real-world billing.
| Category | Common ICD-10-CM Codes | How It Is Used |
|---|---|---|
| General vertigo | R42 | Used during early visits when the patient reports spinning or motion sensation, and no cause has been confirmed |
| Positional vertigo | H81.10, H81.13 | Used when vertigo clearly occurs with head or body movement, such as rolling or bending |
| Benign positional vertigo | H81.11 | Used only after the provider confirms benign paroxysmal positional vertigo through clinical evaluation |
| Unspecified vertigo | R42 (temporary use) | Used briefly when documentation is incomplete or diagnostic testing is still underway |
These examples show why Vertigo ICD 10 Code selection depends on detail. Codes like R42 support early evaluation, but they do not support long-term treatment without added findings. When providers document triggers, exam results, or confirmed diagnoses, coding must advance to vestibular-specific options such as H81.1x.
From a payer viewpoint, this progression shows responsible care and clinical reasoning. From a billing standpoint, it strengthens medical necessity, supports clean claims, and lowers the risk of denials or post-payment review.
In vertigo billing, detail does not slow care. Detail protects payment.
| Condition | ICD-10-CM Code |
|---|---|
| Right ear BPPV | H81.11 |
| Left ear BPPV | H81.12 |
| Bilateral BPPV | H81.13 |
| Unspecified ear | H81.10 (frequent RTP risk in 2026) |
