Prior authorization (PA) remains the number one revenue bottleneck for providers in 2025. According to the American Medical Association (AMA), more than 1 in 4 physicians (29%) reported in a 2024 survey that prior authorization contributed to a serious adverse event for a patient under their care, including outcomes such as hospitalization, permanent impairment, or even death. These delays not only disrupt patient care but also strain cash flow and create administrative waste.
Many practices report revenue leakage ranging from several thousand dollars per month due to delayed or denied authorizations. Industry data shows that prior authorization denial rates typically fall between 15–20%, though certain specialties such as cardiology, oncology, and radiology experience significantly higher rejection levels. With structured workflows and payer-aligned strategies, providers can realistically reduce these denials by 30% or more.
What are the root causes of prior authorization denials?
Insufficient Medical Necessity Documentation
One of the leading reasons for PA denials is the lack of adequate medical necessity proof. Missing clinical notes, incomplete histories of prior treatments, or absent diagnostic test results often cause payers to reject requests. Clear, detailed documentation that ties the diagnosis to the requested service is essential for approval.
Incorrect ICD-10/CPT Linkage
Denials frequently occur when the ICD-10 diagnosis code does not align with the CPT procedure code. Even small mismatches can trigger payer edits and claim rejections. For example, billing CPT 70551 (MRI of the brain without contrast) with a diagnosis code that is not listed as covered under the payer’s Local Coverage Determination (LCD) or National Coverage Determination (NCD) will almost always result in a denial. Similarly, requesting high-cost drugs or DME under HCPCS codes without the appropriate ICD-10 indication is a common trigger for rejection. Ensuring proper linkage between diagnosis and procedure codes strengthens medical necessity and reduces errors at the payer level.
Payer-Specific Policy Gaps
Every payer has unique requirements for prior authorization. Medicare, Medicaid, and commercial insurers often differ in documentation standards, covered services, and pre-authorization thresholds. Failure to meet these policy-specific requirements leads to automatic denials, even when the clinical justification is valid.
Eligibility Errors
Timeliness Issues
Strict deadlines govern both prior authorization submissions and follow-up responses. Requests that are late, incomplete, or not monitored through to resolution often result in denials regardless of medical validity. Real-time tracking systems and proactive follow-ups are necessary to avoid revenue loss tied to timing errors.
Understanding these drivers is the foundation for building denial-prevention workflows.
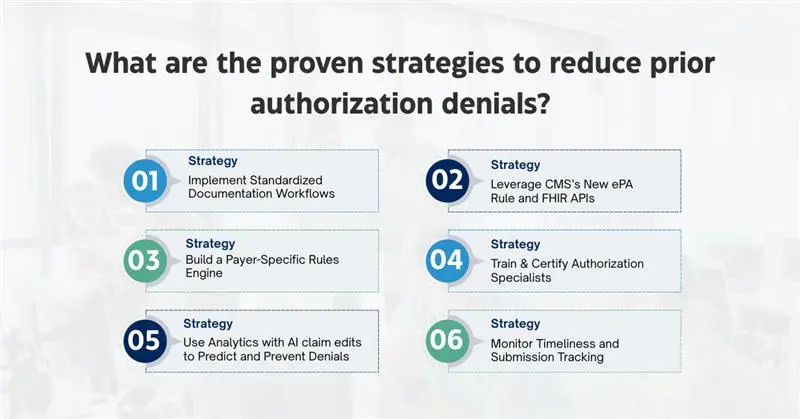
What are the proven strategies to reduce prior authorization denials?
Strategy 1 – Implement Standardized Documentation Workflows
The single largest contributor to prior authorization denials is incomplete or insufficient documentation of medical necessity. Payers require clear justification for why a service, test, or medication is appropriate, and even minor omissions can trigger a rejection. Every request should include a detailed diagnosis coded with ICD-10 specificity, a history of prior treatments or failed therapies when relevant, and any supporting evidence such as imaging reports, lab results, or physician notes.
