The medical billing cycle is not just about sending invoices. It is the full process of converting a patient visit into revenue. When it works well, your practice runs smoothly, claims get paid on time, and your staff can focus on patients. When it breaks down, you face delays, denials, and lost income.
This article explains the full medical billing cycle, highlights common problems, and shows how working with a healthcare billing company can make a real difference.
What Is the Medical Billing Cycle?
The medical billing cycle is the complete set of steps used to track and manage a patient’s bill from start to finish. It begins before the patient even walks into your office and ends once all payments are collected.
Each step is connected. If one part is missed or done incorrectly, it can cause payment delays or denied claims. That is why it is important to understand the process from beginning to end.
Why the Billing Cycle Matters for Your Practice
A well-managed billing workflow is essential to the financial health of any healthcare organization. When the billing cycle works as it should, you get paid faster, avoid costly errors, and create a better experience for your patients.
On the other hand, a weak billing process can lead to:
- Revenue loss due to unpaid or rejected claims
- Increased staff workload from rework and corrections
- Frustration for both staff and patients
- Compliance risks with insurance payers
Understanding the billing cycle helps your team take control of your revenue rather than chasing it after the fact.
Step-by-Step Breakdown of the Medical Billing Cycle
1. Pre-Registration
- Full name and contact details
- Insurance provider and policy number
- Reason for the visit
2. Insurance Verification
- The policy is active
- Services are covered
- Copayments and deductibles are known
- Any pre-authorizations are obtained
3. Patient Check-In and Copay Collection
When the patient arrives, the front desk confirms all details and collects the appropriate copay. They may also update contact or insurance information if anything has changed.
Collecting payments upfront improves cash flow and ensures patients are aware of their responsibilities.
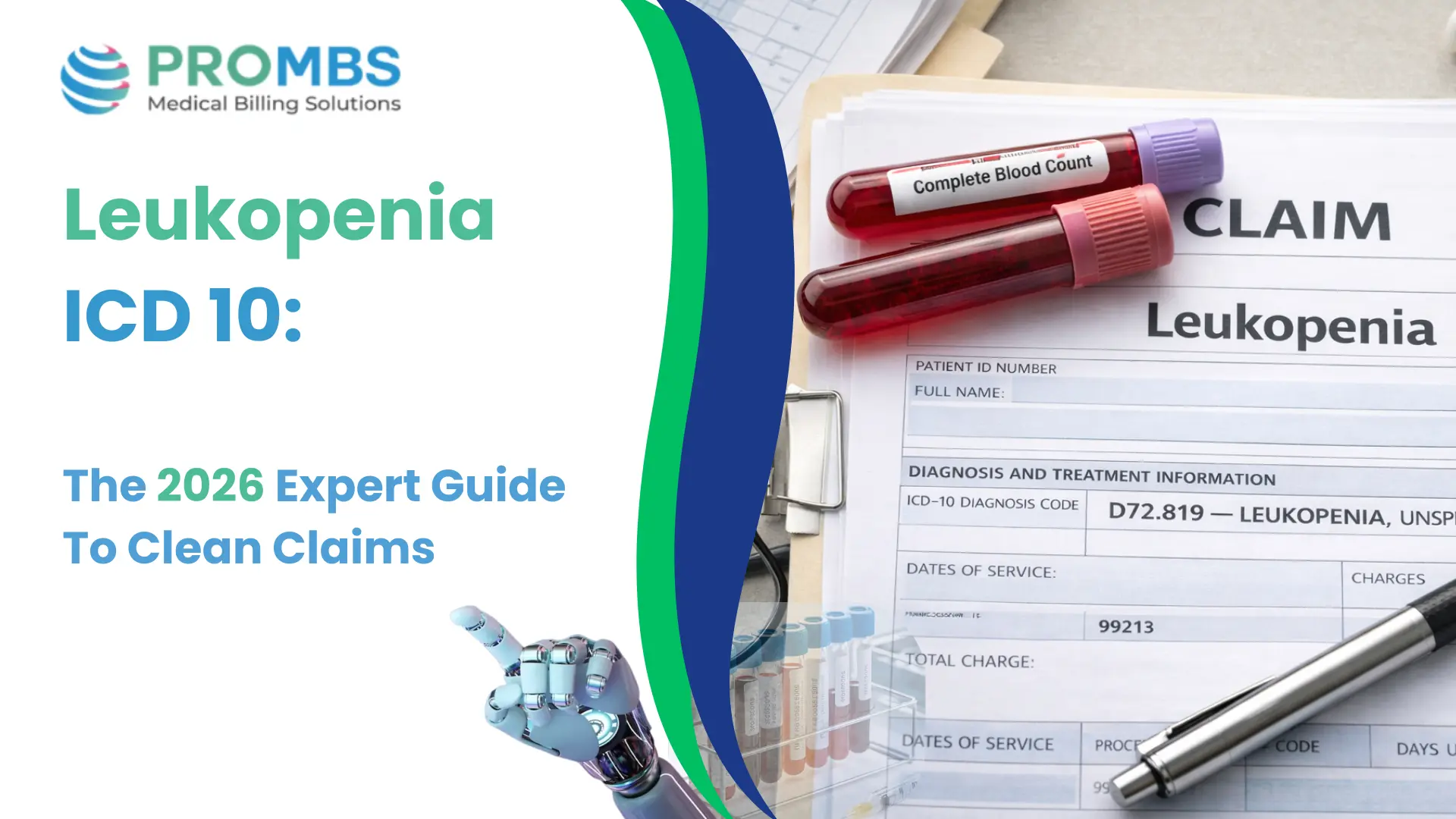
4. Provider Documentation and Medical Coding
After the appointment, the provider documents the visit and services provided. Medical coders then assign the correct CPT, ICD, and HCPCS codes.
Accurate coding is essential for reimbursement. Coding errors are one of the most common reasons claims are denied.
5. Charge Entry
The next step is entering the charges into the billing system. This process includes:
- Linking procedures to the appropriate codes
- Ensuring service dates match the documentation
- Adding any required modifiers
Correct charge entry prepares the claim for timely submission.