For 2026 claims, providers must document laterality. Continued use of unspecified ear codes is a common cause of immediate Return to Provider denials rather than post-payment audits.
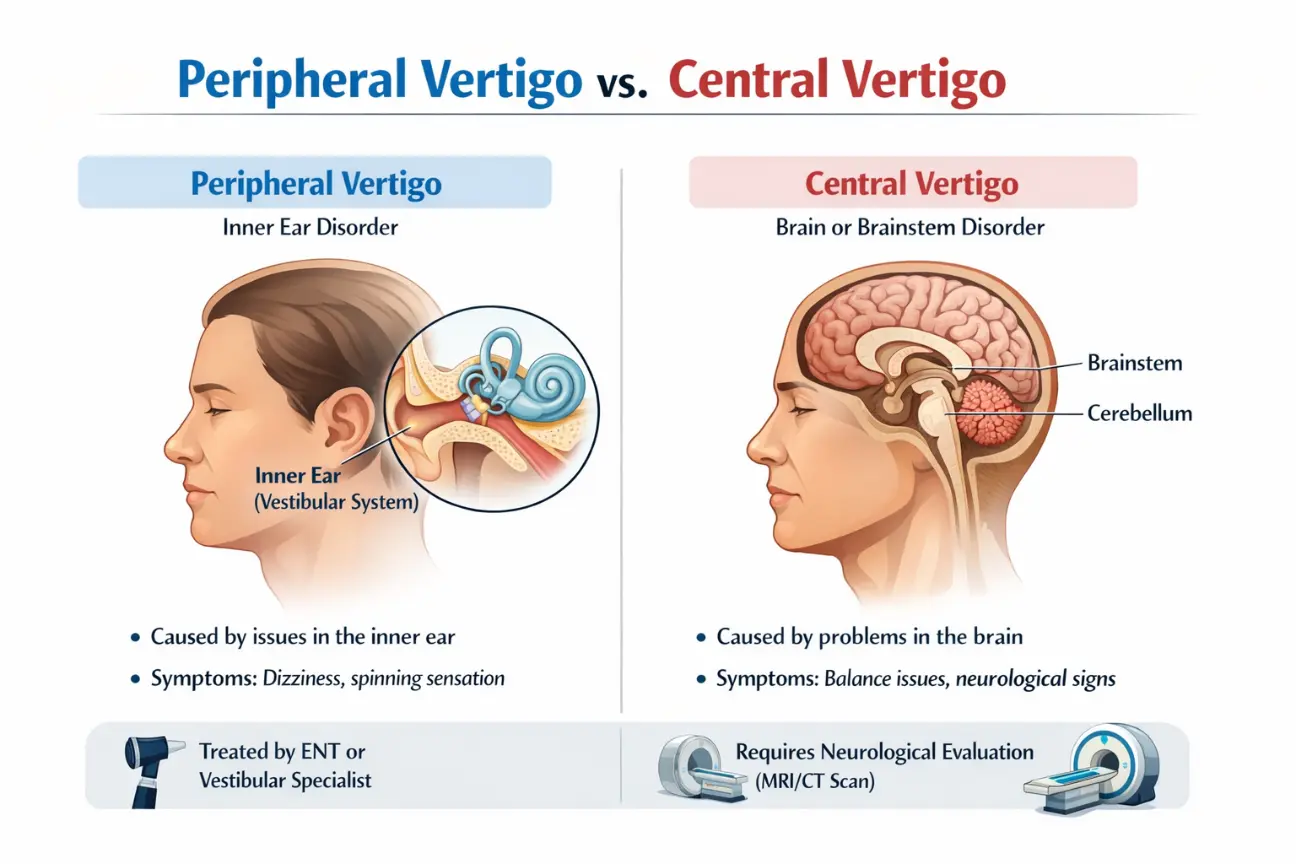
Peripheral vs. Central Vertigo: Where Does the Spinning Start?
The most important question in vertigo coding is whether the problem starts in your inner ear or your brain. Doctors and billers call these two categories "peripheral" and "central." Knowing the difference is the only way to pick the right ICD-10 code and avoid a denied claim.
Peripheral vertigo is the most common type and starts in the inner ear. The "vestibular system" in your ear controls your balance, and when it sends the wrong signals to your brain, you feel like you are spinning. Codes for this usually start with H81. Common causes include BPPV (ear crystals) or ear infections.
These are usually not life-threatening, but they make it very hard to stand up.
Central vertigo is much more serious because it starts in the brain, specifically the brainstem or cerebellum. This is coded as H81.4. Because the brain is the control center for the whole body, central vertigo usually comes with other "red flag" symptoms like slurred speech, double vision, or trouble swallowing.
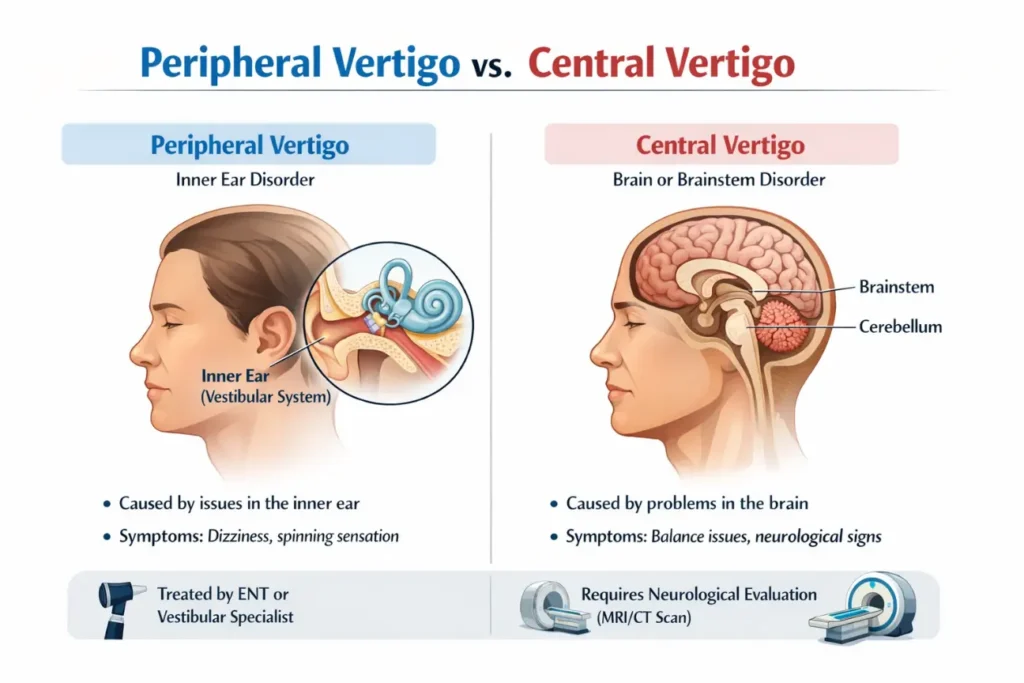
Payers like Medicare almost always require an MRI or a specialist's note to prove that the vertigo is central rather than a simple ear issue.