To prevent gaps, providers can establish standardized documentation workflows using templates, checklists, and EHR-integrated tools that automatically prompt clinicians to include required elements before submission. This level of standardization reduces variability, eliminates common errors, and creates an audit-ready record for each request. In turn, practices see fewer avoidable denials and faster approval timelines.
Strategy 2 – Leverage CMS’s New ePA Rule and FHIR APIs
In 2025, the Centers for Medicare & Medicaid Services (CMS) finalized the nationwide electronic prior authorization (ePA) mandate, a transformative shift in how requests are processed. Under this rule, payers must support Fast Healthcare Interoperability Resources (FHIR) APIs, which enable seamless, real-time exchange of clinical and administrative data between provider EHR systems and payer platforms.
For providers, this means PA requests can now be submitted directly from within their EHR or revenue cycle system and receive near real-time decisions, eliminating the traditional delays associated with fax submissions, phone calls, and proprietary payer portals. By adopting ePA-enabled workflows, providers not only accelerate the authorization process but also significantly reduce denials caused by outdated submission formats or missing fields.
Strategy 3 – Build a Payer-Specific Rules Engine
One of the persistent challenges in prior authorization is the lack of uniformity across payers. Medicare, Medicaid, and commercial insurers each maintain distinct policies, documentation requirements, and coverage limitations for drugs, imaging, and procedures. A one-size-fits-all approach almost guarantees denials.
To overcome this, organizations should develop and maintain a payer-specific rules engine; a centralized matrix that outlines documentation requirements by payer and specialty, pre-authorization thresholds for high-cost medications or devices, and any CPT/HCPCS code restrictions. When integrated into PA workflows, this rules engine guides staff to meet payer expectations before submission, dramatically improving first-pass approval rates and reducing time spent on appeals.
Strategy 4 – Train & Certify Authorization Specialists
Strategy 5 – Use Analytics with AI claim edits to Predict and Prevent Denials
Denials are often predictable when viewed through the lens of data. By analyzing historical claims, providers can identify high-risk services, common payer rejection trends, and even specific providers whose documentation practices frequently trigger payer scrutiny.
Predictive analytics tools can highlight services with historically high denial rates, such as advanced imaging or specialty drugs, while also flagging payers with stricter enforcement policies. Importantly, many payers are now deploying AI-driven claim edits that automatically detect mismatches in coding, documentation gaps, or medical necessity issues before the claim is fully adjudicated. This makes it even more critical for providers to apply predictive analytics proactively on their side to anticipate these edits and prevent avoidable denials.
With these insights, practices can deploy pre-submission checks and allocate additional resources to high-risk requests. This proactive use of analytics transforms denial management from a reactive process into a forward-looking prevention strategy that directly improves first-pass approval rates.
Strategy 6 – Monitor Timeliness and Submission Tracking
What compliance and audit risks do providers face with prior authorizations?