6. Claim Submission
With charges and codes in place, the claim is submitted to the insurance payer. Most claims are sent electronically for faster processing.
Clean claims that are properly formatted and complete are more likely to be accepted on the first try.
7. Claim Follow-Up
After submission, the billing team monitors the claim status. They follow up on any:
- Rejections due to formatting or missing data
- Denials based on coverage or documentation issues
- Delayed responses from the payer
Staying on top of claim status prevents long payment delays.
8. Payment Posting
Once a claim is approved, payment is received and posted to the patient’s account. The Explanation of Benefits (EOB) from the payer explains:
- What was paid
- What was denied or adjusted
- The amount the patient owes
This step is also where you can catch underpayments or repeated issues with specific payers.
9. Patient Billing
If a balance remains, the patient is billed for the remaining amount. Clear and timely statements help patients understand what they owe and encourage prompt payment.
Offering digital payment options or payment plans can also improve collection rates.
10. Collections and Reporting
Some accounts may go unpaid despite your best efforts. At this point, you may need to:
- Send follow-up reminders
- Make phone calls
- Use a collection agency as a last resort
In addition, analyzing your billing reports regularly helps you see where problems are happening and which parts of your workflow need improvement.
Common Challenges in the Billing Process
Incomplete or Incorrect Insurance Info
Documentation Gaps
Delayed Follow-Up
Outdated Billing Software
Why Work with a Healthcare Billing Company
Handling the full billing cycle internally can be time-consuming. That is why many practices partner with a healthcare billing company.
Pro-MBS offer a full range of billing support, including:
- Medical Billing & Coding Services
- Physician Credentialing Services
- Contact Center & Patient Scheduling Services
- AR & Denial Management Services
- Ambulatory Surgical Center Billing (ASC)
- Revenue Cycle Management Services
- Verification & Prior Authorization Services
Our team works with your practice to ensure each step of the cycle is handled efficiently. The result is faster payments, fewer errors, and a smoother experience for your team and your patients.
Conclusion
Medical billing cycle is the core of your revenue process. When every step is handled correctly, your practice stays profitable and your staff can focus more on patient care.
If you are dealing with frequent denials, late payments, or overwhelmed billing staff, it may be time to improve your workflow. Whether you need help with specific steps or full billing services, Pro-MBS is here to support you.