Quick Comparison for Coding
| Feature | Peripheral (Inner Ear) | Central (Brain) |
|---|---|---|
| Common Code | H81.11, H81.12 | H81.4 |
| How it feels | Severe spinning | Intense imbalance |
| Main Cause | Ear crystals or fluid | Stroke, Migraine, or Tumors |
| Billing Rule | Requires laterality (R or L) | Requires neurological proof |
What Is the Vertigo ICD 10 Code Used for Billing?
Why does Vertigo ICD 10 matter so much for billing? Because it supports medical need. Payers review vertigo claims closely. They want proof that symptoms required exams, imaging, or referrals.
Common billing scenarios
- Emergency visits for spinning
- Office visits with balance complaints
- Neurology or ENT referrals
- Imaging ordered due to vertigo
When documentation is weak, denials follow. AMA coding guidance warns against vague symptom use without follow-up detail. Vertigo coding must match the story in the notes. No story, no payment.
What Is Vertigo ICD 10 Unspecified?
ICD 10 Code for Unspecified Vertigo is used when vertigo is present but the cause is unknown.
This code fits first visits. It fits early testing. It does not fit long-term care. When is ICD 10 vertigo unspecified acceptable?
- First encounter
- No confirmed cause
- Testing still pending
Why is it time-limited? Because CMS expects answers. If weeks pass and the code stays the same, the claim looks careless. Unspecified does not mean safe. It means temporary.
Unspecified does not mean safe. It means temporary.
When R42 and an H81.xx code are billed together, payer claim-edit software automatically removes R42 due to Excludes1 rules. If the remaining diagnosis is not well supported in the documentation, this can reduce the perceived complexity of the visit and impact E/M payment.
What Is ICD 10 for Vertigo Unspecified and When Should It Change?
Payers expect diagnosis movement. ICD 10 for Vertigo Unspecified should change when:
- Imaging confirms a cause
- Positional triggers appear
- A specialist confirms BPPV
- Symptoms repeat with a pattern
Repeat visits using the same unspecified code raise flags. OIG audits often focus on symptom codes used too long. The rule is simple. Symptoms explain visits. Diagnoses explain care plans.
What Is Positional Vertigo ICD 10?
Positional vertigo happens when head movement causes spinning.
Positional Vertigo ICD 10 differs from general vertigo because it has triggers. Rolling in bed. Looking up. Bending down.
What documentation supports it?
- Head movement triggers
- Short spinning episodes
- Repeatable symptoms
- Exam findings
Without triggers, positional coding fails.
What Is Benign Positional Vertigo ICD 10?
Benign positional vertigo means the vertigo comes from the inner ear and is not life-threatening.
Benign Positional Vertigo ICD 10 applies only when providers confirm the cause. Why does “benign” still need proof? Because billing does not accept assumptions. AMA documentation rules demand clinical support.
Benign does not mean optional. It means specific.
What Is Benign Paroxysmal Positional Vertigo ICD 10?
BPPV is common. It is also audited often. Benign Paroxysmal Positional Vertigo ICD 10 is used when:
- Spinning lasts seconds
- Head movement triggers symptoms
- Exams confirm inner ear crystals
Why do payers audit it?
- High volume
- Easy to misuse
- Often confused with general vertigo
CMS reviews BPPV claims closely. Clear notes protect payment.