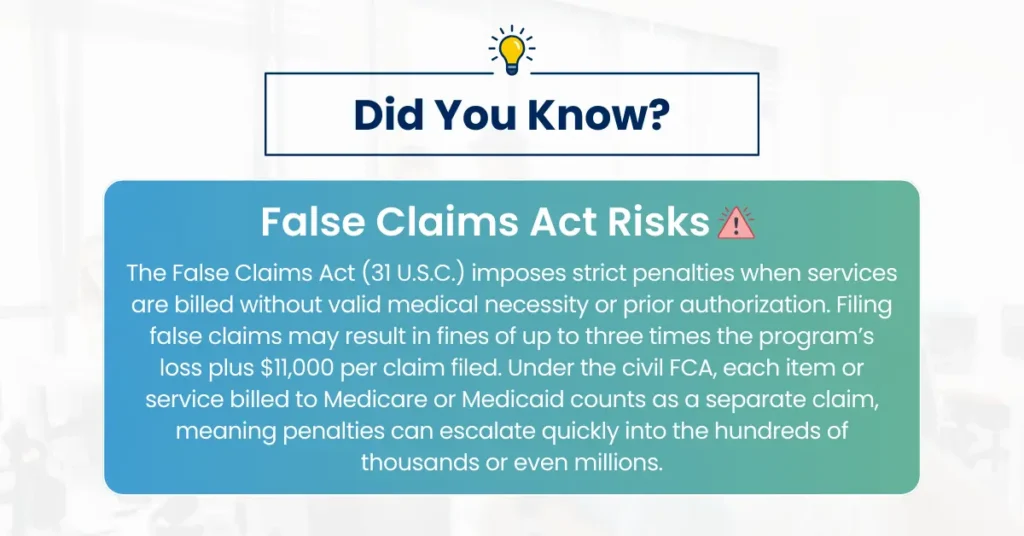
In 2025, the Office of Inspector General (OIG) placed prior authorization (PA) compliance on its formal work plan, signaling a heightened federal focus on how providers justify medical necessity. This reflects growing concerns that payers and providers may not consistently apply CMS and payer-specific guidelines when submitting or approving authorizations. For healthcare organizations, failure to comply with PA requirements now carries risks beyond revenue loss. Noncompliance can trigger civil monetary penalties under the False Claims Act when services are rendered without valid prior authorization or medical necessity. In addition, organizations may face repayment demands, contract sanctions, and increased scrutiny during payer and federal audits.
To mitigate these risks, providers must maintain audit-ready records for every authorization request. An audit-ready file should include the physician’s clinical documentation, medical necessity justification tied to ICD-10 codes, supporting diagnostic test results, and any payer correspondence. Storing this information in a structured, easily retrievable format ensures that organizations can quickly demonstrate compliance if challenged by CMS, commercial payers, or regulatory bodies.
Compliance-first workflows are no longer optional, they are a strategic requirement. By embedding documentation standards, payer-specific rules, and automated tracking into prior authorization processes, providers not only reduce denials but also strengthen their audit defensibility. In a regulatory environment where oversight is intensifying, proactive compliance safeguards both financial stability and institutional reputation.
How can providers measure a 30% reduction in PA denials?
Reducing prior authorization denials by 30% is not just a theoretical goal, it is a measurable performance outcome when organizations track the right key performance indicators (KPIs). The most critical metric is the denial rate by service line, since specialties like cardiology, radiology, and specialty pharmacy often experience disproportionately high rejection levels. Segmenting denial data by service type allows providers to identify where interventions are most effective.
Equally important is monitoring authorization approval turnaround times. Comparing timelines before and after implementing workflow changes provides tangible evidence of process efficiency. A reduction in delays directly translates to faster scheduling, quicker reimbursement, and improved patient satisfaction. In addition, organizations should evaluate appeals success rates, since effective first-pass submissions reduce dependency on time-consuming appeals that drain staff resources.
With standardized workflows, payer-specific rules engines, and analytics-driven tracking, many healthcare organizations begin to see measurable improvements within 90 to 120 days. These improvements are typically reflected in higher clean claim rates, faster cash flow, and a noticeable decline in revenue leakage. Over time, sustained monitoring of denial trends not only validates the 30% reduction target but also positions providers to continually optimize their prior authorization strategy.
How does Pro-MBS help providers reduce prior authorization denials?
We understand that prior authorization is both a compliance requirement and a revenue protection challenge. Our approach is built on payer-specific authorization workflows that eliminate submission errors before they occur. Every request is reviewed and structured using a rules engine aligned with payer policies, ensuring documentation is complete, medically necessary, and fully audit-ready. By standardizing these processes, our certified authorization specialists significantly reduce first-pass denials and strengthen payer compliance.
Beyond manual expertise, Pro-MBS leverages technology-driven integration with EHR and RCM platforms to streamline submissions, automate tracking, and provide real-time visibility into authorization status. This combination of automation and payer-specific expertise allows us to resolve issues proactively rather than reactively. The result is measurable improvement, providers partnering with Pro-MBS consistently achieve fewer denials, faster approvals, stronger compliance, and improved cash flow, even in the face of CMS’s evolving ePA and interoperability requirements.