What Are the Most Common Coding Mistakes With Vertigo ICD 10?
Mistakes cost money.
Common errors
- Confusing dizziness with vertigo
- Using unspecified codes too long
- Missing positional triggers
- Failing to update codes after diagnosis
These mistakes repeat across audits. OIG reports show symptom misuse as a frequent issue. Strong coding follows strong notes. Always.
CPC Pro-Tip for 2026:
Do not use H81.13 (Bilateral) simply because the patient reports spinning on both sides. Auditors expect clinical proof, such as positive Dix-Hallpike findings on both the right and left. When documentation does not clearly support bilateral involvement, code the most symptomatic side.
Key Takeaway
Vertigo ICD 10 coding is simple when the story is clear. Symptoms open the door. Diagnoses finish the job. Progress protects payment. When vertigo spins, your coding should stay steady.
Frequently Asked Questions
How do I code ICD 10 Vertigo caused by a vestibular migraine?
When vertigo is a manifestation of a migraine, the primary code should be G43.821 (Vestibular migraine, intractable) or G43.829 (Vestibular migraine, not intractable). You should not use R42 or H81 codes in this scenario, as G43.82x captures the neurological origin of the symptoms.
When should I use H81.4 (Vertigo of central origin)?
Use H81.4 when the vertigo is determined to be "central" (originating from the brain or brainstem) rather than "peripheral" (inner ear). This often follows a neurological exam or MRI that rules out inner ear issues. Documentation must clearly state "central positional nystagmus" or "central vertigo" to support this code.
Why was my claim denied when using R42 for a repeat visit?
Claims using R42 for multiple visits are often denied for "lack of medical necessity" or "failure to reach a definitive diagnosis." Payers view R42 as a temporary code. If you are billing for ongoing treatment or vestibular rehabilitation, the code must evolve to a specific diagnosis (like H81.11 or H81.39) to prove the patient requires specialized, long-term care.
Can I bill R42 (Dizziness) and H81.11 (BPPV) together?
No. Under ICD-10-CM Excludes1 rules, symptom-based codes such as R42 should not be reported with definitive diagnosis codes from the H81 category. Once a diagnosis like BPPV is confirmed, the symptom of dizziness is considered inherent and must be dropped to prevent mutually exclusive denials.
When does “Unspecified Vertigo” (H81.10) become a billing risk?
Unspecified codes generally become a risk after the second or third encounter. Payers, including Medicare, expect that by the follow-up visit the provider has documented laterality, such as right ear H81.11 or left ear H81.12. Continued use of H81.10 without clinical justification for why laterality cannot be identified may trigger automated medical necessity denials.
Does Medicare require a secondary code with R42 for vestibular testing?
Often, yes. While R42 is a valid primary diagnosis for an initial vertigo evaluation, many Medicare Local Coverage Determinations require either a more specific secondary diagnosis or clear documentation showing referral for further evaluation to justify higher-cost vestibular tests such as videonystagmography or caloric testing.
What is the correct ICD-10 code for vertigo with nausea?
There is no single combination code for vertigo and nausea. Report the primary vertigo diagnosis first, such as H81.11 for benign paroxysmal positional vertigo of the right ear, followed by R11.0 for nausea or R11.2 for nausea with vomiting. Documenting both symptoms supports encounter complexity for appropriate E/M billing.
How should I code vertigo caused by a vestibular migraine?
Use G43.821 for vestibular migraine, intractable, or G43.829 for vestibular migraine, not intractable. Do not report R42 or H81 codes as primary diagnoses in this scenario. Vestibular migraine is a neurological condition, and the G43.82x category already includes the vertigo symptom.
What is the ICD-10 code for vertigo of central origin?
The correct code is H81.4, vertigo of central origin. This diagnosis applies when vertigo arises from the central nervous system, such as the brainstem or cerebellum. Because this code implies a serious neurological cause, payers expect supporting documentation such as MRI findings or detailed neurological examination notes.